Aortic Dissection is a serious cardiovascular condition in which the walls of the aorta begin to separate from each other. It causes a tear through the aortic layers, leading to life-threatening complications.
What is Aortic Dissection?
This is an uncommon but clinically significant pathology of the aorta in which the layers of the aorta separate. It occurs in 30 out of 1 million Americans every year and poses a considerable health risk because of its high mortality rate.1Criado, F. J. (2011). Aortic dissection: a 250-year perspective. Texas Heart Institute Journal, 38(6), 694–700. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3233335
In order to understand this tearing of the aortic layers, it is important to understand the anatomy of the aorta. The aorta is the largest artery in your body and carries blood from the heart to the rest of the organs. It has the following parts and layers, which are implicated in aortic dissection:
| Parts of the Aorta | Layers of the Aorta |
| The ascending aorta is the part of the aorta that rises upward from the heart and towards the arch of the aorta. | The tunica externa or adventitia is the outermost layer of the aorta, which carries blood vessels and nerves. |
| The arch of the aorta is the curved vasculature that connects the ascending and descending aorta. | The tunica media is the central layer of the aorta. It changes the vessel diameter to accommodate changes in blood pressure and provides mechanical support. It also consists of numerous layers that lend it strength. |
| The descending aorta continues downwards from the arch of the aorta. | The tunica intima is the internal lining of the aorta, which provides a smoother surface for blood flow. |
How Does an Aortic Dissection Develop?
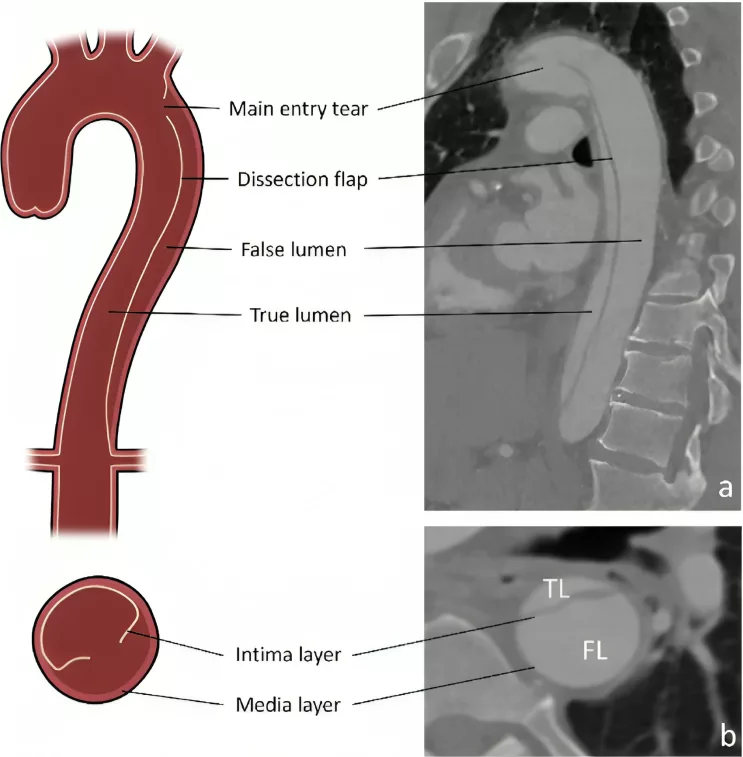
It refers to a split in the aorta. It usually starts in the tunica intima, a site that has undergone weakening due to various factors, such as stress and cardiovascular disease.
When the innermost layer has been torn, the high-pressure blood gushing through the aortic lumen enters the wall of the aorta and starts accumulating there. This accumulation causes heavy stress on the tunica media and causes its layers to separate, too.
