Babesiosis is an acute health-threatening parasitic disease that targets the red blood cells. It is caused by intraerythrocytic parasites belonging to the Babesia genus. These parasites are transmitted primarily through the bite of infected Ixodes ticks. While Babesia is a significant blood parasite, malaria caused by Plasmodium species remains the most prevalent globally. Another name for babesiosis, particularly in veterinary contexts, is “red water fever,” a term referring to the hemoglobinuria seen in infected livestock. The disease is a notable cause of economic loss in regions where livestock is heavily affected.1Cook MJ, Puri BK. Babesiosis: Analysis of the Evidence for Infections in the United Kingdom. International Journal of General Medicine. 2024:4627-31.
Babesiosis is also recognized as an emerging zoonotic disease in humans, raising increasing public health awareness. Transmission can occur not only through tick bites but also via blood transfusion and, in rare cases, from mother to fetus. Common symptoms in humans include fever, chills, fatigue, and headache, while severe cases may involve complications such as acute respiratory distress syndrome (ARDS), hemolytic anemia, and multi-organ failure, necessitating hospitalization.2Homer MJ, Aguilar-Delfin I, Telford III SR, Krause PJ, Persing DH. Babesiosis. Clinical microbiology reviews. 2000;13(3):451-69.3Vannier E, Krause PJ. Babesiosis. Hunter’s tropical medicine and emerging infectious diseases. 2020:799-802.
Life Cycle of the Babesia
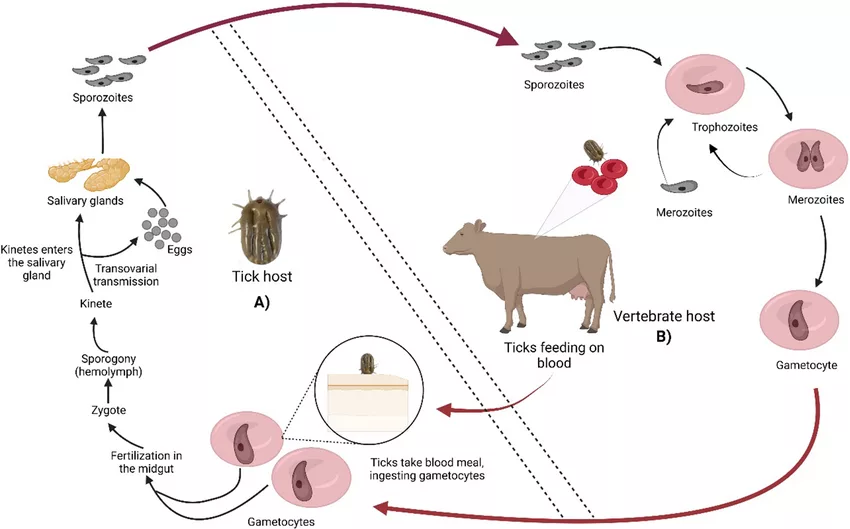
The life cycle of Babesia requires two hosts: a definitive invertebrate host (ticks) and an intermediate vertebrate host (humans, rodents, or other animals).
Infection
The life cycle begins when an infected tick feeds on the vertebrate host. During this feed, the ticks transmit Babesia into the host’s bloodstream.
Asexual Reproduction in Vertebrates
Inside the vertebrate host, the parasite invades the erythrocytes through sporozoites excreted in the tick’s saliva. In the erythrocytes, the parasites multiply asexually. The sporozoites develop into trophozoites. This asexual multiplication is named merogamy. The asexual reproduction ends in the formation of merozoites or gametocytes. Merozoites can infect the neighboring red blood cells, and gametocytes develop into gametes.
Sexual Reproduction in invertebrates
The infected vertebrate host serves as a source of Babesia for ticks. When ticks feed on the infected host, they ingest the parasites. The ingested parasites undergo sexual reproduction in the ticks. Sexual reproduction is also called gamogony. Ticks have a four-stage life cycle: egg, larva, nymph, and adult. Each stage requires a blood meal from a different host to advance to the next stage.
Transmission to a New Host
As the ticks bite new hosts, they transmit the parasite again, and the cycle continues. Human infections usually occur during late summer and spring when the tick population is highest.4Bonnet SI, Nadal C. Experimental infection of ticks: An essential tool for the analysis of Babesia species biology and transmission. Pathogens. 2021;10(11):1403.
