Atrophic vaginitis refers to the inflammatory process of the vagina characterized by thinning and drying of the vaginal epithelium. It commonly occurs in some pre-menopausal and up to 50% of postmenopausal women1Flores, S.A. and Hall, C.A. (2022) Atrophic vaginitis, Statpearls [Internet]. Retrieved 22 July 2023 from https://www.ncbi.nlm.nih.gov/books/NBK143764/. Vaginal atrophy occurs after menopause due to a decline in body estrogen. This condition and other symptoms of menopause are collectively termed Genitourinary Syndrome of Menopause (GSM).
Causes of Atrophic Vaginitis
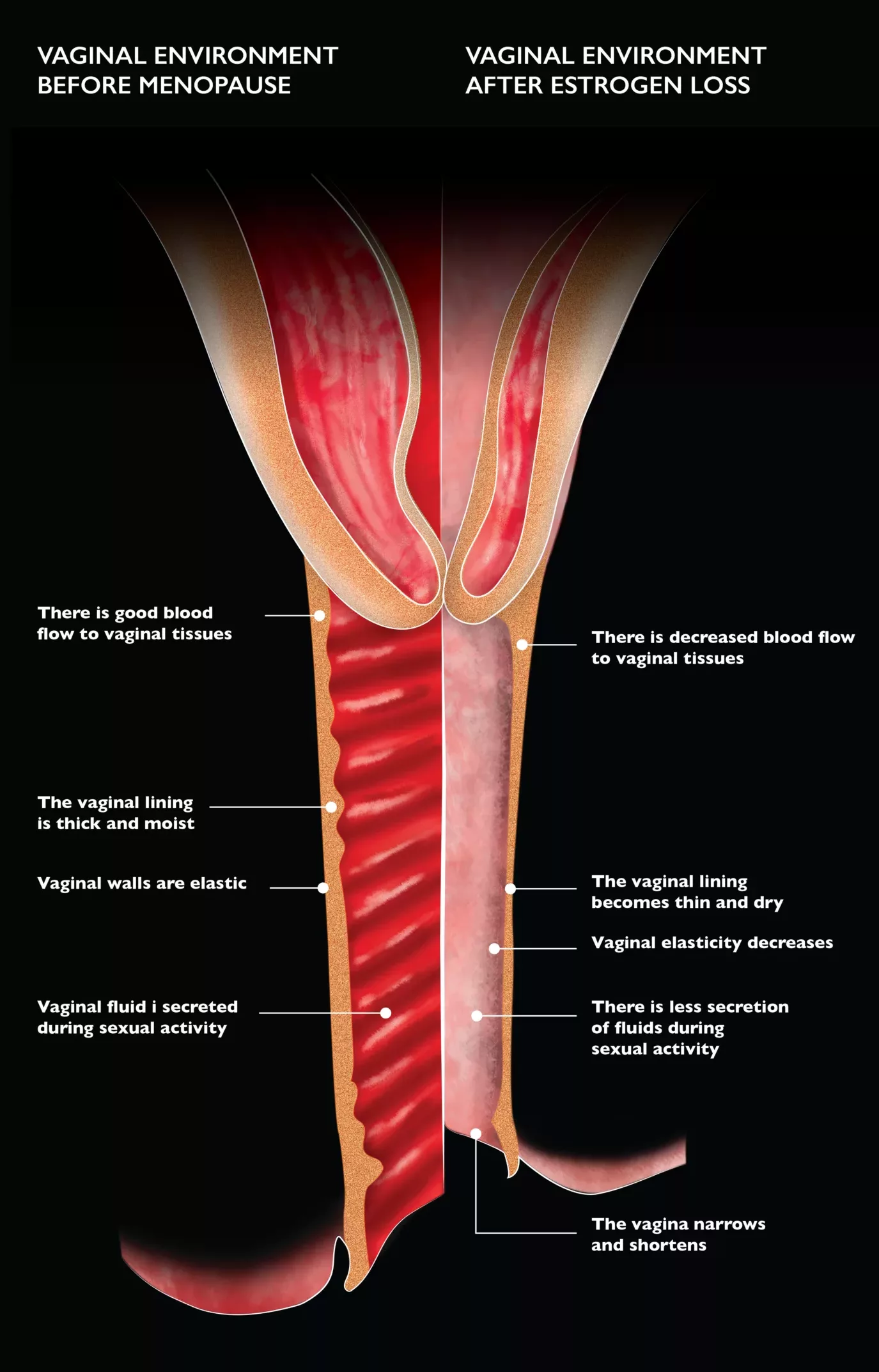
The most common cause of atrophic vaginitis is decreased production of estrogen. Low estrogen levels make your vaginal wall thin and less elastic. Also, it leads to the shortening and narrowing of the vagina. Less estrogen disturbs the pH and fluid balance of the vagina, which makes it dry and more susceptible to irritation.
