Dracunculiasis, or Guinea-worm disease, is a waterborne parasitic illness characterized by the emergence of a long, thread-like worm from the skin in the lower limbs. It presents with local symptoms such as blisters, pain, edema at the emergence site, and systemic manifestations such as fever, rash, diarrhea, and vomiting. Transmission occurs through the ingestion of stagnant water contaminated with copepods (water fleas) that carry infective larvae. Following ingestion, the larvae are released, penetrate the intestinal wall, and mature in the body. Owing to meticulous efforts by the Carter Center and WHO, this disease is currently on the verge of eradication.1Guinea worm case totals. (n.d.). The Carter Center. https://www.cartercenter.org/health/guinea_worm/case-totals.html However, its disabling effects still make it a major public health concern in vulnerable communities.

Causes of Dracunculiasis
Dracunculiasis is caused by a parasite called Dracunculus medinensis that belongs to the nematode or roundworm family. It’s the largest human parasite, with females growing as long as 60-100cm in length.
Lifecycle of Dracunculus Medinensis:
In the lifecycle of Dracunculus medinensis, humans are the definitive host, while water fleas of the Cyclops genus (a type of copepod) act as the intermediate host.
When the gravid female worm comes into contact with water, she releases first-stage larvae (L1) into the environment. These larvae are ingested by water fleas, where they develop into infective third-stage larvae (L3) over about 2 weeks.
When a human drinks unfiltered water containing these infected copepods, the copepods are killed by stomach acid, releasing the L3 larvae. These larvae penetrate the intestinal wall, enter the abdominal cavity and retroperitoneal space, and mature into adult worms over 2–3 months. Males die shortly after mating, which is why only females are typically recovered from infected individuals.
The fertilized female migrates through the body tissues to the subcutaneous tissue, usually of the lower limbs, where she causes a painful blister. When this blister comes in contact with water, the female emerges and releases larvae, continuing the cycle.2Rawla, P., & Jan, A. (2023, August 22). Dracunculiasis. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK538231/

How is Dracunculiasis Transmitted?
The primary mode of transmission in Dracunculiasis is through drinking contaminated water. According to evidence, the larvae of Dracunculus go through multiple phases of molting inside the cyclops fleas.
- The first larval stage, i.e, the stage that adult females release, is purely non-infective. Neither does it cause any disease, nor can it survive more than 3 days without a host.
- After water fleas ingest them, these larvae undergo the process of molting twice, transforming into the second and then the third larval stage.
- The third larval stage is the infective one. It cannot form except in a freshwater environment, therefore, scientists believe waterborne transmission is the only definitive mode of transmission for this illness
According to some other evidence, dogs and fish also act as intermediate hosts in the lifecycle of this parasite.3Cleveland, C. A., Eberhard, M. L., Thompson, A. T., Smith, S. J., Zirimwabagabo, H., Bringolf, R., & Yabsley, M. J. (2017). Possible Role of Fish as Transport Hosts for Dracunculus spp. Larvae. Emerging infectious diseases, 23(9), 1590–1592. https://doi.org/10.3201/eid2309.161931 . Dogs consume infected fish, and later, their bodies release the parasitic larvae into water, continuing the lifecycle discussed earlier.
Another route of transmission might be through the ingestion of infected fish by humans. Epidemiologists believe this might be the reason that the eradication of disease in African countries like Chad is still challenging.4Molyneux, D., & Sankara, D. P. (2017). Guinea worm eradication: Progress and challenges- should we beware of the dog?. PLoS neglected tropical diseases, 11(4), e0005495. https://doi.org/10.1371/journal.pntd.0005495
How common is Dracunculiasis?
Dracunculiasis is one of the oldest known diseases, with references dating back to ancient Egyptian texts of 1550 BCE. It used to be prevalent in Africa and Asia earlier, with 3.5 million cases occurring annually in 1986, throughout twenty different countries.5Hopkins, D. R., Ruiz-Tiben, E., Eberhard, M. L., Weiss, A., Withers, P. C., Roy, S. L., & Sienko, D. G. (2018). Dracunculiasis Eradication: Are We There Yet?. The American journal of tropical medicine and hygiene, 99(2), 388–395. https://doi.org/10.4269/ajtmh.18-0204 Now, thanks to public health measures and global eradication programs, the incidence has dropped to only 14 human cases reported worldwide.6Hopkins DR, Weiss AJ, Yerian S, Zhao Y, Sapp SG, Cama VA. Progress Toward Global Dracunculiasis (Guinea Worm Disease) Eradication, January 2023–June 2024. MMWR Morb Mortal Wkly Rep 2024;73:991–998. DOI: http://dx.doi.org/10.15585/mmwr.mm7344a1. Epidemiologists label it as the second disease eradicated solely based on preventative measures, after smallpox.
Who is at risk for Dracunculiasis?
Even though this disease is now restricted to a narrow belt of rural areas in some countries of Africa, some individuals are at a higher risk than others of contracting it. These include:
- People in endemic areas who depend upon contaminated water sources for their everyday needs.
- Young adults, who may be more exposed to contaminated water bodies, owing to their work or activities.
- Workers in the Agriculture sector, especially farmers and herders, are more vulnerable as they may consume unfiltered water while being away from home
- Individuals responsible for fetching drinking water from contaminated sources are also at an increased risk.
Symptoms of Dracunculiasis
The symptoms of dracunculiasis consist of an initial asymptomatic period, followed by nonspecific systemic symptoms and then localized manifestations correlating with worm emergence.
Initial Phase:
Patients do not experience any symptoms initially, despite the larvae being inside the human body. It’s the period when larvae are maturing into adult parasites. This phase usually lasts for a year.
Non-specific Prodromal Phase:
While the larvae mature, mate, and migrate towards the skin, patients start experiencing nonspecific symptoms such as:
- Fever
- Nausea
- Vomiting
- Diarrhea
- Allergic reactions such as hives, wheezing, respiratory distress, etc
These symptoms symbolize the immune response of the human body against the foreign parasite.
Characteristic Manifestations upon Worm Emergence:
Once the migration is complete and the female parasite has reached the skin, you might experience the following localized symptoms:
- Blister formation
- Intense pain
- Itching and burning sensation
- Edema
- Ulcer formation
The worm may take even up to 8 weeks to emerge, keeping the patient in incapacitating pain til then. There might be an emergence of more than one worm at a time.

