Liposarcoma is a group of rare, malignant soft tissue tumors developing in the fat tissues. Lipo means fat, while sarcoma means tumor of the soft tissues. Liposarcoma can develop in any part of the body, but arms, legs (especially thighs), abdominal (retroperitoneal) region, and groin (inguinal) region are the most common sites. The rare carcinomas account for a mere 1% of adult and 15% of all pediatric cancer diagnoses. However, liposarcomas are the most common type of soft sarcomas worldwide, accounting for 13-20% of all sarcoma cases.1Jonczak, E., Grossman, J., Alessandrino, F., Seldon Taswell, C., Velez-Torres, J. M., & Trent, J. (2024). Liposarcoma: A Journey into a Rare Tumor’s Epidemiology, Diagnosis, Pathophysiology, and Limitations of Current Therapies. Cancers, 16(22), 3858.
According to the National Cancer Institute, every year, around 2000 people are diagnosed with liposarcoma in the United States.2https://www.cancer.gov/pediatric-adult-rare-tumor/rare-tumors/rare-soft-tissue-tumors/myxoid-round-cell-liposarcoma Unfortunately, there has been an increase in liposarcoma diagnoses among American adults (an annual increase of 1.43%) in the recent past. Being of Caucasian origin and being male puts you at a greater risk of developing this recurring cancer.3Bock, S., Hoffmann, D. G., Jiang, Y., Chen, H., & Il’yasova, D. (2020). Increasing incidence of liposarcoma: a population-based study of national surveillance databases, 2001–2016. International journal of environmental research and public health, 17(8), 2710. Liposarcomas are notorious for recurrence and may require special/additional treatment and consequent long-term follow-up (to prevent cancer spread). Oncologists mostly treat the tumors with surgical excision as chemotherapy is not very successful. However, radiotherapy can prove to be a good adjunctive modality to surgery.
Types Of Liposarcomas
Several different types of sarcomas require different treatment modalities. The progression, recurrence rates, treatment plans, and outcomes vary between the different types of sarcomas.
Well-differentiated Liposarcoma (WDLS)
Also known as atypical lipomatous tumor, well-differentiated liposarcoma is the most common type of liposarcoma, accounting for about 30-50% of cases. The progression/growth rate of WDLS is slow, and the tumor is painless in most cases. Generally, it doesn’t spread to other body parts and is morphologically similar to normal fat tissues. However, it may recur in the same position. Many surgeons attribute cancer recurrence to an incomplete resection of the WDLS lesions.4Lu, J., Wood, D., Ingley, E., Koks, S., & Wong, D. (2021). Update on genomic and molecular landscapes of well-differentiated liposarcoma and dedifferentiated liposarcoma. Molecular Biology Reports, 48(4), 3637-3647.
The well-differentiated type mostly affects older individuals, i.e., males aged 50-65 years. The most common sites of WDLS development are:
- Limbs (arms and legs)
- Retroperitoneum (back of the abdomen)
Well-differentiated retroperitoneal liposarcomas have a good disease-free survival rate.5Osuna-Soto, J., Cuenca, T. C., Sanz-Zorrilla, A., Torrecilla-Martinez, A., Salas, R. O., & Leiva-Cepas, F. (2022). Prognosis and survival of patients diagnosed with well-differentiated and dedifferentiated retroperitoneal liposarcoma. Cirugía Española (English Edition), 100(10), 622-628.
Dedifferentiated Liposarcoma (DDLS)
Sometimes, the benign WDLS may transform into a more aggressive form, i.e., dedifferentiated liposarcoma. Unlike its well-differentiated sibling, undifferentiated liposarcoma is a rapidly growing tumor. DDLS develops in the same regions as WDLS. The choice of treatment for most doctors is surgical excision. However, DDLS is known for high recurrence (in almost 44% of cases), and the recurrence-free survival for DDLS is significantly low.6Dehner, C. A., Hagemann, I. S., & Chrisinger, J. S. (2021). Retroperitoneal Dedifferentiated Liposarcoma: The Presence of the Dedifferentiated Component at the Resection Margin Is Associated With Shorter Recurrence-Free Survival. American journal of clinical pathology, 156(5), 920-925.
Therefore, experts believe in adopting a multi-disciplinary approach (pathology and medical, radiation, surgical oncology) in DDLS management. Researchers suggest that surgeons perform resection in high-volume centers and consider radiation therapy for high-grade DDLS of extremities.7Haddox, C. L., Hornick, J. L., Roland, C. L., Baldini, E. H., Keedy, V. L., & Riedel, R. F. (2024). Diagnosis and management of dedifferentiated liposarcoma: A multidisciplinary position statement. Cancer Treatment Reviews, 131, 102846.