Causes & Transmission of Bebesiosis
Babesia spp. is the causative agent of this infection. Most of the Babesia are pear-shaped, oval or round, and small (1-5 mm long). This zoonotic disease requires hard tick vectors for its transmission.5Oz HS, Westlund KH. “Human babesiosis”: an emerging transfusion dilemma. International journal of hepatology. 2012;2012(1):431761.
The most common Babesia species causing human babesiosis include:
- Babesia microti: Endemic in the upper Midwest and northeastern United States.
- Babesia divergens: Common in Europe, often affecting splenectomized or immunocompromised individuals.
- Babesia duncani: Found along the Pacific coast of the United States.
- Babesia crassa: Predominantly seen in China.
- Babesia venatorum: Present in both Europe and China.6Vannier E, Krause PJ. Babesiosis. Hunter’s tropical medicine and emerging infectious diseases. 2020:799-802.
Over 100 Babesia species are known to infect domestic and wild animals, causing significant economic losses in livestock. Common examples include:
- Babesia bovis, B. major, and B. divergens: Affect cattle and lead to anemia, fever, and reduced productivity.
- Babesia canis: Infects dogs.
- Babesia caballi: Infects horses.
- Babesia odocoilei: Found in deer.
- Babesia microti: Common in rodents.
- Babesia felis: Infects cats.7Krause PJ. Human babesiosis. International journal for parasitology. 2019;49(2):165-74.
Modes of Transmission
Babesiosis cannot be transmitted from one person to another. Babesia spp. are hemoprotozoan parasites that are transmitted through:
Bites of Ticks
The most common mode of transmission is through the bite of infected hard ticks, primarily Ixodes scapularis (deer tick) in the United States and Ixodes ricinus in Europe. Ticks become infected during blood meals from parasitized hosts and transmit the parasite during subsequent feedings.8Oz HS, Westlund KH. “Human babesiosis”: an emerging transfusion dilemma. International journal of hepatology. 2012;2012(1):431761.
Congenital Transmission
Infected mothers can also pass the infection to their babies during pregnancy.
Blood Transfusions
Transfusion of contaminated blood products, such as red blood cells, whole blood-derived platelets, or frozen deglycerolized blood cells, is also the transmission source of babesiosis.
Organ Transplant
Rarely, babesiosis has been transmitted through solid organ transplants.9Oz HS, Westlund KH. “Human babesiosis”: an emerging transfusion dilemma. International journal of hepatology. 2012;2012(1):431761.
Pathogenesis of the Babesia
The pathogenesis of Babesia involves its lifecycle within the host’s red blood cells, leading to significant cellular and systemic effects.
After being deposited in the dermis by an infected tick, Babesia sporozoites enter the bloodstream and invade red blood cells (erythrocytes). Once inside, the parasitophorous vacuole membrane surrounding the parasite dissolves, allowing free access to the host cell’s contents. The free sporozoites differentiate into trophozoites. The trophozoites eventually undergo binary fission. It generates two to four merozoites. The merozoites make a way out to trigger the cell lysis in the host, thus causing anemia. Anemia also occurs from the suppression of erythropoiesis and clearance of uninfected erythrocytes. Additionally, inflammatory cytokines also play a role in the formation of acute cytokines. The resolution of parasitemia necessitates intact adaptive and immune responses. Autoantibodies produced during parasite clearance can amplify prolonged anemia or thrombocytopenia.10Vannier E, Krause PJ. Babesiosis. Hunter’s tropical medicine and emerging infectious diseases. 2020:799-802.
Symptoms of Babesiosis
The clinical manifestations of this condition usually range from asymptomatic infection to critical disorder that can cause death. Symptoms appear after an incubation period of one to four weeks after a bite from an infected tick. After one to nine months after the blood transfusion, the patients experience a gradual onset of fatigue and malaise in addition to other symptoms.
