Brachioradial Pruritus is a medical condition involving localized dysesthesia (a set of symptoms associated with unusual touch sensations) of the upper limb. In this condition, you feel pain and abnormal sensations in your forearm and arm. It is a benign, treatable condition. However, its diagnosis and treatment are very difficult.
What Is Brachioradial Pruritus?
It is a neuropathic dysesthesia of the dorsolateral surface of the upper arm, forearms, and sometimes shoulders. It is common in females, and the patient feels itchiness in the forearms. You may feel sensations of itching, burning, or tingling in your upper limbs. It is common in middle-aged women, and exposure to ultraviolet radiation is its cause.1Pinto, A. C., Wachholz, P. A., Masuda, P. Y., & Martelli, A. C. (2016). Clinical, epidemiological and therapeutic profile of patients with brachioradial pruritus in a reference service in dermatology. Anais brasileiros de dermatologia, 91(4), 549–551. https://doi.org/10.1590/abd1806-4841.201644767
Causes Of Brachioradial Pruritus
There are the following causes of brachioradialis pruritus:
Ultraviolet Radiations:
Ultraviolet radiation is a major cause of this condition. It damages the nerve endings in your skin, increases its sensitivity, makes it dry, and releases histamine. All these factors cause irritation of your skin, and itching is a key symptom of this condition.
Cervical Spine Problems:
Patients having cervical spine problems like disc herniation, osteoarthritis, disc impingement, and degenerative disease are more prone to develop brachioradial pruritus. The reason behind that is cervical nerve irritation, leading to this condition.2Marziniak, M., Phan, N. Q., Raap, U., Siepmann, D., Schürmeyer-Horst, F., Pogatzki-Zahn, E., Niederstadt, T., & Ständer, S. (2011). Brachioradial pruritus as a result of cervical spine pathology: the results of a magnetic resonance tomography study. Journal of the American Academy of Dermatology, 65(4), 756–762. https://doi.org/10.1016/j.jaad.2010.07.036
Sun Exposure:
Sun exposure is one of the major causes of this condition. Sunlight produces ultraviolet radiation, which releases histamine and causes brachioradial pruritus. Moreover, sunlight damages C fibers and decreases the C fibers in your nerves, causing brachioradial pruritus.
Compression Of Nerves In Neck:
Compression of the nerves in the neck causes irritation and itching, leading to brachioradial pruritus. Damage to the fifth to eighth cervical nerve may also be a cause.
Other Systemic Diseases:
Other systemic diseases like cholestasis, polycythemia, Hodgkin’s lymphoma, renal insufficiency, and solid tumors can also cause pruritus.3Sommer, F., Hensen, P., Böckenholt, B., Metze, D., Luger, T. A., & Ständer, S. (2007). Underlying diseases and co-factors in patients with severe chronic pruritus: a 3-year retrospective study. Acta dermato-venereologica, 87(6), 510–516. https://doi.org/10.2340/00015555-0320
Who is prone to develop Brachioradial Pruritus?
It has many risk factors; people at greater risk of developing this condition are:
- Women
- Middle age people
- Sun exposure
- People with fair skin
- Cervical spine problems
- Elderly age
- Ultraviolet light exposure
- Neuropathic problems
Symptoms Of Brachioradial Pruritus
Some of the symptoms are:
- Severe Itching
- Severe, irritable itching in your arms, particularly forearms
- Burning
- Tingling of pins in your arms
- Numbness
- Paraesthesia
- Crawling sensation in arms
- Pain radiating from your neck to arms and forearms
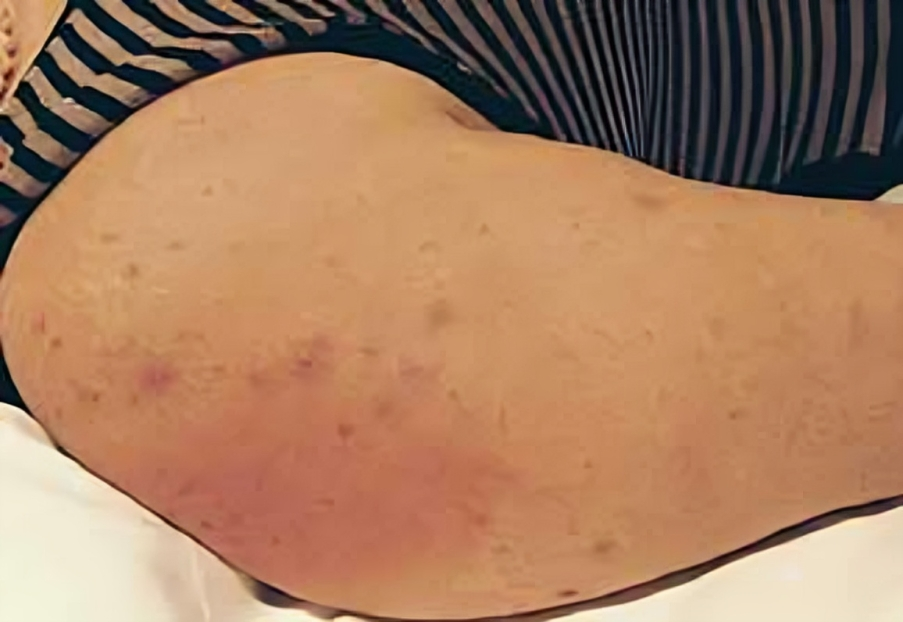
- Inflammation and redness of skin
- Skin lesions
These symptoms and their severity vary in different patients depending on the cause, risk factors, and ethnicity of the patient.