Myxoid Liposarcoma (MLPS)
Also known as Round cell liposarcoma, myxoid liposarcoma is the second most common type of fat cancer. It accounts for about 30% of all liposarcomas. It is called round-cell liposarcoma because the cells appear round when viewed under a microscope. Unlike well-differentiated liposarcoma, myxoid liposarcoma affects younger men 35-55 year olds.
Myxoid liposarcomas are aggressive tumors that require multiple treatment modalities. Prognosis and treatment plans vary from one individual to another. The outcomes of such tumors are generally poor.8Tfayli, Y., Baydoun, A., Naja, A. S., & Saghieh, S. (2021). Management of myxoid liposarcoma of the extremity. Oncology Letters, 22(2), 1-11.
It can affect different types of structures, including muscles, skin, and even bone. The tumor is most commonly found in the deep tissues of the thigh.9De Vita, A., Mercatali, L., Recine, F., Pieri, F., Riva, N., Bongiovanni, A., … & Ibrahim, T. (2016). Current classification, treatment options, and new perspectives in the management of adipocytic sarcomas. OncoTargets and therapy, 6233-6246. However, myxoid liposarcomas are not limited to legs and thighs. There have been reports of MLPS developing in the spine, lungs, esophagus, and heart.
Pleomorphic Liposarcoma
This least common type accounts for only 5-10% of all liposarcomas. However, this is the most aggressive of all subtypes. Most cases present with tumors in the extremities (deep tissues).10Anderson, W. J., & Jo, V. Y. (2019, March). Pleomorphic liposarcoma: updates and current differential diagnosis. In Seminars in Diagnostic Pathology (Vol. 36, No. 2, pp. 122-128). WB Saunders. This tumor subtype is notorious for growing and spreading very fast. Thus, it can quickly metastasize to the patient’s lungs. Studies conclude it to be a high-grade (aggressive) sarcoma that most commonly metastasizes to the lungs.11Downes, K. A., Goldblum, J. R., Montgomery, E. A., & Fisher, C. (2001). Pleomorphic liposarcoma: a clinicopathologic analysis of 19 cases. Modern Pathology, 14(3), 179-184. It requires quick diagnosis and treatment. Despite advanced treatment practices, pleomorphic liposarcoma has the worst survival rate.
Differentiating it from other tumor types is difficult. Diagnosis relies on the identification/recognition of pleomorphic lipoblasts (PLBs) which can be a difficult task.12Wakely Jr, P. E., Wangsiricharoen, S., & Ali, S. Z. (2022). Pleomorphic liposarcoma: a clinicopathologic study of 20 FNA cases. Cancer Cytopathology, 130(9), 705-713.
Myxoid Pleomorphic Liposarcoma
The myxoid pleomorphic liposarcoma is an extremely rare yet very aggressive subtype of liposarcoma. It is a recently discovered anomaly that prefers the mediastinum (space in the lungs that houses vital organs like the heart, trachea, esophagus, etc.) of young patients. Under the microscope, the tumor biopsy shows mixed cells of myxoid and pleomorphic liposarcoma. The mean age of development is 33 years, and the most common sites (apart from mediastinum) include the neck, cheek, back, and leg (including the thigh region).13Creytens, D., Folpe, A. L., Koelsche, C., Mentzel, T., Ferdinande, L., van Gorp, J. M., … & Flucke, U. (2021). Myxoid pleomorphic liposarcoma—a clinicopathologic, immunohistochemical, molecular genetic, and epigenetic study of 12 cases, suggesting a possible relationship with conventional pleomorphic liposarcoma. Modern Pathology, 34(11), 2043-2049.
The progression-free survival of this particular tumor is very low, and managing it is very difficult.14Dermawan, J. K., Hwang, S., Wexler, L., Tap, W. D., Singer, S., Vanderbilt, C. M., & Antonescu, C. R. (2022). Myxoid pleomorphic liposarcoma is distinguished from other liposarcomas by widespread loss of heterozygosity and significantly worse overall survival: a genomic and clinicopathologic study. Modern Pathology, 35(11), 1644-1655.
