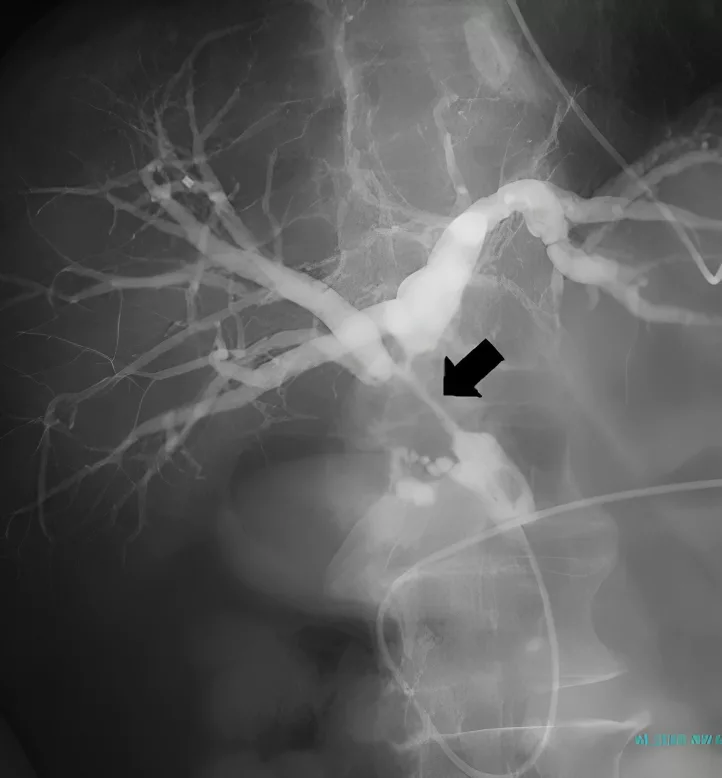
Cholangiography is a technique that your doctor uses to take images of the biliary tree with the help of X-rays after injecting a contrast medium into it. It plays an important role in the diagnosis and management of various biliary tree pathologies.
What Is Cholangiography?
Cholangiography is a procedure for imaging your biliary tree with X-rays after injecting some contrast medium into it. The doctors have been performing this procedure for over forty years.1Hatzidakis, A., Venetucci, P., Krokidis, M., & Iaccarino, V. (2014). Percutaneous biliary interventions through the gallbladder and the cystic duct: What radiologists need to know. Clinical radiology, 69(12), 1304–1311. https://doi.org/10.1016/j.crad.2014.07.016
It provides access to the intrahepatic (inside the liver) and to the extrahepatic biliary tree, which is helpful for the diagnosis as well as management of various pathologies. Endoscopic retrograde cholangiography (ERCP) and, magnetic resonance cholangiography (MRCP), percutaneous cholangiopancreatography (PTC) have been very helpful for diagnosing and managing various diseases affecting your liver, gallbladder, and pancreas.
Types Of Cholangiography
The following are types of cholangiography:
Endoscopic Retrograde Cholangiopancreatography (ERCP):
It is also an imaging technique that uses an endoscope through your bile ducts. ERCP has a camera for imaging. It has diagnostic as well as therapeutic indications, like the diagnosis of tumors and stones in the pancreatic ducts and their removal.
Magnetic Resonance Cholangiopancreatography (MRCP):
It uses magnetic rays to visualize your bile and pancreatic ducts. It is very helpful to check gallstones in your ducts.
Percutaneous Cholangiopancreatography (PTC):
PTC is used to visualize your liver and bile ducts with the help of X-rays. Your doctor performs it by inserting a needle in your liver to see and remove the blockage in your liver and bile ducts.
Computed Tomography (CT Cholangiography):
In computed tomography Cholangiography, your doctor takes a series of images using the computed tomography technique.