Management Of Brachioradial Pruritus
Management involves a thorough history and examination at first, followed by investigations and treatment of this condition by your doctor.
History:
Your doctor asks the following questions if he suspects brachioradial pruritus:
- History of pain, tingling, stinging, numbness, or paresthesia in arms and forearms.
- History of sun exposure or any professional related to sun exposure.
- Neck pain, neck trauma, any cervical spine disease, previous skin diseases, history of any spine disease, nerve damage, or disc herniation.
Examination:
The first examination includes a complete general physical examination. The next steps are:
Skin Examination
If you have brachioradial pruritus, your doctor will examine your skin thoroughly for redness, scars, scratching, or other lesions.
Neurological Examination
After skin examination, the next step is neurological examination, in which the doctor examines nerves, muscles, and strength.
Examination Of Spine
Your doctor also examines the spine for tenderness or signs of spinal cord compression.
Sensory Examination
Then, the doctor performs a detailed sensory examination for pain, touch, and temperature sensations.
Motor Examination
The doctor performs a complete motor examination to check the muscles, tone, and strength.
Reflexes
A doctor assesses the patient’s reflexes because this condition can be due to some nerve issues.
Ice Pack Sign
If you suspect brachioradial pruritus and you do icing of the affected area, it results in the improvement of symptoms of brachioradial, it is a positive Ice pack sign. It is a common sign, and the condition recurs after removing the ice pack.4Medical Pearl: The ice-pack sign in brachioradial pruritus Bernhard, Jeffrey D. et al. Journal of the American Academy of Dermatology, Volume 52, Issue 6, 1073
Investigations:
There are the following investigations:
Imaging Studies
Imaging studies include X-ray, CT scan, MRI brain, and CT cervical spine.
Electromyography
Electromyography (EMG) and Nerve Conduction Studies (NCS) are important for patients with brachioradialis pruritus because their nerves are damaged.
Skin Biopsy
Your doctor may recommend a skin biopsy. These studies are done to rule out other skin conditions.
Treatment Of Brachioradial Pruritus
Treatment of brachioradial includes the following:
Protection From Sunlight:
For the treatment, your doctor will advise you to protect yourself from sunlight, such as using sunscreen, avoiding going out in mid-day, wearing ultraviolet light-protective clothes, wearing full-sleeve dresses, and icing the affected area.
Steroids:
Topical steroids are a good option for the treatment of brachioradial pruritus. They suppress your immune system, reduce inflammation, and stabilize your nerves. Your doctor can advise steroids in oral, topical, or injection form, but their excessive use can make you prone to skin infections or other problems.
Capsaicin Cream & Other Topical Medicines:
Doctors also advise capsaicin Cream and other typical medicines like lidocaine and triamcinolone for brachioradialis pruritus. Capsaicin cream works by reducing Substance P from your nerve fibers, which is a transmitter for pain sensations. So, it reduces pain transmission, and you get relief from pain and itching.5Pereira, M. P., Lüling, H., Dieckhöfer, A., Steinke, S., Zeidler, C., Agelopoulos, K., & Ständer, S. (2018). Application of an 8% capsaicin patch normalizes epidermal TRPV1 expression but not the decreased intraepidermal nerve fiber density in patients with brachioradial pruritus. Journal of the European Academy of Dermatology and Venereology: JEADV, 32(9), 1535–1541. https://doi.org/10.1111/jdv.14857
Antihistamines:
Your doctor may advise you to take antihistamine drugs like diphenhydramine and chlorpheniramine to treat this condition. These drugs work by blocking the release of histamine from the nerve fibers and controlling allergy. They also have a sedating effect that can help you sleep at night and avoid scratching.