Liposarcoma Stages
Staging of this carcinoma is done using the Enneking oncologic staging system. The stages are as follows:
| Stages Of Cancer | Size And Spread |
| ⅠA | Tumor size<5 cm, and there is no spread (metastasis) of cancer to the body or the lymph nodes. |
| ⅠB | Tumor size>5cm and no spread. |
| ⅡA | Tumor size ≤ 5cm, no spread, but the grade is higher than ⅠA. |
| ⅡB | Tumor size ≥ 5cm, no spread, but the grade is higher than ⅡA. |
| ⅢA | Intra-compartmental tumor (high grade) that has metastasized. |
| Stage ⅢB | Extra-compartmental tumor that is malignant. |
| Ⅳ | The tumor has spread to different/other parts of the body. |
Liposarcoma Symptoms
The symptoms of liposarcoma depend on multiple factors including:
- Tumor location
- Tumor size
In some cases, there are no noticeable symptoms, while some patients may notice bumps or hard lumps underneath their skin. Most of the time, patients only notice the tumor when it becomes large enough to start putting pressure on the neighboring structures. Individuals may feel a push on organs like the stomach, intestines, or lungs. When present, individuals report the following symptoms:
Lumps Under The Skin
Several patients report lumps/bumps under the skin. Common sites for liposarcoma bumps include the back of the knees and the thigh area. However, you may also develop tumorous bumps in the arms. Clinicians advise you to immediately report a skin lump that measures 5 cm or more. There have been case reports of apparently innocuous tumorous growths becoming life-threatening.15Gearges, C., Fahmy, M., Siddiqui, S., & Iftikhar, A. (2023). BENIGN SKIN MASS TURNS INTO LETHAL CANCER LEADS TO CARDIAC ARREST: A CASE REPORT. CHEST, 164(4), A2563-A2564.
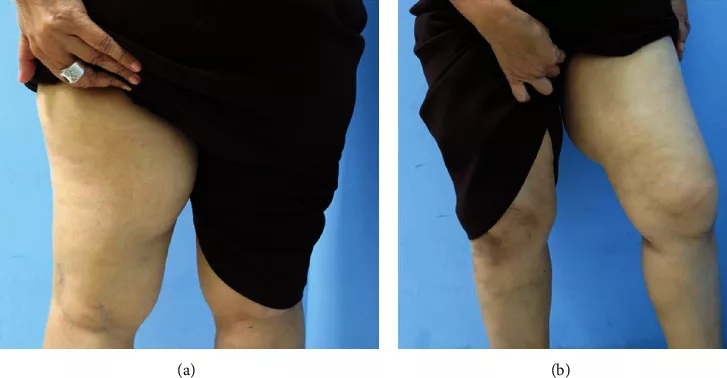
Some individuals can notice a new bump early on, while others note a persistently growing bump. Most of the bumps are not painful and cause discomfort (when they become large) by pressing against other structures. You may also notice weakness in the muscles of the affected thigh/arm.
Note: You should contact your healthcare provider if experiencing a skin bump larger than 5 centimeters.
Breathing Difficulties
Mediastinal liposarcomas are extremely rare, but they tend to cause significant breathing troubles by displacing the breathing apparatus.16De Llano, J. G., Mijares, M. F., Vasudevan, V., Arrangoiz, R., Sastry, A., De la Cruz, F., … & Legaspi, A. (2021). Mediastinal liposarcoma: case report and literature review. Journal of Cancer Therapy, 12(4), 208-220. Dedifferentiated liposarcoma in an 82-year-old male presented with shortness of breath, swallowing difficulty, and loss of voice.17Portnoy, R., Abbasi, R., Yablonsky, T. M., Cohen, E. G., & Widmann, M. (2024). Mediastinal liposarcoma: Case report with radiology review. Radiology Case Reports, 19(8), 3294-3300.
Appetite Loss
Several liposarcoma patients report having appetite loss. In multiple cases, there is a feeling of being full even at the start of eating. Advanced giant retroperitoneal dedifferentiated liposarcomas can cause abdominal distention and lead to loss of appetite.18Tani, A., Tarumi, Y., Kakibuchi, A., Aoyama, K., Kokabu, T., Kataoka, H., … & Mori, T. (2022). Giant retroperitoneal dedifferentiated liposarcoma mimicking ovarian cancer: a case report. Gynecologic Oncology Reports, 44, 101088.
Gastric Upset
Constipation is an unusual presentation of liposarcomas. Giant retroperitoneal liposarcomas can cause gastric symptoms by pushing down the diaphragm which consequently leads to gastric upset. Progressive constipation was an evident symptom in a 72-year-old male suffering from giant retroperitoneal liposarcoma.19Rabai, N. A., Alrababah, A., Halalsheh, O., Ba-shamakh, S., & Batayha, S. A. A Giant Retroperitoneal Dedifferentiated Liposarcoma Presenting as Progressive Constipation: A Rare Case Report. Int Clinc Med Case Rep Jour. 2023; 2 (16): 1, 12. Rectal bleeding and constipation may be the initial symptoms in cases of hidden giant retroperitoneal liposarcomas.20Shindgikar, P., & Yip, B. (2024). S3057 Unveiling the Hidden Giant: Multidisciplinary Management of a Retroperitoneal Dedifferentiated Liposarcoma. Official journal of the American College of Gastroenterology| ACG, 119(10S), S2080-S2081.