Common Symptoms
The most common manifestations include:
- Fatigue
- A very high fever (104 F)
- Sweats
- Chills
- Anorexia
- Myalgia
- Headache
Less Common Symptoms
These include:
- Depression
- Emotional liability
- Arthralgia
- Abdominal pain
- Sore throat
- Neck stiffness
- Nausea
- Hyperesthesia
- Vomiting
- Shortness of breath
- Conjunctival infection
- Weight loss
- Photophobia
- Non-productive cough
- Hyperesthesia
Laboratory Findings
Other laboratory abnormalities involve:
- Elevated levels of liver enzymes,
- Elevated reticulocyte count
- Severe Hemolytic anemia
- Thrombocytopenia
- Elevated blood urea
- Elevated creatinine levels
- Proteinuria
Physical Findings
Physical abnormalities may involve:
- Pallor
- Jaundice
- Hepatomegaly
- Splenomegaly
People with malignancy, AIDS/HIV, neonatal prematurity, immunosuppressive therapy, asplenia, immunosuppressive therapy, liver, hematologic, or cardiac comorbidities experience severe symptoms. The most severe complications that can arise in these patients are:
- Renal failure
- Hemophagocytic lymphohistiocytosis
- Disseminated intravascular coagulation
- Acute respiratory distress syndrome (ARDS)
- Congestive heart failure
- Severe anemia
- Splenic rupture11Krause PJ. Human babesiosis. International journal for parasitology. 2019;49(2):165-74.
Diagnosis of Babesiosis
Diagnosing babesiosis involves a combination of clinical evaluations, epidemiological factors, and laboratory testing. The primary methods for diagnosing babesiosis include microscopic examination, serology, and molecular techniques.
Symptomatic Evaluation:
The healthcare providers will first look at the symptoms of the condition. The diagnosis should also consider risk factors such as recent travel to endemic areas and exposure to ticks. Fever is the most common finding in a physical exam. The skin can be yellowish or pale. Tenderness in the abdomen, usually at the upper left quadrant, suggests splenomegaly. Unexplained splenomegaly or abdominal pain with increased heart rate raises the possibility of hemoperitoneum and splenic rupture. An erythematous skin lesion is also suggestive of concurrent Lyme disease. Jaundice can also be observed due to petechiae, disseminated intravascular coagulopathy, or hemolysis.12Vannier E, Krause PJ. Babesiosis. Hunter’s tropical medicine and emerging infectious diseases. 2020:799-802.
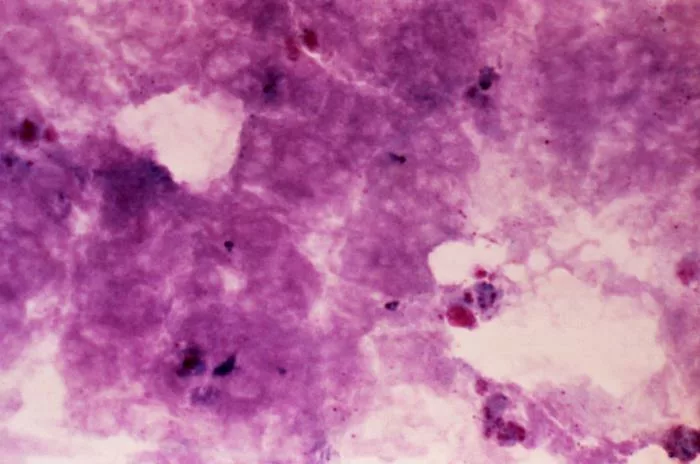
Microscopic Examination:
A more definitive diagnosis can be made through microscopic examination of the Giemsa-stained blood smears. The provider smears a blood sample on a slide, airs dry it, fixes it in methanol, and then stains it. The stained slides are then examined under high magnification (100x oil immersion lens) to detect the presence of Babesia spp. in the erythrocytes. Thin smears provide better morphological details for identifying the parasites. The Babesia trophozoites appear in ring forms, while merozoites often appear pear-shaped and can also be arranged in a tetrad. Thick smears are also informative, but as these parasites are small, they can be missed.13Karasová M, Tóthová C, Grelová S, Fialkovičová M. The etiology, incidence, pathogenesis, diagnostics, and treatment of canine babesiosis caused by Babesia gibsoni infection. Animals. 2022;12(6):739.
Laboratory Tests:
Some routine laboratory tests can help in diagnosing the condition. These tests include:
Complete Blood Count (CBC)
A complete CBC will reveal low hematocrit, low hemoglobin, an elevated reticulocyte, a low platelet count, and a low red blood cell count. Elevated lactate dehydrogenase and low haptoglobin levels are consistent with hemolytic anemia. Neutropenia also occurs in some patients. The leukocyte count is usually normal to slightly decreased. However, in severe cases, the examiner may also observe elevated bilirubin and liver enzymes.14Krause PJ. Human babesiosis. International journal for parasitology. 2019;49(2):165-74.