In addition, this series of changes in the aortic wall structure leads to the formation of a “false lumen,” which compresses the actual lumen of the aorta. It greatly reduces and sometimes completely cuts off the blood supply to various organs in your body.2Sayed, A., Munir, M., & Bahbah, E. I. (2021). Aortic Dissection: A Review of the Pathophysiology, Management and Prospective Advances. Current Cardiology Reviews, 17(4). https://doi.org/10.2174/1573403×16666201014142930
Types of Aortic Dissection
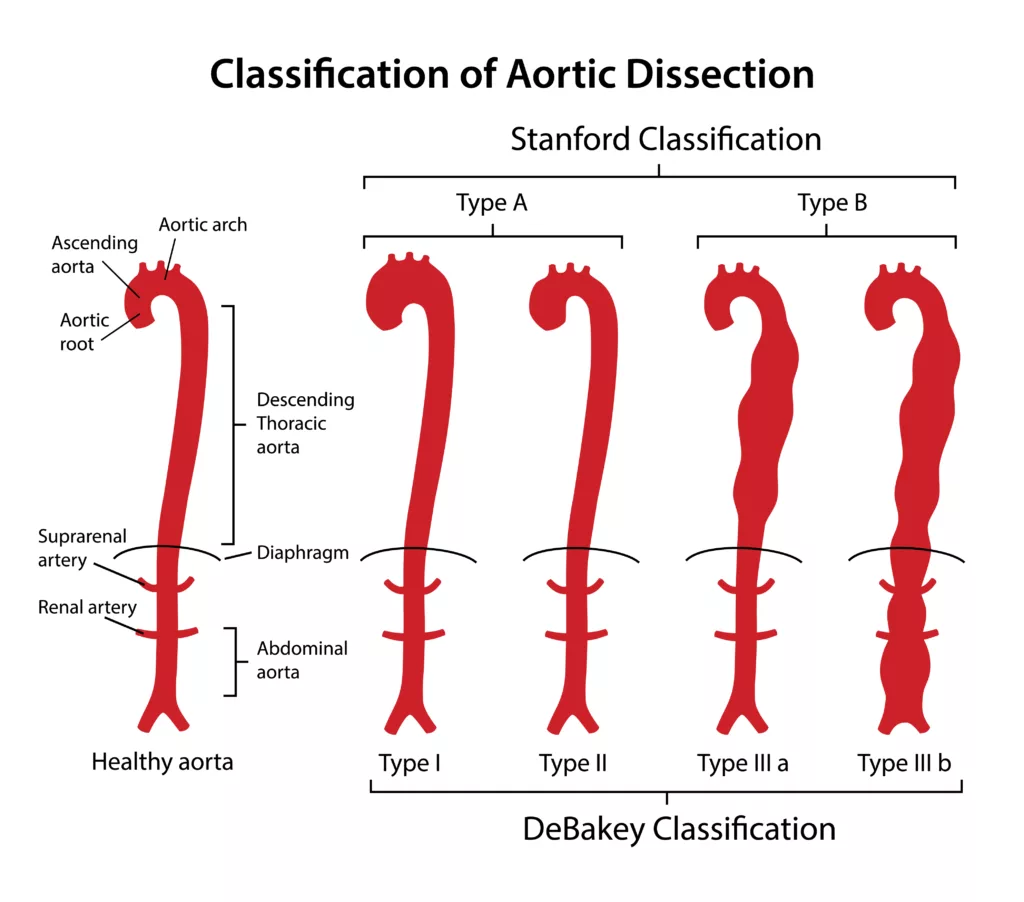
Aortic dissections have been classified anatomically based on which part of the aorta the tear occurs in. These classifications are important in estimating prognosis and determining the course of treatment.
The Stanford Classification
The Stanford classification is based on where the dissection occurs in relation to the ascending aorta.
| Type of Aortic Dissection | Description |
| Type A | When the aortic dissection involves the ascending aorta, it is classified as Type A. Since the ascending aorta is close to vital organs, it has a higher mortality rate and requires immediate surgical management. |
| Type B | When the aortic dissection starts further down in the descending aorta instead of involving the ascending aorta, it is classified as Type B. It is less life-threatening and usually does not require emergency surgery. |
The DeBakey Classification
The DeBakey classification is another classification that differentiates between aortic dissection, which requires surgery, and aortic dissection, which does not require immediate surgery for its management.3Aortic Dissection – Cardiovascular Disorders. (n.d.). MSD Manual Professional Edition. https://www.msdmanuals.com/professional/cardiovascular-disorders/diseases-of-the-aorta-and-its-branches/aortic-dissection
| Type of Aortic Dissection | Description |
| Type I
60% of cases |
Only the ascending and descending aorta are involved. It requires emergency surgery and is the most lethal type of aortic dissection. |
| Type II
10-15% of cases |
There is only the involvement of the ascending aorta. It may or may not require emergency surgery. |
| Type III
25-30% of cases |
Only the descending aorta is involved, and it does not require emergency surgery. |
Causes of Aortic Dissection
This is a result of various factors that result in increased biomechanical stress on the aorta and weaken its walls. These causes and risk factors include:
High Blood Pressure
High blood pressure is known as the most common cause of this condition, as over 70% of people who present with aortic dissection also have hypertension (high blood pressure). The risk for aortic dissection especially increases if your systolic blood pressure is over 132 mm Hg and diastolic blood pressure is over 75 mm Hg. Similarly, having a normal blood pressure is associated with a much lower risk of this condition. 4Makoto Hibino, Yoichiro Otaki, Kobeissi, E., Pan, H., Hiromi Hibino, Henock Taddese, Majeed, A., Verma, S., Tsuneo Konta, Yamagata, K., Fujimoto, S., Kazuhiko Tsuruya, Narita, I., Kasahara, M., Yugo Shibagaki, Kunitoshi Iseki, Moriyama, T., Kondo, M., Koichi Asahi, & Watanabe, T. (2022). Blood Pressure, Hypertension, and the Risk of Aortic Dissection Incidence and Mortality: Results From the J-SCH Study, the UK Biobank Study, and a Meta-Analysis of Cohort Studies. Circulation, 145(9), 633–644. https://doi.org/10.1161/circulationaha.121.056546
Congenital Abnormalities
A number of genetic conditions are associated with connective tissue and cardiovascular defects. They cause a weakening of the walls of various blood vessels, including the aorta. These disorders include:
- Marfan syndrome
- Loeys-Dietz syndrome
- Ehlers-Danlos syndrome, vascular type in particular
- Turner syndrome
- Familial thoracic aortic aneurysm and dissection syndrome
Heart Disease
Coronary artery disease has long been implicated in this condition. Conditions such as arteriosclerosis (narrowing of the blood vessels) and atherosclerosis (hardening of the blood vessels) cause great stress on the aorta and can result in sudden or chronic development of tears in its walls.