Moreover, metastasis can affect the intestines. Colonic liposarcomas contribute to gastric abnormalities like constipation and intermittent diarrhea.21Chaturvedi, R. A., Patil, R. D., Sonavane, T. S., & Tripathi, N. (2023). Metastatic dedifferentiated liposarcoma of ileum presenting as an ileal mass with intussusception—A rare case with literature review. Indian Journal of Pathology and Microbiology, 66(1), 213-215.
Blood In Vomit/Stool
Mixing of blood in vomit or stool can be indicative of underlying liposarcoma. Your poop may look black or tarry due to mixing of blood.
Abdominal Pain & Distention
Retroperitoneal liposarcomas are common retroperitoneal tumors that are known to cause abdominal symptoms. Painless masses slowly grow to impact the structures of the abdomen. It mainly manifests as abdominal distention and pain. Some might also experience cramping.22Li, Y. M., Zhu, H. H., Wang, X. Q., Shi, M. Z., & ShangGuan, C. L. (2024). Giant mucinous liposarcoma of the abdominal cavity: A case report. Medicine, 103(33), e39282.
Liposarcoma Causes
The exact cause of the uncontrolled growth of fat cells is unknown. However, according to experts, genetic mutations are the main cause of liposarcoma. Numerous mutations are linked to the cancer. Experts believe that as many as 20 different genetic mutations can lead to liposarcoma development. Recently, alterations in new driver genes have been identified in well-differentiated retroperitoneal liposarcoma.23Tyler, R. W. (2022). Identifying new driver genes in well-differentiated retroperitoneal liposarcoma (Doctoral dissertation, University of Birmingham).
Moreover, researchers have noted a high incidence of pleomorphic myxoid liposarcoma in cases of Li-Frameni syndrome (an inherited genetic mutation disorder).24Zare, S. Y., Leivo, M., & Fadare, O. (2020). Recurrent pleomorphic myxoid liposarcoma in a patient with Li-Fraumeni syndrome. International Journal of Surgical Pathology, 28(2), 225-228. 25Francom, C. R., Leoniak, S. M., Lovell, M. A., & Herrmann, B. W. (2019). Head and neck pleomorphic myxoid liposarcoma in a child with Li-Fraumeni syndrome. International Journal of Pediatric Otorhinolaryngology, 123, 191-194.
Radiation exposure can also serve as a contributing factor for liposarcomas. Studies indicate that women undergoing radiation therapy for breast carcinoma are at a greater risk of developing soft tissue carcinomas like liposarcoma.26Huang, J., & Mackillop, W. J. (2001). Increased risk of soft tissue sarcoma after radiotherapy in women with breast carcinoma. Cancer, 92(1), 172-180.
Exposure to workplace chemicals like vinyl chloride, arsenic compounds, and alkylators can also increase your chances of falling prey to liposarcoma.27Giselle, H. P., Mariana, C. B., Cintia, F., Tatiana, G., Noelia, F., Gabriela, T., … & Gustavo, H. (2021). Liposarcoma of the chest wall mimicking a breast mass in a man: a case report. Radiology Case Reports, 16(11), 3400-3405.
Liposarcoma Diagnosis
History & Physical Examination:
Your healthcare provider will start by taking your history. Common questions include details of symptoms. When suspected, the doctor may also ask about a family history of cancer.
A thorough examination of the affected area follows history-taking. After the physical exam, your healthcare provider may order an array of imaging tests.