Urinalysis
The presence of hematuria, proteinuria, hemoglobinuria, and excessive urobilinogen will confirm the infection. Additionally, the high levels of serum creatinine and urea nitrogen will also indicate renal compromise.15Vannier E, Krause PJ. Babesiosis. Hunter’s tropical medicine and emerging infectious diseases. 2020:799-802.
Immunological Testing:
Healthcare providers use immunological techniques to detect antibodies.
Indirect Fluorescent Antibody Test (IFAT)
IFAT recognizes parasitic antigens by serum antibodies. This method uses fluorochrome anti-Ig antibodies to detect bound antibodies. IFAT holds 93.1% sensitivity and 88.9% specificity for the detection.16Karasová M, Tóthová C, Grelová S, Fialkovičová M. The etiology, incidence, pathogenesis, diagnostics, and treatment of canine babesiosis caused by Babesia gibsoni infection. Animals. 2022;12(6):739.
Enzyme-linked Immunosorbent Assay (ELISA)
ELISA detects the antibodies against Babesia in the serum. It can process a large number of samples at a time to save time. It has a higher specificity (97.4%) than IFAT. This test can identify ongoing infection and can monitor a high parasitic load. The other advantages of ELISA include the non-subjectivity and simplicity of the technique.17Karasová M, Tóthová C, Grelová S, Fialkovičová M. The etiology, incidence, pathogenesis, diagnostics, and treatment of canine babesiosis caused by Babesia gibsoni infection. Animals. 2022;12(6):739.
Immunochromatography
Immunochromatography is also a rapid diagnostic test to detect antibodies to specific antigens. It requires a small amount of serum and uses specific antibodies and test strips. It is an easy, rapid, and simple test, and its cost is lower than that of other techniques. This process requires only 15 minutes to complete.
Molecular Techniques:
Molecular techniques target nucleic acids and are generally used in conditions when immunological methods cannot be employed. Such conditions include acute or chronic infection and also when antibodies do not exist. In addition, molecular methods seem to be more specific and sensitive compared to immunological methods. The most frequently used approach for field diagnosis of babesiosis is the Polymerase chain reaction (PCR).
PCR
PCR can detect low parasitemia effectively. It is particularly beneficial because the identification is more accurate when microscopy cannot identify the parasites. PCR provides better results for distinguishing Babesia spp and is definitive when conventional microscopy is unsatisfactory.18Karasová M, Tóthová C, Grelová S, Fialkovičová M. The etiology, incidence, pathogenesis, diagnostics, and treatment of canine babesiosis caused by Babesia gibsoni infection. Animals. 2022;12(6):739.
Loop-Mediated Isothermal Amplification (LAMP)
LAMP, or Loop-Mediated Amplification, is a relatively young method of nucleic acid-based diagnostics. This method gives the result within a short period and has high sensitivity without requiring sophisticated instruments. For delamination, LAMP only calls for an ordinary water bath for the slide. The results are quite visible and one can read them with plain naked eye sight. Therefore, LAMP is a rapid, easy-to-perform, and inexpensive method of DNA amplification.19Liu A, Guan G, Du P, Gou H, Liu Z, Liu J, et al. Loop-mediated isothermal amplification (LAMP) method based on two species-specific primer sets for the rapid identification of Chinese Babesia bovis and B. bigemina. Parasitology international. 2012;61(4):658-63.
Treatment & Management of Babesiosis
Babesiosis therapy and approaches for control are considered depending on the disease’s stage, the species causing the infection, and the immunocompetency of the host. The following part of the article will provide comprehensive information on the available methods that may help to cure babesiosis.
Mild to Moderate Babesiosis
In children, the first-line treatment option is atovaquone 750 mg/ 12 hours. The recommended dose of azithromycin is 500 mg /day. Quinine sulfate 650 mg per dose and clindamycin 600 mg per dose is an alternative option for children.