Family History
Around 20% of people who experience an aortic dissection or aortic aneurysm (especially in the thoracic aorta) are genetically predisposed to it.5Pinard, A., Jones, G. T., & Milewicz, D. M. (2019). Genetics of Thoracic and Abdominal Aortic Diseases. Circulation Research, 124(4), 588–606. https://doi.org/10.1161/circresaha.118.312436
Trauma
Sudden trauma because of blast or penetrating injuries during accidents, falls, and fighting can also result in this condition. However, traumatic aortic injuries like these are usually rare, as they constitute around 1-2% of the complaints patients present to trauma centers with.
Signs & Symptoms of Aortic Dissection
A typical patient with aortic dissection is a middle-aged or older male who may have a history of unmanaged hypertension or heart disease. They could also have a diagnosed genetic condition that affects their connective tissue. They are likely to present with the following signs and symptoms:
Pain
Pain is the most common and significant clinical hallmark of aortic dissection. The pain begins suddenly and is so severe that patients often call it the worst pain they have ever experienced. Pain often starts in the chest and radiates to:
- Back
- Arms
- Neck
- Jaw
- Between shoulders
- Scapula
The location of pain can help doctors determine what type of aortic dissection you have, especially if imaging modalities are not available at hand.
Cardiovascular Signs & Symptoms
The main signs and symptoms are cardiovascular and include:
- Abnormally high or low blood pressure
- Abnormal heart rate
- Weak or absent pulses in the limbs
- Murmurs
- Shortness of breath
- Fainting
- Shock
Non-cardiovascular Signs & Symptoms
In addition to cardiovascular signs and symptoms, there are several other features that can be seen in this condition:
- Neurological deficits are seen in around 20% of cases
o Confusion
o Weakness
o Numbness
o Difficulty talking - Hoarseness of voice due to compression of the recurrent laryngeal nerve
- Difficulty swallowing because of compression of the esophagus
- Nausea and vomiting
- Excessive sweating6Mancini, M. C. (2023, June 30). Aortic Dissection Clinical Presentation: History, Physical Examination, Complications. Medscape.com; Medscape. https://emedicine.medscape.com/article/2062452-clinical
Diagnosis of Aortic Dissection
This is a serious medical emergency that requires a quick clinical exam as well as imaging studies and laboratory investigation.
History & Physical Exam:
Your doctor will ask you if you are experiencing any pain. They will also ask you to describe and localize it. This condition is associated with a distinct type of continuous, burning pain, which is unlike any other condition. In addition, your doctor will run a quick physical exam to check for:
- Any differences in blood pressure between your arms
- Any drastic differences between your systolic and diastolic blood pressure
- Irregular heartbeat
- Irregular heart sounds or murmurs
- Any signs of shock
- Any inequalities or weaknesses in various pulses across your body
Laboratory Investigations:
A variety of baseline investigations are ordered while managing and diagnosing aortic dissection. They help rule out other causes of the signs and symptoms associated with the condition, as well as help your doctor establish the severity of the dissection:
- Full blood count — to check your body for infection and anemia
- Troponin levels — to rule out myocardial infarction
- Coagulation profile — to assess for clotting or bleeding disorders
- Renal function tests — to rule out renal damage
- Liver function tests — to rule out hepatic and mesenteric ischemia
- Serum electrolytes — to rule out fluid shifts and electrolyte imbalance
Imaging:
It is vital to perform emergency radiological investigations to confirm the diagnosis of this condition, even if your doctor has not yet received the results of lab Investigations. These modalities include:
Chest X-Ray
A simple chest X-ray can show a widened chest cavity or mediastinum, which occurs in at least 80% of the cases of aortic dissection. Abnormalities in the aortic arch may also be seen as a “knob” on the aorta.