Radiography/Imaging Tests:
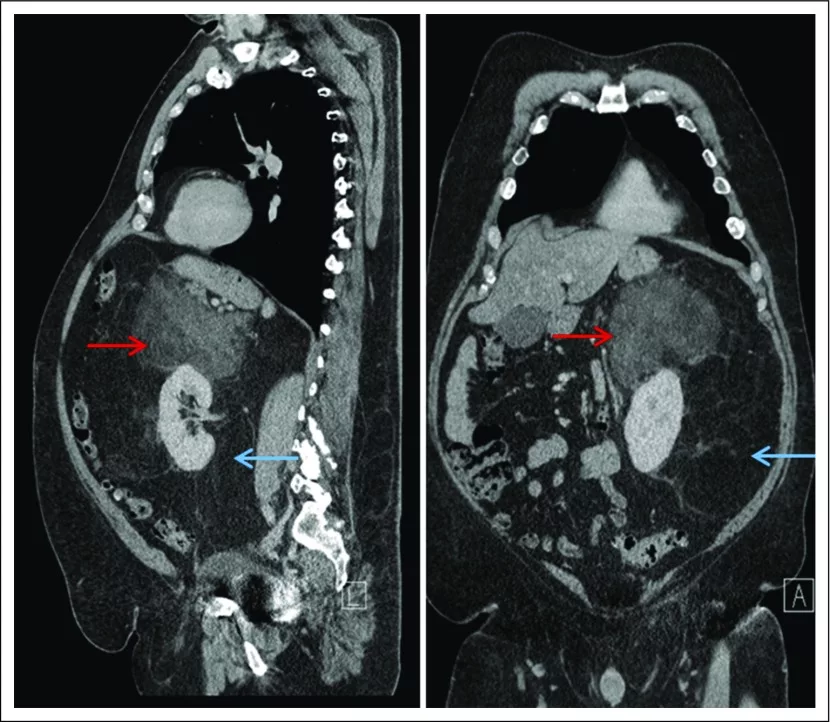
CT scans
Computed tomography scans help locate tumors while revealing the proximity of the tumors to vital organs. Oncologists also use CTs to evaluate tumor size.
MRI Scans
Magnetic Resonance Imaging scans help visualize the nearby muscles, nerves, blood vessels, etc. It is important to note these structures to identify the potential damage the liposarcoma can cause.
Your doctor may also use conventional X-rays or positron emission tomography (PET) scans.
Biopsy:
For numerous tumorous growths (including liposarcoma), doctors opt for removing a part (tissue sample) of the affected region. The biopsy samples are sent to pathologists, who observe the abnormal cells under a microscope.
Genetic/Molecular Testing:
For molecular genetic testing, the doctor removes some blood, and body fluids (or tissues) and sends it to the lab. In the lab, professionals look for changes in chromosomes, DNA, and proteins. This test determines the specific type of liposarcoma.
Differential Diagnosis:
Liposarcoma Vs Lipoma
Both lipomas and liposarcomas are fatty carcinomas, but lipomas are benign tumors, while liposarcomas are malignant cancers. Lipomas are commonly seen near the skin of the neck, arms, and shoulders, but liposarcomas’ preferred site is the depth of the abdomen and thighs. Moreover, lipomas generally do not grow more than 2cm in size. On the other hand, liposarcomas can grow very large.
Liposarcoma Treatment
Oncologists adopt different types of treatment plans to manage liposarcomas in various regions. An important point of consideration in liposarcoma treatment is the spread of cancer to other regions. The majority of the time, doctors utilize a combination of two or more therapies for complete treatment. The most prevalent treatment options include:
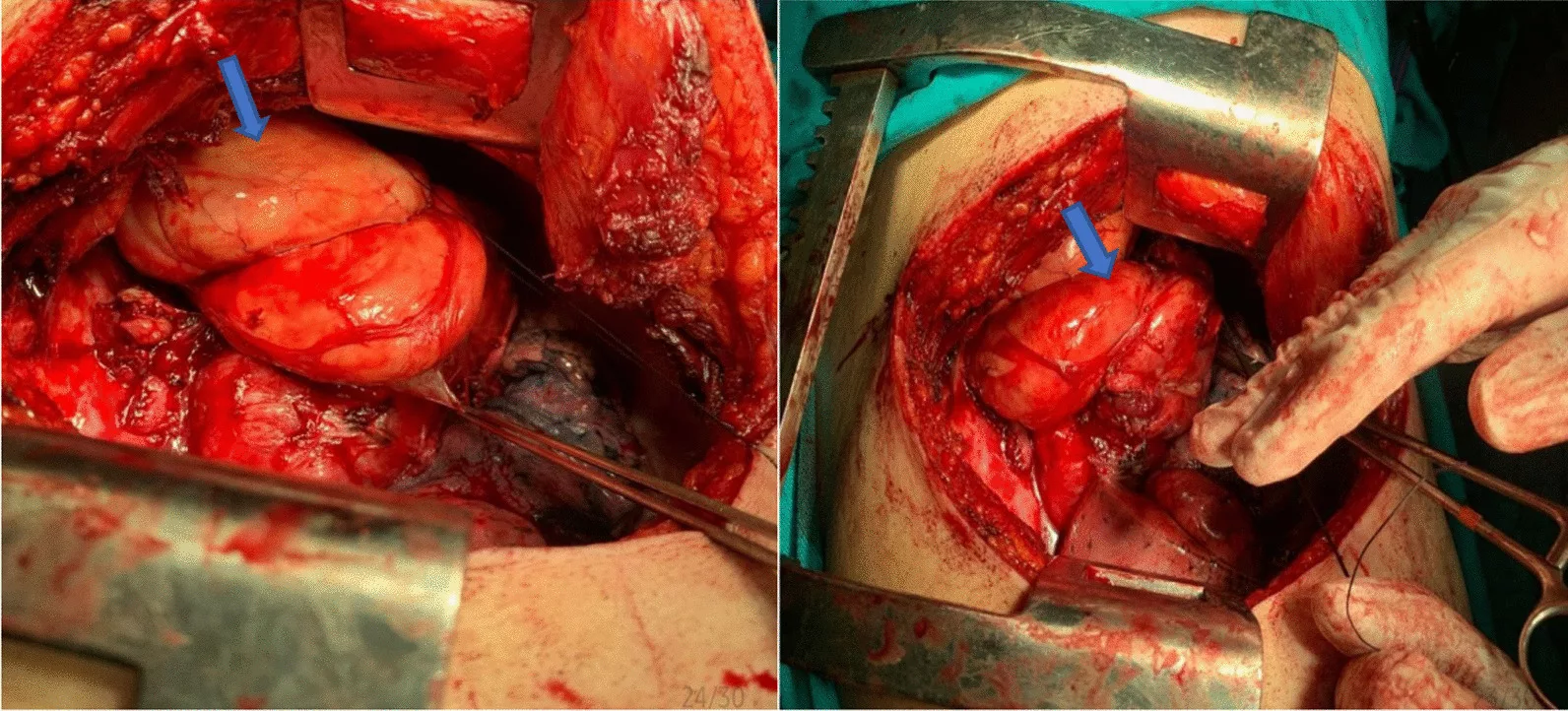
Surgery
Surgical excision is the primary treatment type for all liposarcomas. Experts prefer surgical resection of liposarcoma tumors when diagnosis is confirmed. However, the prognosis of liposarcoma treatment is poor.28Zhao, C., Han, Z., Xiao, H., Yang, C., Zhao, Y., Fan, T., … & Xiao, J. (2016). Surgical management of spinal liposarcoma: a case series of 7 patients and literature review. European Spine Journal, 25, 4088-4093. Poor outcomes are partly attributed to the high recurrence rate of the carcinoma. Modern studies conclude that early surgical management of primary retroperitoneal liposarcomas is linked to better outcomes.29Chen, J., Hang, Y., Gao, Q., & Huang, X. (2021). Surgical diagnosis and treatment of primary retroperitoneal liposarcoma. Frontiers in Surgery, 8, 672669.
