Powassan Virus (POWV) is a Flavivirus (a family of RNA viruses known for causing diseases like dengue, yellow fever, hepatitis C, etc.) transmitted by tick bites, i.e., arboviral infection. The virus causes Powassan virus disease in humans. It is a rare infectious disorder that generally causes mild symptoms such as fatigue, fever, confusion, seizures, etc. In rare instances, powassan virus infection can cause serious complications such as encephalitis.
Wildlife animals serve as reservoirs for the viral pathogen, proving to be a threat to domestic animals and humans. The disease is primarily found in regions of Canada, Russia, and the Northeastern United States. By 2012, there were only 200 reported cases of the Powassan virus in the US. However, according to reports by the CDC, there has been a surge in POWV cases in recent years, with the highest number of cases being reported in Minnesota.1Centers for Disease Control and Prevention. (n.d.). *Powassan virus disease cases by state*. Retrieved from [https://www.cdc.gov/powassan/data-maps/current-year-data.html](https://www.cdc.gov/powassan/data-maps/current-year-data.html) 11 cases of powassan virus were reported in Minnesota in 2024. No specific treatment is available for the powassan virus. Generally, management aims at alleviating symptoms.
Powassan Virus Disease Symptoms
In most cases, the powassan virus infection causes insignificant or mild symptoms. However, it can lead to grave consequences and long-term effects.
 The most prevalent symptoms of the disease include:
The most prevalent symptoms of the disease include:
Fever
A low-grade fever is a symptom common to most infectious disorders. As per studies, fever is the most common symptom of powassan virus disease, reported by 77% of the patients.2Kakoullis, L., Vaz, V. R., Kaur, D., Kakoulli, S., Panos, G., Chen, L. H., & Behlau, I. (2023). Powassan virus infections: a systematic review of published cases. Tropical Medicine and Infectious Disease, 8(12), 508.
Headache
The second most common symptom of this tick-borne disease is headache. More than half of patients experience headaches after the acute onset of the disease. Investigation of clinical cases revealed that the Flavivirus infection can cause headaches and severe neurological symptoms.3Raval, M., Singhal, M., Guerrero, D., & Alonto, A. (2012). Powassan virus infection: case series and literature review from a single institution. BMC research notes, 5, 1-6.
Fatigue
Clinical analyses show that most symptomatic individuals report muscle weakness and fatigue accompanied by acute onset of fever, nausea/vomiting, and tremors.4Johnson, D. K., Staples, J. E., Sotir, M. J., Warshauer, D. M., & Davis, J. P. (2010). Tickborne Powassan virus infections among Wisconsin residents. Wmj, 109(2), 91-97. Weakness, fatigue, and malaise are reported in around 30% of the cases.
Nausea And Vomiting
A nauseous feeling may be the primary indication of the disease. Many patients suffer from acute episodes of nausea and vomiting. According to a clinical report, an 82-year-old man reported a sudden onset of nausea and vomiting (accompanied by dizziness) after contracting the disease.5Piantadosi, A., Rubin, D. B., McQuillen, D. P., Hsu, L., Lederer, P. A., Ashbaugh, C. D., … & Lyons, J. L. (2016). Emerging cases of Powassan virus encephalitis in New England: clinical presentation, imaging, and review of the literature. Clinical Infectious Diseases, 62(6), 707-713. Experts believe nausea and vomiting may be associated with encephalitis.
Confusion & Dizziness
Confusion and dizziness make it to the list of the most common symptoms of powassan virus disease. Mostly, older patients experience an altered state of mind and get dizzy during the acute onset of the disease.6Kemenesi, G., & Bányai, K. (2018). Tick-borne flaviviruses, with a focus on the Powassan virus. Clinical microbiology reviews, 32(1), 10-1128.
Seizures & Paralysis
Powassan virus is known to cause neurological symptoms in patients. Oftentimes, seizures follow persistent headaches in older adults. The seizures can eventually lead to paralysis. According to a study, seizures are present in almost 8% of the reported cases of POWV.7Fareed, A., Rohail, S., Zameer, U., Wahid, A., Akhtar, S. M. M., & Masood, W. (2024). A comprehensive neurological perspective on tick-borne flaviviruses, with emphasis on Powassan virus. Therapeutic Advances in Infectious Disease, 11, 20499361241247470. Other neurological manifestations of the viral infection include cognitive and memory loss. Patients usually have slurred speech, face difficulty in balancing the body, and suffer from gait abnormalities.
Myalgias
The viral infection is also responsible for joint and muscle pains (myalgias). However, arthralgia and myalgia are reported in only 8% of the cases.