Anticonvulsants:
Anticonvulsants like pregabalin and gabapentin are used in the management of this condition. They act by down-regulating your Gamma amino butyric acid (GABA) receptors and Calcium channel receptors, reducing pain transmission to these receptors. So, it gives you relief from pain and itching.6Yilmaz, S., Ceyhan, A. M., & Baysal Akkaya, V. (2010). Brachioradial pruritus successfully treated with gabapentin. The Journal of Dermatology, 37(7), 662–665. https://doi.org/10.1111/j.1346-8138.2010.00830.x
Tricyclic Antidepressants:
Doctors also prescribe tricyclic antidepressants like amitriptyline. These drugs reduce the reuptake of serotonin from the serotonin receptors. Moreover, they have antihistamine and sedative effects that help relieve severe itching. They also reduce neuropathic pain.7Wachholz, P. A., Masuda, P. Y., Pinto, A. C. V. D., & Martelli, A. C. C. (2017). Impact of drug therapy on brachioradial pruritus. Anais brasileiros de dermatologia, 92(2), 281–282. https://doi.org/10.1590/abd1806-4841.20175321.
Surgical Treatment:
As this condition is caused by cervical spine herniation or other spine issues, the recent surgical method for the treatment is a CT-guided nerve block. In this method, analgesic is injected into the cervical nerve root and it is effective in the treatment of this condition. It is a very effective method for patients complaining about chronic brachioradial pruritus related to cervical spine issues. Mostly, your doctor uses CT-guided steroid injections in this method.
Is Brachioradial Pruritus Genetic Disorder?
No, It is not a genetic disorder. It is just related to environmental factors and spine abnormalities.
Prognosis
The prognosis is not good; you may develop chronic brachioradial pruritus lasting for months or years. Moreover, it may relapse after the treatment. Its treatment also takes a lot of time and is difficult.
Complications
If chronic, this condition has many complications. Continuous itching and scratching lead to scratch marks and sores on the skin. The lesions can also become infected. Moreover, many diseases like prurigo (hard lumps on the skin), lichenification (thick plaques on the skin), hypopigmentation, or hyperpigmentation can also occur.
Does Brachioradial Pruritus become worse at night & why?
Yes, it becomes worse at night. Your body releases cytokines at night, which are inflammatory mediators. These induce inflammation, and pruritus becomes worse at night.
What Cervical Vertebrae Are Involved In Brachioradial Pruritus?
It mostly involves the fifth to eighth cervical vertebrae. The dermatomes of your arm are cervical nerve (C5) five to cervical nerve six (C6).
Differential Diagnosis
There are many differential diagnosis of this condition; some of them are:
- Atopic dermatitis
- Contact dermatitis
- Notalgia paresthetica
- Systemic disease
- Nerve related pruritus
- Peripheral neuropathy
- Psychogenic
- Shingles
- Nerve damage
- Pruritus due to diseases like multiple endocrine neoplasia (MEN)
Brachioradial Pruritus Vs. Scabies
| Brachioradial Pruritus | Scabies | |
| Definition | Brachioradial pruritus is a neurological skin condition in which there is excessive itching and paraesthesia of your skin. | Scabies is a skin condition characterized by severe itching, erythema, and small reddish blisters, particularly on the armpits, wrists, elbows, and genital area. |
| Cause
Spread |
The cause of brachioradial pruritus is related to nerves like nerve damage or some cervical disc problems.
Brachioradial pruritus is a non-contagious disease. |
The cause of scabies is Sarcoptes scabiei or Itch mite.
Scabies is a contagious disease spread by direct contact or using contaminated things by the infected person. |
| Treatment | Your doctor may recommend drugs such as topical anesthetics, anticonvulsants, steroids, and creams to treat brachioradial pruritus. | Your doctor may recommend creams and lotions, such as permethrin lotion and ivermectin, for treating scabies. |
Is Brachioradial Pruritus Affected by Pregnancy?
Yes, brachioradialis pruritus is affected by pregnancy and gets worsened by it. Although it is unrelated to pregnancy, it is common in pregnant ladies. Moreover, pruritus can also occur due to any systemic disease that occurs during pregnancy.
Correlation of Brachioradial Pruritus with Thyroid Disease
This condition is closely related to thyroid disease. Both hypothyroidism and hyperthyroidism can cause skin itching, eczema, scaly skin, and skin diseases like psoriasis and brachioradialis pruritus. Autoimmune disorders like Grave’s disease and Hashimoto’s thyroiditis can also lead to brachioradial pruritus. Thyroid disease is one of the common causes of this condition.
Difference between Notalgia Paresthetica & Brachioradial Pruritus
Both brachioradial pruritus and notalgia paresthetica are neuropathic conditions. Their symptoms resemble each other, but there are also differences. Brachioradial pruritus commonly involves the forearm between the elbow and wrist, while notalgia paresthetica involves the shoulder blades and upper back.
It affects your arms bilaterally, while notalgia paresthetica is unilateral.