Radiation Therapy
There are two aims of radiotherapy. One purpose of radiotherapy is to shrink the size of the tumor before surgical removal. Doctors usually use adjunctive radiotherapy in myxoid liposarcoma. Your cancer specialist may also deliver radiation therapy after surgical excision to reduce the risk of the cancer coming back.30Haddox, C. L., & Riedel, R. F. (2021). Recent advances in the understanding and management of liposarcoma. Faculty reviews, 10.
Chemotherapy
Doctors administer chemical agents in cases where surgical excision or surgery can not be done. Chemotherapy is not the preferred choice of therapy.
Are There Any Complications Of The Treatment?
Yes, cancer treatment can cause several complications. Doctors outweigh the benefits of a particular treatment to the risks before starting. Your oncologist will discuss the potential pitfalls of cancer treatment (chemo, radiotherapy, surgery). The following issues are seen:
- Fatigue
- Skin issues (soreness, redness, dryness, etc.)
- Bone weakness
- Non-healing surgical wounds
- Infection
- Nausea and vomiting
Liposarcoma Prognosis
Liposarcomas generally have a poor prognosis due to high recurrence rates. Research shows that large, symptomatic dedifferentiated, and pleomorphic liposarcomas have poor prognosis. On the other hand, well-differentiated or myxoid liposarcomas have a relatively better prognosis.31Xiao, J., Liu, J., Chen, M., Liu, W., & He, X. (2021). Diagnosis and prognosis of retroperitoneal liposarcoma: a single Asian center cohort of 57 cases. Journal of Oncology, 2021(1), 7594027.
According to one study, the five-year survival rate for recurrent retroperitoneal liposarcoma was 34.4%. Combined organ and tumor resection favored the survival of patients.32Deng, H., Gao, J., Xu, X., Liu, G., Song, L., Pan, Y., & Wei, B. (2023). Predictors and outcomes of recurrent retroperitoneal liposarcoma: new insights into its recurrence patterns. BMC cancer, 23(1), 1076.
Conclusion
Liposarcoma is a cancer of the fat cells. It mostly affects the fats in the deep skin layers of your thigh, legs, arms, etc. Well-differentiated liposarcoma is the most common type that progresses slowly, while myxoid and pleomorphic types are rare and grow aggressively. Liposarcomas have a high recurrence rate, therefore, progression-free survival of patients is poor.