Indications Of Cholangiography
There are diagnostic as well as therapeutic indications of cholangiography. These are:
Diagnostic Indications:
Diagnostic indications of cholangiography are:
- Biliary tree obstruction
- Jaundice
- Inflammation of your biliary tree
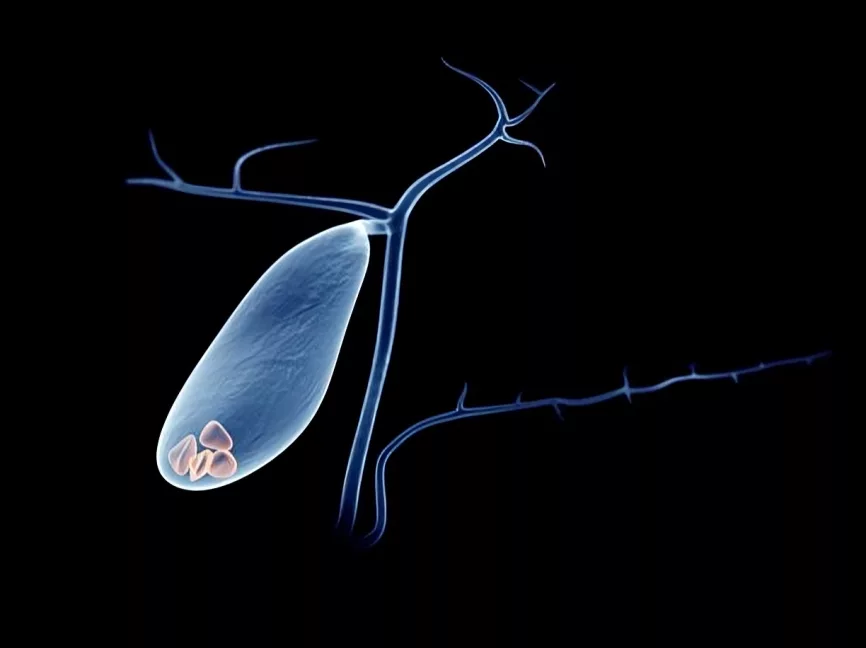
- Gallbladder stones
- Strictures in the bile duct
- Abdominal pain
- Evaluation after liver transplant like post-transplant biliary leakage2Marth, A. A., Auer, T. A., Walter-Rittel, T. C., Nevermann, N., Krenzien, F., Schmelzle, M., Müller, T., Kolck, J., Wieners, G., Geisel, D., Gebauer, B., Hamm, B., Schöning, W., & Fehrenbach, U. (2023). Gd-EOB-DTPA-MRCP to localize bile leakage after liver trauma and surgery: impact on treatment and outcome. European radiology, 33(9), 5933–5942. https://doi.org/10.1007/s00330-023-09608-x
Therapeutic Indications:
The doctors recommend cholangiography for the following therapeutic indications:
- Removal of gallstones
- Removal of biliary tree strictures
- Drainage of your biliary system
- Bile duct stunting
- Recurrent pancreatitis
- History of trauma to the biliary tree
- Cholangiocarcinoma
- Chronic pancreatitis
Which Patients are fit for Cholangiography?
Patients who are fit for cholangiography include:
- Adult patients aged more than five years
- Vitally stable patients
- Patients with normal renal function because contrast medium is harmful to your kidneys. It worsens your chronic kidney disease.
- Patients who are non-allergic to contrast medium because contrast medium can cause a severe reaction if you are allergic to it.
Contraindications Of Cholangiography
The following are contraindications of Cholangiography:
- Patients having impaired renal function
- Pregnancy
- Bleeding disorders
- Vitally unstable patient
- Patients with chronic kidney disease
- History of allergy to the contrast medium
- Severe cardiac disease
- If you have an allergy to iodine (which your doctor uses as a contrast medium)
- If you have asthma or chronic obstructive pulmonary disease (COPD)
Equipment used in Cholangiography
Cholangiography is a procedure that has diagnostic and therapeutic uses. While performing cholangiopancreatography, your doctor’s first priority is to make it the least invasive. That’s why they use minimally invasive techniques. They use various equipment in Cholangiography. These are:3Saad W. E. (2008). Transhepatic techniques for accessing the biliary tract. Techniques in vascular and interventional radiology, 11(1), 21–42. https://doi.org/10.1053/j.tvir.2008.05.004
Imagining Equipment:
- Computed tomography machine for computed tomography Cholangiography
- Magnetic resonance imaging MRI machine for magnetic resonance cholangiopancreatography
- Endoscope and a camera for endoscopic retrograde cholangiopancreatography.

Contrast Medium:
Your doctors use iodinated contrast mediums like iohexol and iopamidol as well as non-iodinated contrast medium like gadolinium-based contrast medium for cholangiography.
Other Equipment:
Endoscopic retrograde cholangiopancreatography requires equipment like:
- Duodenoscope
- Guidewires
- Balloons
- Stents
- Catheters.
Moreover, your doctors use protective equipment like:
- Lead aprons
- Lead gloves
- Protective shields.
In addition, monitoring equipment is needed, which includes a blood pressure cuff, electrocardiography, and pulse oximeter.
How to Prepare a Patient for Cholangiography?