CT Angiography
A computerized topographic angiography with contrast is considered the gold standard for diagnosing aortic dissection, as both its specificity and sensitivity are around 100%. The use of a contrast dye helps doctors visualize the actual extent of aortic dissection — the shape and size of the tear, where it is located, and the severity of the false lumen that has formed.
MRI
MRI scans are used to detect aortic dissection in patients who are allergic to contrast used in CT scans or have kidney disease. They give a detailed picture of the vasculature and structure of the aorta, as well as abnormalities of blood flow in the aortic lumen.
Transesophageal Echocardiography
Transesophageal echocardiography is used to diagnose this condition in unstable patients in an acute clinical setting. It can showcase where the flap from the tear is present, the presence of true and false lumens, and the extent of the dissection.7Levy, D., Goyal, A., Yulia Grigorova, Farci, F., & Le, J. K. (2023, April 23). Aortic Dissection. Nih.gov; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK441963/
How is Aortic Dissection Treated?
The treatment involves medication, surgery as well as lifestyle modification to prevent recurrence.
Immediate Management
If you have presented to the ER with aortic dissection, the priority for medical professionals will be to stabilize you. They will establish IV access to administer fluids and medication to you as soon as possible. In addition, they will start monitoring certain vital signs, including your blood pressure, heart rate, and oxygen saturation.
Pharmacologic Treatment
A variety of medications are used for the short-term and long-term treatment of this condition, such as:
Analgesics
Aortic dissection is associated with excruciating pain. Therefore, healthcare professionals immediately administer medications — mostly opioids — for rapid pain relief, such as:
- Morphine
- Fentanyl
- Hydromorphone
- Meperidine
Antihypertensives
The prognosis of aortic dissection can be rapidly improved by normalizing your blood pressure and reducing the stress on your aorta. Examples of blood pressure-lowering drugs include:
- Beta-blockers
o Labetalol
o Esmolol
o Metoprolol
o Propranolol - Calcium channel blockers
o Diltiazem
o Verapamil
o Nicardipine - Vasodilators
o Sodium nitroprusside
o Hydralazine
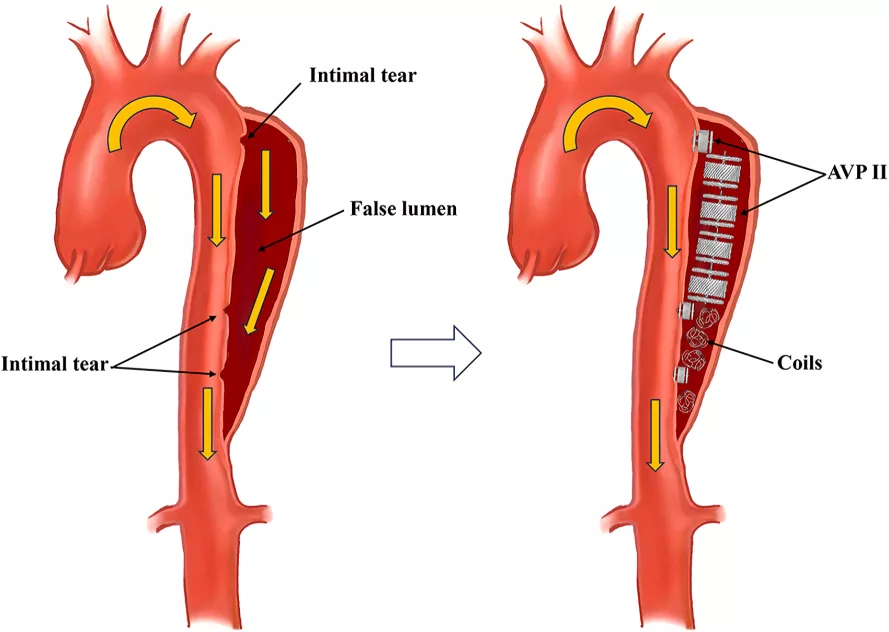
Surgical Treatment
Surgical treatment is lifesaving in patients with severe or complicated aortic dissection. Surgery often includes repair of the affected part of the aorta or its replacement with a graft.