The first-line treatment for babesiosis in adults involves the use of atovaquone together with azithromycin. Atovaquone recommended dosage is 750 mg per 12 hours. The recommended dose of azithromycin is 50 mg/ day and then 250mg/ day. The symptoms of babesiosis usually start resolving within one of the treatments. Clindamycin, along with quinine, is an alternative treatment option for babesiosis. A 650 mg dose of quinine and 600 mg dose of clindamycin, 600 mg after every eight hours, is recommended.20Ulusoy TÜ. CLINICAL FEATURES AND TREATMENT OF BABESIOSIS (PYROPLASMOSIS).
Severe Babesiosis
Adults require a regimen of oral atovaquone 750 mg every 12 hours and intravenous azithromycin 500 mg once a day in severe cases. It is the most effective drug combination. The alternative option is oral quinine sulfate 650 mg every eight hours plus intravenous clindamycin 600 mg every six hours.
To treat severe cases in children, the first line of treatment is atovaquone 750 mg per dose plus 500 mg of intravenous azithromycin per day.21Ulusoy TÜ. CLINICAL FEATURES AND TREATMENT OF BABESIOSIS (PYROPLASMOSIS).
Antibiotic therapy requires seven to ten days. Additionally, immunocompromised patients might not respond sufficiently to standard antibiotic therapy. These patients may require transfusion of erythrocytes. This process requires removing the patient’s erythrocytes and replacing them with the donor’s erythrocytes.
After treatment, the healthcare providers should monitor the susceptible patients who are at risk of potential complications.22Krause PJ. Human babesiosis. International journal for parasitology. 2019;49(2):165-74.
Complications
Treatment regimens of babesiosis often result in mild to severe complications. These complications include:
- Diarrhea
- Vertigo
- Tinnitus
- Decreased hearing
- Rash
Severe complications include:
- QT prolongation
- Cardiac arrhythmia23Ulusoy TÜ. CLINICAL FEATURES AND TREATMENT OF BABESIOSIS (PYROPLASMOSIS).
Prevention of Babesiosis
Following are the tips for effective prevention from babesiosis:
- Avoid visiting areas known for high tick populations. These include grassy, brushy, and wooded areas where deer and rodents thrive.
- Wear appropriate attire. Try to wear light-colored clothes to spot ticks easily.
- Tuck your pants into socks to avoid ticks crawling into your pants.
- In endemic areas, clothes treated with permethrin provide an additional layer of protection.
- Use insect repellents on exposed skin.
- After spending some time outdoors, thoroughly check yourself for ticks. You can seek help from a friend to check for the ticks. Pay special attention to the hidden areas.
• Take a shower within two hours of being outdoors. It will help wash off unattached ticks. - Modify your landscape. Keep grass trimmed and short. Remove leaf litter and brush piles where ticks may reside.
- Use recommended insect control products on your pets. Check them regularly for ticks after keeping them outdoors for some time.
- Beware of the signs of babesiosis and seek medical attention if you develop symptoms after being in the tick-infected area.
- Support local initiatives aimed at educating communities about tick-borne infection, prevention strategies, and safe outdoor practices.
- The most significant preventive measure is to protect the blood supply. Transmission of babesiosis through blood transfusion is a serious threat. People living in endemic areas should be prevented from donating blood if they have a history of babesiosis. However, this approach is inadequate, as many infections are asymptomatic.
- Screening of blood donors for pathogen exposure is the most common preventive measure. This method should be a must in endemic regions to decrease the risk of transfusion-mediated babesiosis.
- Pathogen inactivation can also successfully prevent transfusion-transmitted infection.
Babesiosis versus Lyme
Lyme and babesiosis are both tick-borne illnesses caused by different pathogens but transmitted by the same tick species. The key differences between the two conditions are given in the table below.
| Feature | Babesiosis | Lyme |
| Pathogen | Babesia spp. | Borrelia burgdorferi |
| Incubation Period | One to four weeks after a tick bite | 3 to 30 days after the tick bite |
| Symptoms
|
Fever
Chills Nausea Loss of appetite Dark urine Jaundice Shortness of breath |
Circular bull eye rash around the tick bite
Tiredness Neck stiffness Joint pain Memory problems Heart problems. |
| Risks | It can be life-threatening in immunocompromised patients. | Generally not life-threatening, but can lead to chronic symptoms. |
| Diagnosis | Blood smear examination, serology, and PCR | Clinical evaluation and serology, western blot for confirmation. |
| Treatment | Combination of antibiotics or antiparasitics | Antibiotics |
Final Remarks
Babesiosis represents a growing public health concern, particularly in endemic regions where tick populations are more prevalent. The symptoms are non-specific and closely match with other conditions. The severity of the disorder is recognized in the United States. In the U.S., routine testing for blood donations for Babesia is carried out, and there is a need for improved testing. The present antibiotic therapies are effective in the majority of the cases. However, immunocompromised patients require prolonged or more aggressive treatments. Continued research into active treatment and vaccines with robust public health initiatives should be focused on education and prevention, which are crucial for managing the disease and protecting the population at risk.