The following are steps for the preparation of a patient for Cholangiography:
History:
Your doctor may ask the following questions:
- Do you have any cardiac or kidney disease or history of any cardiac disease or kidney problem like chronic kidney disease in your family?
- Have you been through this type of investigation before? Do you have a history of allergy to any type of contrast medium or any medicine?
- Do you have any bleeding disorders or a history of family members having any bleeding disorders?
- Do you have any other illnesses like cirrhosis of the liver, pancreatitis, pancreatic cancer, human Immunodeficiency Virus (HIV), or immunodeficiency?
Examination:
After a complete history, your doctor will perform a complete general physical examination. He will particularly focus on your gastrointestinal tract examination.
Investigations:
Your doctor will advise you on the following investigations before Cholangiography:
- Complete blood count (CBC)
- Liver function tests (LFTs)
- Renal function tests (RFTs)
- Complete urine examination
- Serum electrolytes
- Pancreatic enzymes (pancreatic amylase and lipase levels)
- Infection screening
- Human Immunodeficiency Virus (HIV) screening
- Viral markers (Hepatitis B and C screening particularly)
- Bleeding time, clotting time, Prothrombin time (PT), Activated Partial thromboplastin time (APTT), and International normalized ratio (INR). Your doctor corrects any abnormality in any of them.4Patel, I. J., Davidson, J. C., Nikolic, B., Salazar, G. M., Schwartzberg, M. S., Walker, T. G., Saad, W. A., & Standards of Practice Committee, with Cardiovascular and Interventional Radiological Society of Europe (CIRSE) Endorsement (2012). Consensus guidelines for periprocedural management of coagulation status and hemostasis risk in percutaneous image-guided interventions. Journal of vascular and interventional radiology: JVIR, 23(6), 727–736. https://doi.org/10.1016/j.jvir.2012.02.012
Prophylactic Antibiotics:
Antibiotic prophylaxis is important before performing cholangiography as it protects against a wide range of bacteria. Your doctor might advise you to take antibiotics thirty minutes before the procedure and ask you to continue them twenty-four to forty hours after the surgery.
Doctors usually advise ceftriaxone, metronidazole, and ciprofloxacin before the procedure. Antibiotic prophylaxis is very important for high-risk patients, such as immunocompromised patients, people with biliary tree obstruction, and those with liver disease.
What Precautions Should You Follow Before Cholangiography?
You should follow the following precautions before Cholangiography:
- Don’t eat or drink anything six to eight hours before the procedure.
- Remove any kind of jewelry or metallic materials.
- Wear comfortable dresses.
- Inform your doctors if you have any illness, about the medication you are taking, or if you have an allergy to any medicine or contrast medium they use during the procedure.
Step-by-Step Procedure for Cholangiography
The following are steps of different types of Cholangiography:
Percutaneous Cholangiography:
In percutaneous cholangiography, doctors use various techniques to look into your biliary tree with the help of fluoroscopic guided needles, snares, or wires. They may perform procedures under ultrasound guidance. The doctor asks you to lie in the supine position, and the anesthetist gives you local anesthesia along with moderate sedation. After this, they insert the catheter through the mid-axillary line, advance it, and when it reaches the bile duct, they inject the contrast medium and take images via X-rays. Then, they drain the ducts, remove the stricture, or stent it, depending on the diagnosed pathology shown on the cholangiogram.
Magnetic Resonance Cholangiopancreatography (MRCP):
Fasting for four hours is necessary for magnetic resonance cholangiopancreatography to reduce your bowel movements. Your doctors make you lie supine and introduce a contrast medium like gadolinium intravenously. Then, they place an array coil on your abdomen and take a series of images. They take images in the coronal and sagittal plane by T2 weighted sequence. The fluids appear dark in these images, while the solid tissues like your liver and pancreas appear bright. It provides a visualization of your biliary tree.
Moreover, three-dimensional magnetic resonance cholangiopancreatography is helpful in visualizing your biliary tree during reconstruction.
Endoscopic Retrograde Cholangiopancreatography (ERCP):
Endoscopic retrograde cholangiopancreatography is a minimally invasive procedure that uses an endoscopic approach along with fluoroscopy. The doctors make you lie in a prone or left lateral position and administer sedatives and analgesics. Then, they insert an endoscope through your mouth and advance through the esophagus, stomach, and into the duodenum, where the ampulla of Vater (the opening where the bile and pancreatic ducts empty into the small intestine) is located. After localization, they insert a cannula and guide wire to inject a contrast medium to visualize the ducts. Your doctor can visualize your bile ducts and remove any kind of stones, strictures, obstruction, or mass.