A reduction in estrogen level may be due to one of the following causes:
- Menopause: It may occur in years advancing to menopause or after menopause when estrogen production declines.
- During Breastfeeding: Breastfeeding women have increased levels of prolactin in the body. Prolactin counters the production of estrogen, which leads to vaginal thinning.
- Medications: Contraceptives and Antiestrogenic medicines such as Tamoxifen and Medroxyprogesterone cause vaginal dryness.
- Surgical Removal of Ovaries: Ovaries are responsible for most estrogen production. Removal of ovaries causes diminished estrogen that leads to symptoms of atrophic vaginitis.
- Chemotherapy: Some chemotherapeutic drugs might damage ovaries2Hormone therapy for breast cancer: Breast cancer treatment (2023) Breast Cancer Treatment | American Cancer Society. Retrieved 01 August 2023 from https://www.cancer.org/cancer/types/breast-cancer/treatment/hormone-therapy-for-breast-cancer. Damaged ovaries produce insufficient estrogen that causes vaginal dryness.
- Adverse effect of Hormonal Therapy for Breast Cancer: Breast cancer treatment involves anti-estrogen medicines that block estrogen production in the body. This reduces vaginal elasticity and causes dryness.
- Treatment of Pelvic Area: Pelvic radiation therapy causes vaginal stenosis and adversely affects life quality. It may cause vaginal dryness and dyspareunia3Varytė, G. and Bartkevičienė, D. (2021) Pelvic radiation therapy induced vaginal stenosis: A review of current modalities and recent treatment advances, Medicina (Kaunas, Lithuania). Retrieved 01 August 2023 from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8066324.
- Uncontrolled Diabetes: High blood glucose levels damage the vaginal blood vessels. It causes less lubrication and increased dryness of the vagina.
Symptoms of Atrophic Vaginitis
The primary symptoms of atrophic vaginitis are:
- Vaginal dryness
- Burning or itching
- Atypical vaginal discharge (yellow)
- Dyspareunia (pain during sex)
- Itching around vulva
- Bleeding or spotting
- Occurrence of urinary tract infections (UTIs)
- Urinary incontinence
Pathophysiology
Estrogen receptors are present primarily in the uterus and ovary. Estrogen is responsible for the adequate growth and development of vaginal epithelium. Decreased estrogen production causes fragmentation of elastin fibers that causes loss of elasticity of vaginal tissue. The collagen fibers fuse, and squamous cells decrease in number and cause the narrowing of the vagina with loss of rugae. This also leads to thinning of the vaginal walls, reduced blood flow, and altered vaginal microbiome.
When to See a Doctor?
Many find it embarrassing to discuss symptoms of vaginal atrophy with a healthcare provider. However, seeking appropriate medical assistance can help relieve symptoms and improve quality of life.
Consult your doctor if you notice unusual bleeding, vaginal discharge, itching, or burning. Painful sexual intercourse also indicates atrophic vaginitis if it does not go away with vaginal moisturizers or lubricants.
How to Diagnose Atrophic Vaginitis?
Diagnosis is based on your medical history, symptoms, and pelvic examination.
The doctor may ask about your age, other menopausal symptoms, and the use of vaginal irritants. They may examine the pelvic region to look for the signs of atrophy, such as redness, dryness, swelling, loss of elasticity, narrowing and shortening of the vaginal canal.
The examination can be painful if vaginal atrophy occurs. Diagnosis is confirmed after the following test:
Hormonal Testing:
Serum hormone concentration, i.e., low levels of circulating Estrogen (less than or equal to 4.5), indicates atrophic vaginitis.4Pandit L, Ouslander JG. Postmenopausal vaginal atrophy and atrophic vaginitis. Am J Med Sci 1997;314:228–31, and Osmers R, Volksen M, Schauer A. Vaginosonography for early detection of endometrial carcinoma? Lancet 1990;335:1569–71.
Acid Balance Test:
The doctor checks vaginal pH using a paper strip. pH greater than five shows atrophic vaginitis5Bachmann, G.A. and Nevadunsky, N.S. (2000) Diagnosis and treatment of atrophic vaginitis, American Family Physician. Retrieved 22 July 2023 from https://www.aafp.org/pubs/afp/issues/2000/0515/p3090.html#afp20000515p3090-b3 (normal vaginal pH is 4.5).