Refrences
- 1Cook MJ, Puri BK. Babesiosis: Analysis of the Evidence for Infections in the United Kingdom. International Journal of General Medicine. 2024:4627-31.
- 2Homer MJ, Aguilar-Delfin I, Telford III SR, Krause PJ, Persing DH. Babesiosis. Clinical microbiology reviews. 2000;13(3):451-69.
- 3Vannier E, Krause PJ. Babesiosis. Hunter’s tropical medicine and emerging infectious diseases. 2020:799-802.
- 4Bonnet SI, Nadal C. Experimental infection of ticks: An essential tool for the analysis of Babesia species biology and transmission. Pathogens. 2021;10(11):1403.
- 5Oz HS, Westlund KH. “Human babesiosis”: an emerging transfusion dilemma. International journal of hepatology. 2012;2012(1):431761.
- 6Vannier E, Krause PJ. Babesiosis. Hunter’s tropical medicine and emerging infectious diseases. 2020:799-802.
- 7Krause PJ. Human babesiosis. International journal for parasitology. 2019;49(2):165-74.
- 8Oz HS, Westlund KH. “Human babesiosis”: an emerging transfusion dilemma. International journal of hepatology. 2012;2012(1):431761.
- 9Oz HS, Westlund KH. “Human babesiosis”: an emerging transfusion dilemma. International journal of hepatology. 2012;2012(1):431761.
- 10Vannier E, Krause PJ. Babesiosis. Hunter’s tropical medicine and emerging infectious diseases. 2020:799-802.
- 11Krause PJ. Human babesiosis. International journal for parasitology. 2019;49(2):165-74.
- 12Vannier E, Krause PJ. Babesiosis. Hunter’s tropical medicine and emerging infectious diseases. 2020:799-802.
- 13Karasová M, Tóthová C, Grelová S, Fialkovičová M. The etiology, incidence, pathogenesis, diagnostics, and treatment of canine babesiosis caused by Babesia gibsoni infection. Animals. 2022;12(6):739.
- 14Krause PJ. Human babesiosis. International journal for parasitology. 2019;49(2):165-74.
- 15Vannier E, Krause PJ. Babesiosis. Hunter’s tropical medicine and emerging infectious diseases. 2020:799-802.
- 16Karasová M, Tóthová C, Grelová S, Fialkovičová M. The etiology, incidence, pathogenesis, diagnostics, and treatment of canine babesiosis caused by Babesia gibsoni infection. Animals. 2022;12(6):739.
- 17Karasová M, Tóthová C, Grelová S, Fialkovičová M. The etiology, incidence, pathogenesis, diagnostics, and treatment of canine babesiosis caused by Babesia gibsoni infection. Animals. 2022;12(6):739.
- 18Karasová M, Tóthová C, Grelová S, Fialkovičová M. The etiology, incidence, pathogenesis, diagnostics, and treatment of canine babesiosis caused by Babesia gibsoni infection. Animals. 2022;12(6):739.
- 19Liu A, Guan G, Du P, Gou H, Liu Z, Liu J, et al. Loop-mediated isothermal amplification (LAMP) method based on two species-specific primer sets for the rapid identification of Chinese Babesia bovis and B. bigemina. Parasitology international. 2012;61(4):658-63.
- 20Ulusoy TÜ. CLINICAL FEATURES AND TREATMENT OF BABESIOSIS (PYROPLASMOSIS).
- 21Ulusoy TÜ. CLINICAL FEATURES AND TREATMENT OF BABESIOSIS (PYROPLASMOSIS).
- 22Krause PJ. Human babesiosis. International journal for parasitology. 2019;49(2):165-74.
- 23Ulusoy TÜ. CLINICAL FEATURES AND TREATMENT OF BABESIOSIS (PYROPLASMOSIS).