Computed Tomography Cholangiography (CT Cholangiography):
In computer tomography cholangiography, your doctors use the computed tomography technique. They inject about ten to twenty milliliters of iodinated contrast medium in your veins and make you lie supine thirty minutes later. They take an image of your liver and pancreas.
Arterial Visualization
After the first image, your doctor takes images in the arterial phase (twenty to thirty seconds after the initial image), in which your arteries are filled with blood.
Venous Visualisation
In the next sixty to seventy seconds, there is a venous phase in which the veins are engorged with blood, and the doctor can see the image of your vein.
Delayed Phase
In the next phase, which is the delayed phase, your doctor visualizes your bile duct. This phase is usually three to five minutes after the venous phase.
The doctors take images in the coronal, sagittal as well as three-dimensional planes.
What Post Operative Or Recovery Care Is Needed After Cholangiography?
After cholangiography, your doctors provide you with proper post-operative care. They monitor you for some time for complications like infection, bleeding, hematoma, hypertension or hypotension, and oxygen saturation. They give you analgesics for pain. Then, they provide you with a proper follow-up plan and ensure that there are no complications and that you are healing properly.
In addition, your doctors will monitor you for allergic reactions to the contrast agent.
Cholangiography Versus Cholangiogram:
Cholangiography is the procedure in which your doctor uses a contrast medium to diagnose as well as treat biliary tree pathologies like lesions, stones, and obstructions, while Cholangiogram is the resultant graph that your doctor obtains while performing cholangiography.
Cholangiogram provides a complete visual representation of your bile ducts to your doctor. It shows structures in your bile ducts, cystic ducts, common bile ducts, pancreatic ducts, and hepatic ducts.
Hence, it is helpful to your doctor in the detection of biliary cirrhosis, gallstones, strictures, obstructions, tumors, and other abnormalities. Moreover, your doctor can use the information obtained from the cholangiogram for stunting, removal of cholangiocarcinoma, gallstones removal, strictures removal, and treating chronic pancreatitis.
Complications Of Cholangiography
Cholangiography can result in very severe complications. The main causes of these complications include improper technique, an inexperienced person performing the procedure, or a lack of antibiotic prophylaxis before the procedure. Moreover, if you have a malignant disease, you have more chances of developing complications than those with benign diseases.5Yee, A. C., & Ho, C. S. (1987). Complications of percutaneous biliary drainage: benign vs malignant diseases. AJR. American Journal of roentgenology, 148(6), 1207–1209. https://doi.org/10.2214/ajr.148.6.1207
The following are complications of Cholangiography procedures:
Severe bleeding:
Severe bleeding mostly occurs due to faulty technique. It is necessary to control bleeding. If the bleeding is severe, your doctor may need to perform embolization to control the bleeding.
Allergy to Contrast Medium:
Some patients may develop an allergy to contrast medium, which can be a very life-threatening condition. It requires immediate management.
Worsening of Kidney Disease:
Cholangiography worsens kidney disease as its contrast material is harmful to your kidneys.
Arterial hemobilia:
Arterial hemobilia (bleeding in the biliary tract) may occur in some patients. Its chances are 0.2 to 4 percent. It occurs due to communication of your biliary tract with some major vessel.6Winick, A. B., Waybill, P. N., & Venbrux, A. C. (2001). Complications of percutaneous transhepatic biliary interventions. Techniques in vascular and interventional radiology, 4(3), 200–206. https://doi.org/10.1016/s1089-2516(01)90026-5
Biliary Leak:
Bile may leak due to rupture of the bile ducts. Its common cause is faulty techniques by inexperienced people. It can be peritoneal or pleural leaks.
Pneumothorax:
Pneumothorax may occur during the introduction of the catheter in the biliary tract by right-sided approach. Sometimes, it even becomes necessary to pass a chest tube to such patients.7Saad, W. E., Wallace, M. J., Wojak, J. C., Kundu, S., & Cardella, J. F. (2010). Quality improvement guidelines for percutaneous transhepatic cholangiography, biliary drainage, and percutaneous cholecystostomy. Journal of vascular and interventional radiology: JVIR, 21(6), 789–795. https://doi.org/10.1016/j.jvir.2010.01.012
Cellulitis:
Cellulitis may occur due to infection of the skin. Other types of skin lesions may appear as well.