Most tumors are asymptomatic, but very large-sized tumors can cause symptoms by pressing on neighboring structures. When present, symptoms include skin lumps, appetite loss, constipation, breathing issues, and abdominal distention. Genetic mutations lead to carcinoma, and doctors diagnose it using molecular genetic testing and radiographic imaging (CT, MRIs, etc.) Oncologists treat cancers of different regions mainly with surgery and radiation therapy. Chemotherapy is not commonly used. The prognosis of liposarcoma is poor.
Refrences
- 1Jonczak, E., Grossman, J., Alessandrino, F., Seldon Taswell, C., Velez-Torres, J. M., & Trent, J. (2024). Liposarcoma: A Journey into a Rare Tumor’s Epidemiology, Diagnosis, Pathophysiology, and Limitations of Current Therapies. Cancers, 16(22), 3858.
- 2https://www.cancer.gov/pediatric-adult-rare-tumor/rare-tumors/rare-soft-tissue-tumors/myxoid-round-cell-liposarcoma
- 3Bock, S., Hoffmann, D. G., Jiang, Y., Chen, H., & Il’yasova, D. (2020). Increasing incidence of liposarcoma: a population-based study of national surveillance databases, 2001–2016. International journal of environmental research and public health, 17(8), 2710.
- 4Lu, J., Wood, D., Ingley, E., Koks, S., & Wong, D. (2021). Update on genomic and molecular landscapes of well-differentiated liposarcoma and dedifferentiated liposarcoma. Molecular Biology Reports, 48(4), 3637-3647.
- 5Osuna-Soto, J., Cuenca, T. C., Sanz-Zorrilla, A., Torrecilla-Martinez, A., Salas, R. O., & Leiva-Cepas, F. (2022). Prognosis and survival of patients diagnosed with well-differentiated and dedifferentiated retroperitoneal liposarcoma. Cirugía Española (English Edition), 100(10), 622-628.
- 6Dehner, C. A., Hagemann, I. S., & Chrisinger, J. S. (2021). Retroperitoneal Dedifferentiated Liposarcoma: The Presence of the Dedifferentiated Component at the Resection Margin Is Associated With Shorter Recurrence-Free Survival. American journal of clinical pathology, 156(5), 920-925.
- 7Haddox, C. L., Hornick, J. L., Roland, C. L., Baldini, E. H., Keedy, V. L., & Riedel, R. F. (2024). Diagnosis and management of dedifferentiated liposarcoma: A multidisciplinary position statement. Cancer Treatment Reviews, 131, 102846.
- 8Tfayli, Y., Baydoun, A., Naja, A. S., & Saghieh, S. (2021). Management of myxoid liposarcoma of the extremity. Oncology Letters, 22(2), 1-11.
- 9De Vita, A., Mercatali, L., Recine, F., Pieri, F., Riva, N., Bongiovanni, A., … & Ibrahim, T. (2016). Current classification, treatment options, and new perspectives in the management of adipocytic sarcomas. OncoTargets and therapy, 6233-6246.
- 10Anderson, W. J., & Jo, V. Y. (2019, March). Pleomorphic liposarcoma: updates and current differential diagnosis. In Seminars in Diagnostic Pathology (Vol. 36, No. 2, pp. 122-128). WB Saunders.
- 11Downes, K. A., Goldblum, J. R., Montgomery, E. A., & Fisher, C. (2001). Pleomorphic liposarcoma: a clinicopathologic analysis of 19 cases. Modern Pathology, 14(3), 179-184.
- 12Wakely Jr, P. E., Wangsiricharoen, S., & Ali, S. Z. (2022). Pleomorphic liposarcoma: a clinicopathologic study of 20 FNA cases. Cancer Cytopathology, 130(9), 705-713.
- 13Creytens, D., Folpe, A. L., Koelsche, C., Mentzel, T., Ferdinande, L., van Gorp, J. M., … & Flucke, U. (2021). Myxoid pleomorphic liposarcoma—a clinicopathologic, immunohistochemical, molecular genetic, and epigenetic study of 12 cases, suggesting a possible relationship with conventional pleomorphic liposarcoma. Modern Pathology, 34(11), 2043-2049.
- 14Dermawan, J. K., Hwang, S., Wexler, L., Tap, W. D., Singer, S., Vanderbilt, C. M., & Antonescu, C. R. (2022). Myxoid pleomorphic liposarcoma is distinguished from other liposarcomas by widespread loss of heterozygosity and significantly worse overall survival: a genomic and clinicopathologic study. Modern Pathology, 35(11), 1644-1655.