Lifestyle Modifications
It is necessary to adopt a number of lifestyle modifications to prevent the recurrence of this condition. These include:
- Strictly managing your medical conditions, such as hypertension and hyperlipidemia
- Maintaining normal body weight
- Adopting a low-sodium diet
- Healthy eating
- Avoiding highly stressful environments
- Practicing stress reduction
Complications of Aortic Dissection
The aorta is the most important artery in the body, so aortic dissection can have devastating complications if it is not managed promptly. 30% of patients die before reaching the ER, and 20-30% die even after medical help. Complications include:
- Myocardial infarction
- Aortic rupture
- Pericardial tamponade
- Superior vena cava syndrome
- Horner’s syndrome 8Puttegowda B, Sharma R, Nagamani AC, Navin A, Basappa R, Manjunath NC. Interrupted aortic arch presenting as Horner’s syndrome: an unusual presentation. Heart Asia. 2013 Dec 16;5(1):260-2. doi: 10.1136/heartasia-2013-010446. PMID: 27547249; PMCID: PMC4987430.
Aortic Dissection Vs. Aneurysm
Aortic dissection and aortic aneurysm are both serious disorders of the aorta. The term “aortic dissection” refers to the tearing of the aortic wall, whereas “aortic aneurysm” refers to an abnormal dilation in the aorta, which causes it to balloon.
| Aortic Dissection | Aortic Aneurysm |
| Tear in the wall of the aorta | Abnormal enlargement of a part of the aorta |
| A sudden and severe onset | Gradual onset |
| Severe, tearing pain | Often unsymptomatic until rupture |
| Lower mortality | Higher mortality if ruptured |
Conclusion
Aortic dissection is an acute vascular disorder of the aorta, the largest artery in the human body. It causes a tear in the wall of the aorta, often starting at the innermost later. It has high mortality and needs to be managed as an emergency.
Refrences
- 1Criado, F. J. (2011). Aortic dissection: a 250-year perspective. Texas Heart Institute Journal, 38(6), 694–700. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3233335
- 2Sayed, A., Munir, M., & Bahbah, E. I. (2021). Aortic Dissection: A Review of the Pathophysiology, Management and Prospective Advances. Current Cardiology Reviews, 17(4). https://doi.org/10.2174/1573403×16666201014142930
- 3Aortic Dissection – Cardiovascular Disorders. (n.d.). MSD Manual Professional Edition. https://www.msdmanuals.com/professional/cardiovascular-disorders/diseases-of-the-aorta-and-its-branches/aortic-dissection
- 4Makoto Hibino, Yoichiro Otaki, Kobeissi, E., Pan, H., Hiromi Hibino, Henock Taddese, Majeed, A., Verma, S., Tsuneo Konta, Yamagata, K., Fujimoto, S., Kazuhiko Tsuruya, Narita, I., Kasahara, M., Yugo Shibagaki, Kunitoshi Iseki, Moriyama, T., Kondo, M., Koichi Asahi, & Watanabe, T. (2022). Blood Pressure, Hypertension, and the Risk of Aortic Dissection Incidence and Mortality: Results From the J-SCH Study, the UK Biobank Study, and a Meta-Analysis of Cohort Studies. Circulation, 145(9), 633–644. https://doi.org/10.1161/circulationaha.121.056546
- 5Pinard, A., Jones, G. T., & Milewicz, D. M. (2019). Genetics of Thoracic and Abdominal Aortic Diseases. Circulation Research, 124(4), 588–606. https://doi.org/10.1161/circresaha.118.312436
- 6Mancini, M. C. (2023, June 30). Aortic Dissection Clinical Presentation: History, Physical Examination, Complications. Medscape.com; Medscape. https://emedicine.medscape.com/article/2062452-clinical
- 7Levy, D., Goyal, A., Yulia Grigorova, Farci, F., & Le, J. K. (2023, April 23). Aortic Dissection. Nih.gov; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK441963/
- 8Puttegowda B, Sharma R, Nagamani AC, Navin A, Basappa R, Manjunath NC. Interrupted aortic arch presenting as Horner’s syndrome: an unusual presentation. Heart Asia. 2013 Dec 16;5(1):260-2. doi: 10.1136/heartasia-2013-010446. PMID: 27547249; PMCID: PMC4987430.