Urine Test:
Your doctor recommends this test if you face issues with urination, e.g., urinary incontinence, urinary tract infection (UTI)
Infection Screening:
Your healthcare provider may advise an infection screening for discharge and bleeding. Atrophic vaginitis puts the vagina at a greater risk of infections, e.g., bacterial vaginosis, candidiasis, and endometritis6Wilson, D.R. (ed.) (2018) Atrophic vaginitis: Symptoms, causes, and treatments, Medical News Today. Retrieved 21 July 2023 from https://www.medicalnewstoday.com/articles/189406#diagnosis.
Endometrial Biopsy:
Bleeding after sexual intercourse is a sign of endometrial cancer. The doctor may perform a biopsy to rule out malignancy. They remove a piece of tissue from the uterine wall and examine it in the laboratory.
Pap test:
Pap smear (named after Dr George Papanicolaou) is a common tool for screening cervical cancer. Cytologic examination of smears from the upper one-third of the vagina shows an increased proportion of parabasal cells and a decreased percentage of superficial cells.
Ultrasonography:
A vaginal ultrasonogram of the uterine lining that demonstrates a thin endometrium measuring between 4 and 5 mm signifies loss of adequate estrogenic stimulation.7Botsis D, Kassanos D, Kalogirou D, Antoniou G, Vitoratos N, Karakitsos P. Vaginal ultrasound of the endometrium in postmenopausal women with symptoms of urogenital atrophy on low-dose estrogen or tibolone treatment: a comparison. Maturitas. 1997 Jan;26(1):57-62. doi: 10.1016/s0378-5122(96)01070-5. PMID: 9032748.
Atrophic Vaginitis Prevention
Atrophic vaginitis is part of the natural aging process. However, one can prevent its progression through appropriate measures.
- Frequent sexual activity increases blood flow to the vagina which helps prevent dryness and itching.
- Avoid perfumes, soaps, lotions, etc., that irritate vaginal epithelium.
- Exercise regularly to improve blood circulation in the genitalia.
- Avoid wearing tight clothes
Atrophic Vaginitis Treatment
Various treatment options are available, from non-prescription moisturizers to hormone replacement therapy. Women can get along with mild symptoms using moisturizers and vaginal lubricants to relieve itching and dryness in the vagina.
If the symptoms persist, you should seek medical assistance. Your physician may recommend other treatment options like estrogen creams or hormonal therapy. Here is an account of treatment options:
Steroids for Atrophic Vaginitis (Hormone Replacement Therapy)
Estrogen Replacement Therapy is the main treatment regimen for vaginal atrophy. Local estrogen treatment relieves symptoms of atrophic vaginitis in 80-90% of patients. In comparison, systemic therapy does so in 75% of patients8Wilson, D.R. (ed.) (2018) Atrophic vaginitis: Symptoms, causes, and treatments, Medical News Today. Retrieved 21 July 2023 from https://www.medicalnewstoday.com/articles/189406#diagnosis. Topical preparations relieve vaginal dryness, while those meant for systemic use increase the overall estrogen levels in the body.
Topical Estrogen
These formulations are available as pills, patches, creams, etc. Local administration of these estradiol-based products treats symptoms of atrophy by restoring vaginal thickness, secretions, flora, and pH. However, it does not increase estrogen levels in the body. Your doctor may discuss and recommend a therapy that suits your condition.
- Vaginal Estrogen Cream: You have to apply this cream inside your vagina with an applicator. You may use it daily for some weeks and then twice or thrice weekly. Otherwise, follow your doctor’s instructions while using it.
- Vaginal Ring: Your physician will place a thin, flexible ring in the vagina that releases estrogen. It remains there for three months and then replaced with a new one.
- Vaginal Tablet: Place a small tablet in the vagina that releases estrogen daily. After several weeks, use it twice or thrice a week.
Systemic Hormone Replacement Therapy
This approach proves beneficial when patients exhibit additional menopausal symptoms, especially hot flashes. It involves utilizing formulations that encompass estradiol and conjugated estrogens, effectively enhancing both vaginal well-being and overall quality of life. The therapy introduces estrogen directly into the bloodstream, ensuring its distribution throughout the entire body. However, it’s essential to acknowledge the potential drawbacks, as it might exert adverse effects on the endometrium and breast tissue.