- 15Gearges, C., Fahmy, M., Siddiqui, S., & Iftikhar, A. (2023). BENIGN SKIN MASS TURNS INTO LETHAL CANCER LEADS TO CARDIAC ARREST: A CASE REPORT. CHEST, 164(4), A2563-A2564.
- 16De Llano, J. G., Mijares, M. F., Vasudevan, V., Arrangoiz, R., Sastry, A., De la Cruz, F., … & Legaspi, A. (2021). Mediastinal liposarcoma: case report and literature review. Journal of Cancer Therapy, 12(4), 208-220.
- 17Portnoy, R., Abbasi, R., Yablonsky, T. M., Cohen, E. G., & Widmann, M. (2024). Mediastinal liposarcoma: Case report with radiology review. Radiology Case Reports, 19(8), 3294-3300.
- 18Tani, A., Tarumi, Y., Kakibuchi, A., Aoyama, K., Kokabu, T., Kataoka, H., … & Mori, T. (2022). Giant retroperitoneal dedifferentiated liposarcoma mimicking ovarian cancer: a case report. Gynecologic Oncology Reports, 44, 101088.
- 19Rabai, N. A., Alrababah, A., Halalsheh, O., Ba-shamakh, S., & Batayha, S. A. A Giant Retroperitoneal Dedifferentiated Liposarcoma Presenting as Progressive Constipation: A Rare Case Report. Int Clinc Med Case Rep Jour. 2023; 2 (16): 1, 12.
- 20Shindgikar, P., & Yip, B. (2024). S3057 Unveiling the Hidden Giant: Multidisciplinary Management of a Retroperitoneal Dedifferentiated Liposarcoma. Official journal of the American College of Gastroenterology| ACG, 119(10S), S2080-S2081.
- 21Chaturvedi, R. A., Patil, R. D., Sonavane, T. S., & Tripathi, N. (2023). Metastatic dedifferentiated liposarcoma of ileum presenting as an ileal mass with intussusception—A rare case with literature review. Indian Journal of Pathology and Microbiology, 66(1), 213-215.
- 22Li, Y. M., Zhu, H. H., Wang, X. Q., Shi, M. Z., & ShangGuan, C. L. (2024). Giant mucinous liposarcoma of the abdominal cavity: A case report. Medicine, 103(33), e39282.
- 23Tyler, R. W. (2022). Identifying new driver genes in well-differentiated retroperitoneal liposarcoma (Doctoral dissertation, University of Birmingham).
- 24Zare, S. Y., Leivo, M., & Fadare, O. (2020). Recurrent pleomorphic myxoid liposarcoma in a patient with Li-Fraumeni syndrome. International Journal of Surgical Pathology, 28(2), 225-228.
- 25Francom, C. R., Leoniak, S. M., Lovell, M. A., & Herrmann, B. W. (2019). Head and neck pleomorphic myxoid liposarcoma in a child with Li-Fraumeni syndrome. International Journal of Pediatric Otorhinolaryngology, 123, 191-194.
- 26Huang, J., & Mackillop, W. J. (2001). Increased risk of soft tissue sarcoma after radiotherapy in women with breast carcinoma. Cancer, 92(1), 172-180.
- 27Giselle, H. P., Mariana, C. B., Cintia, F., Tatiana, G., Noelia, F., Gabriela, T., … & Gustavo, H. (2021). Liposarcoma of the chest wall mimicking a breast mass in a man: a case report. Radiology Case Reports, 16(11), 3400-3405.
- 28Zhao, C., Han, Z., Xiao, H., Yang, C., Zhao, Y., Fan, T., … & Xiao, J. (2016). Surgical management of spinal liposarcoma: a case series of 7 patients and literature review. European Spine Journal, 25, 4088-4093.
- 29Chen, J., Hang, Y., Gao, Q., & Huang, X. (2021). Surgical diagnosis and treatment of primary retroperitoneal liposarcoma. Frontiers in Surgery, 8, 672669.
- 30Haddox, C. L., & Riedel, R. F. (2021). Recent advances in the understanding and management of liposarcoma. Faculty reviews, 10.
- 31Xiao, J., Liu, J., Chen, M., Liu, W., & He, X. (2021). Diagnosis and prognosis of retroperitoneal liposarcoma: a single Asian center cohort of 57 cases. Journal of Oncology, 2021(1), 7594027.
- 32Deng, H., Gao, J., Xu, X., Liu, G., Song, L., Pan, Y., & Wei, B. (2023). Predictors and outcomes of recurrent retroperitoneal liposarcoma: new insights into its recurrence patterns. BMC cancer, 23(1), 1076.