Moreover, triggering factors for brachioradial pruritus are ultraviolet radiation, nerve damage, sun exposure, and cervical spine problems. The triggering factors for notalgia paresthetica are stress, anxiety, and certain medicines like antidepressants, opioids, angiotensin-converting enzyme inhibitors, and muscle relaxants. Symptoms of both diseases are similar, but there is more stinging and burning of your skin in the brachioradial pruritus as compared to the notalgia paresthetica, and the use of capsaicin cream has more effective results in the brachioradial pruritus as compared to the notalgia paresthetica.8Steinke, S., Gutknecht, M., Zeidler, C., Dieckhöfer, A. M., Herrlein, O., Lüling, H., Ständer, S., & Augustin, M. (2017). Cost-effectiveness of an 8% Capsaicin Patch in the Treatment of Brachioradial Pruritus and Notalgia Paraesthetica, Two Forms of Neuropathic Pruritus. Acta dermato-venereologica, 97(1), 71–76. https://doi.org/10.2340/00015555-2472
Can a Spinal Cord Tumour cause Brachioradial Pruritus?
Yes, a spinal cord tumor can also cause this condition if it involves your cervical dermatomes. There has been a case where a spinal cord tumor involved dermatomes between the fifth and sixth cervical spine presented with brachioradial pruritus.9Kavak, A., & Dosoglu, M. (2002). Can a spinal cord tumor cause brachioradial pruritus?. Journal of the American Academy of Dermatology, 46(3), 437–440. https://doi.org/10.1067/mjd.2002.113674
Conclusion
Brachioradial pruritus is a skin condition caused by nerve damage or cervical spine problems. Its common symptoms are itching, crusting, burning, numbness, and paraesthesia of the forearm. Steroids, local anesthetics, capsaicin, anticonvulsants, and nerve blocks are used to treat it. If it is not treated on time, it can become chronic and cause many other complications.
Refrences
- 1Pinto, A. C., Wachholz, P. A., Masuda, P. Y., & Martelli, A. C. (2016). Clinical, epidemiological and therapeutic profile of patients with brachioradial pruritus in a reference service in dermatology. Anais brasileiros de dermatologia, 91(4), 549–551. https://doi.org/10.1590/abd1806-4841.201644767
- 2Marziniak, M., Phan, N. Q., Raap, U., Siepmann, D., Schürmeyer-Horst, F., Pogatzki-Zahn, E., Niederstadt, T., & Ständer, S. (2011). Brachioradial pruritus as a result of cervical spine pathology: the results of a magnetic resonance tomography study. Journal of the American Academy of Dermatology, 65(4), 756–762. https://doi.org/10.1016/j.jaad.2010.07.036
- 3Sommer, F., Hensen, P., Böckenholt, B., Metze, D., Luger, T. A., & Ständer, S. (2007). Underlying diseases and co-factors in patients with severe chronic pruritus: a 3-year retrospective study. Acta dermato-venereologica, 87(6), 510–516. https://doi.org/10.2340/00015555-0320
- 4Medical Pearl: The ice-pack sign in brachioradial pruritus Bernhard, Jeffrey D. et al. Journal of the American Academy of Dermatology, Volume 52, Issue 6, 1073
- 5Pereira, M. P., Lüling, H., Dieckhöfer, A., Steinke, S., Zeidler, C., Agelopoulos, K., & Ständer, S. (2018). Application of an 8% capsaicin patch normalizes epidermal TRPV1 expression but not the decreased intraepidermal nerve fiber density in patients with brachioradial pruritus. Journal of the European Academy of Dermatology and Venereology: JEADV, 32(9), 1535–1541. https://doi.org/10.1111/jdv.14857
- 6Yilmaz, S., Ceyhan, A. M., & Baysal Akkaya, V. (2010). Brachioradial pruritus successfully treated with gabapentin. The Journal of Dermatology, 37(7), 662–665. https://doi.org/10.1111/j.1346-8138.2010.00830.x
- 7Wachholz, P. A., Masuda, P. Y., Pinto, A. C. V. D., & Martelli, A. C. C. (2017). Impact of drug therapy on brachioradial pruritus. Anais brasileiros de dermatologia, 92(2), 281–282. https://doi.org/10.1590/abd1806-4841.20175321.
- 8Steinke, S., Gutknecht, M., Zeidler, C., Dieckhöfer, A. M., Herrlein, O., Lüling, H., Ständer, S., & Augustin, M. (2017). Cost-effectiveness of an 8% Capsaicin Patch in the Treatment of Brachioradial Pruritus and Notalgia Paraesthetica, Two Forms of Neuropathic Pruritus. Acta dermato-venereologica, 97(1), 71–76. https://doi.org/10.2340/00015555-2472
- 9Kavak, A., & Dosoglu, M. (2002). Can a spinal cord tumor cause brachioradial pruritus?. Journal of the American Academy of Dermatology, 46(3), 437–440. https://doi.org/10.1067/mjd.2002.113674