Non-Hormonal Treatment Options
Although estrogen therapy is the primary treatment for atrophy, other options are available. Other therapies are considered when a patient presents combined symptoms of GSM.
The following are the most commonly employed treatments besides steroids:
- Vaginal Moisturizers
Vaginal moisturizers are water-based products that attach to the vaginal wall and release water to make a moist film. These are good options to eliminate vaginal dryness, one of the primary symptoms of atrophic vaginitis. Some of them also maintain the acid-base balance of the vagina. Moisturizers effectively treat symptoms of atrophic vaginitis. - Vaginal Lubricants
It’s good to use before intercourse if you have pain during sex. These products have a smooth, clear consistency similar to vaginal secretions. Vaginal lubricants are water, oil, or silicone-based products with a neutral pH so they do not irritate. Astroglide, for example, is a common lubricant with the above-mentioned properties. - Laser Treatment
Laser treatment causes revascularization of vagina tissue. It also increases the thickness of the vaginal epithelium, stimulating collagen synthesis that restores tissue elasticity. Overall, it improves the symptoms of atrophy by restoring vaginal anatomy and physiology
Atrophic Vaginitis Vs. Lichen Sclerosus
Atrophic vaginitis may seem like lichen sclerosus, but the two conditions are completely different. Lichen sclerosus is a discolored, erratic, and thin skin in the genital area due to an unknown cause. The primary cause of atrophic vaginitis is vaginal thinning due to a lack of estrogen. Atrophic vaginitis occurs in the post-menopausal population, but lichen sclerosus may occur at a young age, though common after menopause.
Physical examination reveals a friable, red, and thin vulvovaginal area with loss of rugae and abnormal anatomy in atrophic vaginitis. Lichen sclerosus is restricted to labia with a thin, white epithelium and loss of vaginal framework. Estrogen therapy effectively cures atrophic vaginitis, while topical corticosteroids can treat lichen sclerosus.
The Bottom Line
Atrophic vaginitis is not life-threatening but may worsen if not treated properly. It affects your quality of life with a greater risk of infections, discomfort, and urinary problems. Multiple treatment options are available that help restore vaginal anatomy and alleviate symptoms. Don’t hesitate to consult a physician and seek appropriate treatment for your condition.
Refrences
- 1Flores, S.A. and Hall, C.A. (2022) Atrophic vaginitis, Statpearls [Internet]. Retrieved 22 July 2023 from https://www.ncbi.nlm.nih.gov/books/NBK143764/
- 2Hormone therapy for breast cancer: Breast cancer treatment (2023) Breast Cancer Treatment | American Cancer Society. Retrieved 01 August 2023 from https://www.cancer.org/cancer/types/breast-cancer/treatment/hormone-therapy-for-breast-cancer
- 3Varytė, G. and Bartkevičienė, D. (2021) Pelvic radiation therapy induced vaginal stenosis: A review of current modalities and recent treatment advances, Medicina (Kaunas, Lithuania). Retrieved 01 August 2023 from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8066324
- 4Pandit L, Ouslander JG. Postmenopausal vaginal atrophy and atrophic vaginitis. Am J Med Sci 1997;314:228–31, and Osmers R, Volksen M, Schauer A. Vaginosonography for early detection of endometrial carcinoma? Lancet 1990;335:1569–71.
- 5Bachmann, G.A. and Nevadunsky, N.S. (2000) Diagnosis and treatment of atrophic vaginitis, American Family Physician. Retrieved 22 July 2023 from https://www.aafp.org/pubs/afp/issues/2000/0515/p3090.html#afp20000515p3090-b3
- 6Wilson, D.R. (ed.) (2018) Atrophic vaginitis: Symptoms, causes, and treatments, Medical News Today. Retrieved 21 July 2023 from https://www.medicalnewstoday.com/articles/189406#diagnosis
- 7Botsis D, Kassanos D, Kalogirou D, Antoniou G, Vitoratos N, Karakitsos P. Vaginal ultrasound of the endometrium in postmenopausal women with symptoms of urogenital atrophy on low-dose estrogen or tibolone treatment: a comparison. Maturitas. 1997 Jan;26(1):57-62. doi: 10.1016/s0378-5122(96)01070-5. PMID: 9032748.
- 8Wilson, D.R. (ed.) (2018) Atrophic vaginitis: Symptoms, causes, and treatments, Medical News Today. Retrieved 21 July 2023 from https://www.medicalnewstoday.com/articles/189406#diagnosis