Powassan Virus Disease Long-term Effects & Complications
In most cases, powassan virus symptoms are mild. However, the virus does tend to impact the brain and cause serious long-term consequences. Though rare, long-term effects of powassan virus disease include:
Tick-Borne Encephalitis (TBE)
Neuroinvasion by the virus can prove fatal. The powassan virus’s involvement in the central nervous system can cause inflammation of the active brain tissues, i.e., encephalitis. Clinical studies reveal that encephalitis develops after an incubation period of 1-4 weeks. The most common symptoms are headache and fever, with alterations in mental status and paralysis (hemiplegia). The vast majority of POWV-induced encephalitis patients are seen in Minnesota and Wisconsin. Therefore, residents of these regions should be suspected of encephalitis if relevant symptoms are seen.8Birge, J., & Sonnesyn, S. (2012). Powassan virus encephalitis, Minnesota, USA. Emerging infectious diseases, 18(10), 1669.
Tick-borne encephalitis also caused a life-threatening condition in a 9-year-old resident of Canada. The young patient experienced persistent high fever and an ongoing severe headache. Symptoms developed one week after a camping trip to Ontario. By the third day of hospital administration, the patient was unresponsive and showed clear signs of neuroinvasion (by the virus). Immediate treatment saved the life of the young boy. Thus, it is imperative for doctors to provide immediate medical attention if tick-borne encephalitis is suspected.9Blatman, Z., Rowan-Legg, A., Schaffzin, J. K., Wilson, N., & Bechard, N. (2024). Powassan virus encephalitis in a 9-year-old. CMAJ, 196(28), E973-E976.
Meningoencephalitis
Entry of the powassan virus into the CNS can cause havoc. Patients may suffer from a combination of tick-borne encephalitis and viral meningitis. Meningitis is the inflammation (swelling) of the brain layers called meninges. This nervous system attack by the powassan virus can deteriorate the mental status of the patient and lead to grave consequences. The initial symptoms include fever, fatigue, and headache (occipital headache).10Pach, J. J., Zubair, A. S., Traner, C., Falcone, G. J., & Dewey, J. J. (2021). Powassan meningoencephalitis: a case report highlighting diagnosis and management. Cureus, 13(7). Neck stiffness is a typical symptom of meningitis. Encephalitis and meningoencephalitis can lead to permanent neurological damage. Both conditions are life-threatening and require emergency medical management.
How Does Powassan Virus Spread?
The main causative agent for the disease is the powassan virus. However, what’s important is the mode of transmission to humans. Bite from a specific type of infected tick i.e., Ixodes scapularis (aka deer tick or black-legged tick) causes transmission of the virus.11Eisen, R. J., & Eisen, L. (2018). The black-legged tick, Ixodes scapularis: an increasing public health concern. Trends in parasitology, 34(4), 295-309. Only 15 minutes of attachment (tick feeding) are sufficient for the transmission of the Powassan virus.
High-Risk Areas For Possawan Virus Spread
Clinicians have seen a rise in POWV cases during the past few years. The Great Lakes region of the Northeastern US, Canada, and Russia are home to different types of ticks.
 Thus, the highest number of tick-borne infections (such as Powassan virus disease) have been reported in:
Thus, the highest number of tick-borne infections (such as Powassan virus disease) have been reported in:
- Minnesota
- Wisconsin
- Massachusetts
- Connecticut
- New York
- New Jersey
- Maine
Powassan Virus Incubation Period
The incubation period for Powassan virus disease lies between one week and one month. Reports show that a typical powassan virus infection has a 7-34 day incubation period. After the incubation period, there is a prodrome phase characterized by fevers, chills, headache, fatigue/lethargy, nausea/vomiting, etc. This period lasts for about one to three days. Generally, it takes 1-4 weeks (after exposure) for symptoms to develop.12Kemenesi, G., & Bányai, K. (2018). Tick-borne flaviviruses, with a focus on the Powassan virus. Clinical microbiology reviews, 32(1), 10-1128.
Powassan Virus Disease Diagnosis
Diagnosing powassan virus disease is a little tricky because it is a rare disorder present only in tick-abundant areas. Healthcare providers working in such areas are aware of the situation and can reach a conclusive diagnosis sooner. The following steps/tests are important in POWV disease diagnosis:
History:
Healthcare providers usually will start with patient history. Your doctor will ask you questions regarding the onset of the symptoms (especially encephalitis). The provider might ask you if you remember having been bitten by a tick or if you have traveled to an area with the Powassan virus spread.