Infections & Cholangitis:
It is more common in endoscopic retrograde cholangiopancreatography because it allows the bacteria from your gut to enter the biliary tree. Moreover, it is more common in malignant diseases.8Yee, A. C., & Ho, C. S. (1987). Complications of percutaneous biliary drainage: benign vs malignant diseases. AJR. American Journal of roentgenology, 148(6), 1207–1209. https://doi.org/10.2214/ajr.148.6.1207
Can Cholangiography Help In The Diagnosis Of Pancreatic Cancer?
Yes, cholangiography can help in the diagnosis of pancreatic cancer. It visualizes the pancreatic and bile ducts to help your doctor check any kind of lesion inside the pancreas. However, it is not an investigation of choice for the diagnosis of pancreatic cancer.
Difference Between Magnetic Resonance Cholangiopancreatography & Endoscopic Retrograde Cholangiopancreatography?
Both magnetic resonance cholangiopancreatography and endoscopic retrograde cholangiopancreatography are useful in the diagnosis of lesions and masses in the bile duct, but endoscopic retrograde cholangiopancreatography has therapeutic indications as well. Your doctor can use it for removing gallstones, strictures and masses. Moreover, the doctors also use it to remove stones left in the common bile duct after cholecystectomy.
Endoscopic retrograde cholangiography is an invasive procedure which uses an endoscopic approach. In contrast, magnetic resonance cholangiopancreatography uses magnetic resonance imaging.
Conclusion
Cholangiography is a diagnostic as well as therapeutic procedure. It is used to diagnose biliary tract lesions, prolonged jaundice, strictures, masses, tumors, and gallstones and remove them. It has various types depending on why your doctor has recommended it. Moreover, cholangiography needs expert surgeons to avoid complications. However, if you experience any complications, immediately consult your doctor.
Refrences
- 1Hatzidakis, A., Venetucci, P., Krokidis, M., & Iaccarino, V. (2014). Percutaneous biliary interventions through the gallbladder and the cystic duct: What radiologists need to know. Clinical radiology, 69(12), 1304–1311. https://doi.org/10.1016/j.crad.2014.07.016
- 2Marth, A. A., Auer, T. A., Walter-Rittel, T. C., Nevermann, N., Krenzien, F., Schmelzle, M., Müller, T., Kolck, J., Wieners, G., Geisel, D., Gebauer, B., Hamm, B., Schöning, W., & Fehrenbach, U. (2023). Gd-EOB-DTPA-MRCP to localize bile leakage after liver trauma and surgery: impact on treatment and outcome. European radiology, 33(9), 5933–5942. https://doi.org/10.1007/s00330-023-09608-x
- 3Saad W. E. (2008). Transhepatic techniques for accessing the biliary tract. Techniques in vascular and interventional radiology, 11(1), 21–42. https://doi.org/10.1053/j.tvir.2008.05.004
- 4Patel, I. J., Davidson, J. C., Nikolic, B., Salazar, G. M., Schwartzberg, M. S., Walker, T. G., Saad, W. A., & Standards of Practice Committee, with Cardiovascular and Interventional Radiological Society of Europe (CIRSE) Endorsement (2012). Consensus guidelines for periprocedural management of coagulation status and hemostasis risk in percutaneous image-guided interventions. Journal of vascular and interventional radiology: JVIR, 23(6), 727–736. https://doi.org/10.1016/j.jvir.2012.02.012
- 5Yee, A. C., & Ho, C. S. (1987). Complications of percutaneous biliary drainage: benign vs malignant diseases. AJR. American Journal of roentgenology, 148(6), 1207–1209. https://doi.org/10.2214/ajr.148.6.1207
- 6Winick, A. B., Waybill, P. N., & Venbrux, A. C. (2001). Complications of percutaneous transhepatic biliary interventions. Techniques in vascular and interventional radiology, 4(3), 200–206. https://doi.org/10.1016/s1089-2516(01)90026-5
- 7Saad, W. E., Wallace, M. J., Wojak, J. C., Kundu, S., & Cardella, J. F. (2010). Quality improvement guidelines for percutaneous transhepatic cholangiography, biliary drainage, and percutaneous cholecystostomy. Journal of vascular and interventional radiology: JVIR, 21(6), 789–795. https://doi.org/10.1016/j.jvir.2010.01.012
- 8Yee, A. C., & Ho, C. S. (1987). Complications of percutaneous biliary drainage: benign vs malignant diseases. AJR. American Journal of roentgenology, 148(6), 1207–1209. https://doi.org/10.2214/ajr.148.6.1207