Tests/Studies:
Blood tests
Pathologists look for specific viral antigens in the serum. A blood test helps detect Powassan virus-specific antibodies (immunoglobulins), i.e., IgM antibodies in the serum. Mostly, an ELISA test is performed to detect the specific IgM antibodies.
CSF tests
A lumbar puncture (spinal tap) is performed to obtain the cerebrospinal fluid (CSF). Lab technicians look for virus-specific IgM antibodies in the CSF.
Immunocompromised patients may require molecular testing (additional testing) for an accurate diagnosis. This includes Immunohistochemistry (IHC) to detect Powassan virus antigen and RT-PCR test.
Radiographic Imaging:
CT scan
A computerized tomography scan of the brain plays an important role in diagnosing tick-borne encephalitis and meningoencephalitis.
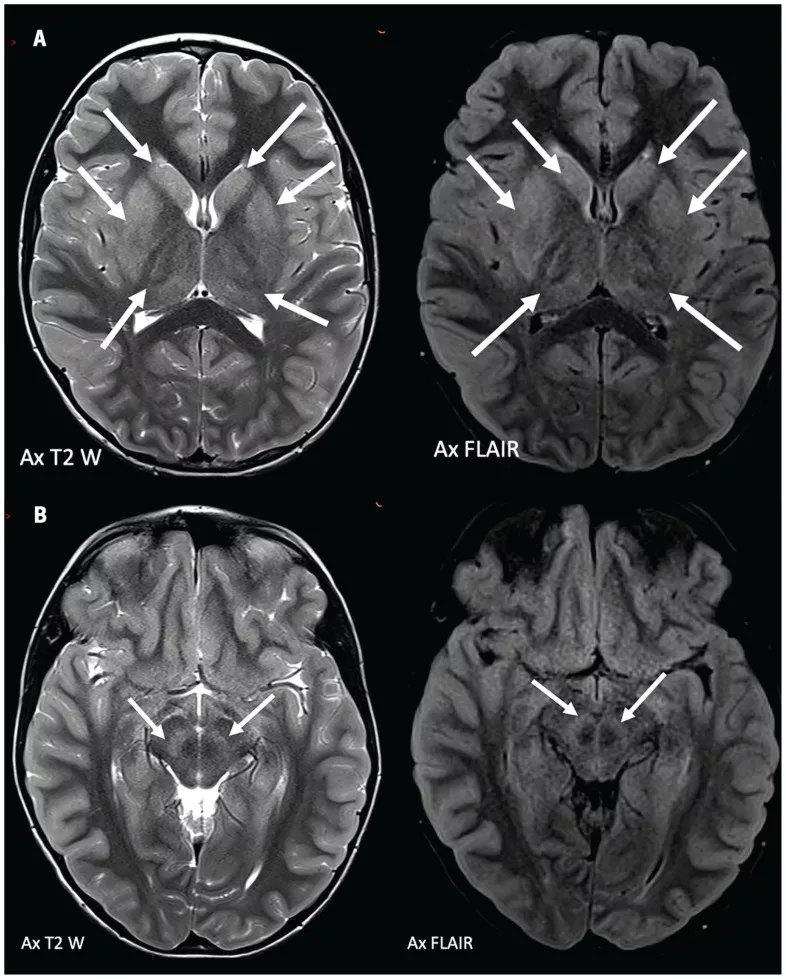
MRI scan
Doctors generally advise an MRI scan if the patient has neurological symptoms. A brain MRI plays an important role in detecting brain signal changes caused by encephalitis.
Relation With Lyme Disease
Lyme disease is a bacterial infection transmitted to humans through tick bite. Research shows that Powassan virus disease is highly prevalent in Lyme-endemic areas. Experts suggest that residents of the Midwest and Northeastern United States reporting altered state of mind and headaches should be screened for Powassan virus.13Bazer, D. A., Orwitz, M., Koroneos, N., Syritsyna, O., & Wirkowski, E. (2022). Powassan encephalitis: a case report from New York, USA. Case Reports in Neurological Medicine, 2022(1), 8630349.
Powassan Virus Disease Treatment
Unfortunately, there are no antiviral drugs available for Powassan virus infections. Thus, the main aim of the treatment is symptomatic management. For mild symptoms, the doctor advises rest, fluid intake, and over-the-counter painkillers to manage headaches.
Doctors advise different types of medicines to serious, hospitalized patients. Hospital management involves the provision of the following:
- Supplemental oxygen is given for respiratory support
- IV fluids keep the patient hydrated
- Corticosteroids are given to rapidly reduce brain swelling (in encephalitis and meningoencephalitis cases).14Hodzic, E., Hasbun, R., Granillo, A., Tröscher, A. R., Wagner, H., Von Oertzen, T. J., & Wagner, J. N. (2023). Steroids for the treatment of viral encephalitis: a systematic literature review and meta-analysis. Journal of Neurology, 270(7), 3603-3615.
- Antiemetic drugs are advised to alleviate feelings of nausea and vomiting.
Powassan Virus Prevention
Prevention from Powassan virus disease is possible if you take the necessary steps to keep ticks away. By using anti-tick sprays and cutting your grass short, you can limit the number of ticks in ticks in your surroundings. Wear full clothes during the peak season to avoid exposure.
Final Word
Powassan virus disease is a rare infectious disorder caused by a tick (Ixodex scapularis) bite. The disease causes fatigue, fever, altered mental status, headache, nausea/vomiting, and, in rare cases, encephalitis/meningoencephalitis. Encephalitis and meningoencephalitis can prove to be fatal, so they require immediate medical attention. It is common in areas of Northern America and Canada. The incubation period for the disease is one week to 1 month. Doctors detect antibodies in your serum/CSF for diagnosis. Currently, there are no anti-virals available for the disease, and doctors rely on symptomatic management only.
Refrences
- 1Centers for Disease Control and Prevention. (n.d.). *Powassan virus disease cases by state*. Retrieved from [https://www.cdc.gov/powassan/data-maps/current-year-data.html](https://www.cdc.gov/powassan/data-maps/current-year-data.html)
- 2Kakoullis, L., Vaz, V. R., Kaur, D., Kakoulli, S., Panos, G., Chen, L. H., & Behlau, I. (2023). Powassan virus infections: a systematic review of published cases. Tropical Medicine and Infectious Disease, 8(12), 508.
- 3Raval, M., Singhal, M., Guerrero, D., & Alonto, A. (2012). Powassan virus infection: case series and literature review from a single institution. BMC research notes, 5, 1-6.
- 4Johnson, D. K., Staples, J. E., Sotir, M. J., Warshauer, D. M., & Davis, J. P. (2010). Tickborne Powassan virus infections among Wisconsin residents. Wmj, 109(2), 91-97.
- 5Piantadosi, A., Rubin, D. B., McQuillen, D. P., Hsu, L., Lederer, P. A., Ashbaugh, C. D., … & Lyons, J. L. (2016). Emerging cases of Powassan virus encephalitis in New England: clinical presentation, imaging, and review of the literature. Clinical Infectious Diseases, 62(6), 707-713.
- 6Kemenesi, G., & Bányai, K. (2018). Tick-borne flaviviruses, with a focus on the Powassan virus. Clinical microbiology reviews, 32(1), 10-1128.
- 7Fareed, A., Rohail, S., Zameer, U., Wahid, A., Akhtar, S. M. M., & Masood, W. (2024). A comprehensive neurological perspective on tick-borne flaviviruses, with emphasis on Powassan virus. Therapeutic Advances in Infectious Disease, 11, 20499361241247470.
- 8Birge, J., & Sonnesyn, S. (2012). Powassan virus encephalitis, Minnesota, USA. Emerging infectious diseases, 18(10), 1669.
- 9Blatman, Z., Rowan-Legg, A., Schaffzin, J. K., Wilson, N., & Bechard, N. (2024). Powassan virus encephalitis in a 9-year-old. CMAJ, 196(28), E973-E976.
- 10Pach, J. J., Zubair, A. S., Traner, C., Falcone, G. J., & Dewey, J. J. (2021). Powassan meningoencephalitis: a case report highlighting diagnosis and management. Cureus, 13(7).
- 11Eisen, R. J., & Eisen, L. (2018). The black-legged tick, Ixodes scapularis: an increasing public health concern. Trends in parasitology, 34(4), 295-309.
- 12Kemenesi, G., & Bányai, K. (2018). Tick-borne flaviviruses, with a focus on the Powassan virus. Clinical microbiology reviews, 32(1), 10-1128.
- 13Bazer, D. A., Orwitz, M., Koroneos, N., Syritsyna, O., & Wirkowski, E. (2022). Powassan encephalitis: a case report from New York, USA. Case Reports in Neurological Medicine, 2022(1), 8630349.
- 14Hodzic, E., Hasbun, R., Granillo, A., Tröscher, A. R., Wagner, H., Von Oertzen, T. J., & Wagner, J. N. (2023). Steroids for the treatment of viral encephalitis: a systematic literature review and meta-analysis. Journal of Neurology, 270(7), 3603-3615.