Complications of Dracunculiasis:
The worm may migrate to other parts of the body, causing pains and complications there, such as:
- Secondary abscess formation in the pericardium, lungs, or the spinal cord: This happens when the worm migrates to respective sites in the body.
- Secondary bacterial infections: This is the most common complication. Ulcers formed in dracunculiasis are frequently infected with bacteria. These infections can progress to abscess formation, cellulitis, or even sepsis.
- Joint pain, contracture formation, or septic arthritis: These symptoms develop during worm migration through the joints.
- Sepsis: It’s a life-threatening systemic reaction that develops when secondary bacterial infections from the parasite’s exit site enter our bloodstream. Note that it’s a medical emergency, and you need to seek immediate medical attention if you experience any of the following:
- High-grade fever
- Chills
- Rapid breathing
- Racing heart rate
- Confusion or dizziness
- Cellulitis: It’s the diffuse inflammation below the skin, often occurring secondary to worm breakage inside the subcutaneous region.
- Chronic pain and swelling: If the worm dies before emerging, it becomes encapsulated and calcified, producing recurrent pain and swelling.
- Recurrent infections: Since there is no acquired immunity to dracunculiasis, people who catch it once are prone to getting it again and again.
- Disability: The symptoms and complications of dracunculiasis are severely debilitating. Patient often experience temporary or even permanent disability, severely impacting their quality of life.
How to diagnose Dracunculiasis?
Doctors diagnose dracunculiasis primarily upon clinical symptoms, identification of the emerging worm, and differentiation from other ulcerative skin conditions
History:
Your doctor will take a thorough history, exploring the duration, intensity, and progression of your symptoms. In case he suspects dracunculiasis, he may also inquire about
- Travel history to the endemic area
- Ingestion of contaminated water
- Consumption of fruits/vegetables washed with such water
- Bathing or swimming in potentially contaminated water sources
Physical Examination:
After a thorough history, your doctor will move forward towards a local and general physical examination:
- The general look of a patient with dracunculiasis may be characterized by extreme pain, distress, and irritability due to the disabling manifestations of the disease.
- Vital signs may reveal a high body temperature, tachycardia, tachypnea, or other signs or allergic reactions
- Local examination would reveal a blister, abscess, or ulcer on the lower extremity. The blister may be erythematous around the edges. As the worm reaches near the skin, the blister may increase in size and finally erupt, allowing for the worm to exit. Your doctor might also observe edema around the lesion.
- Once the blister erupts, the worm is also visible through the consequent ulcer. This identification of the worm head confirms a diagnosis of dracunculiasis
- The rest of the physical examination is generally unremarkable, except for the presence of occasional lymphadenopathy in some regions
Laboratory Tests & Imaging Studies:
Right now, there isn’t any reliable lab test to diagnose Dracunculiasis. Non-specific lab findings may include:
- A raised white blood cell count on the Blood Complete Picture.
- Differential White Blood Cell count may show eosinophilia.
- Doctors might notice elevated levels of IgE and IgG immunoglobulins.
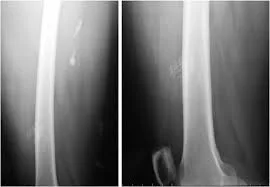
- Imaging may reveal calcified, encapsulated, dead worms.
But all these findings are non-conclusive, and the mainstay of diagnosis is always clinical.
What is the treatment for Dracunculiasis?
The treatment of choice for Dracunculiasis is the removal of the worm and supportive therapies. There is no definitive medical cure for this disease to date.
Supportive Therapy:
- The doctor may advise you to take painkillers such as aspirin or ibuprofen to ease the pain and associated swelling.
- You will need to apply topical antibiotics to the site of the primary lesion. These help prevent secondary bacterial infections.
- Most probably, you won’t require any systemic antibiotics unless there is evidence of sepsis or cellulitis.
- Your doctor might also prescribe antihistamines such as diphenhydramine to soothe the itching.
- Anti-parasitic agents such as metronidazole have a limited efficacy in the treatment of Dracunculiasis.7A. Issaka-Tinorgah, P. Magnussen, P. Bloch, A. Yakubu, Lack of effect of ivermectin on prepatent guinea-worm: a single-blind, placebo-controlled trial, Transactions of The Royal Society of Tropical Medicine and Hygiene, Volume 88, Issue 3, May 1994, Pages 346–348, https://doi.org/10.1016/0035-9203(94)90111-2 Doctors might recommend them as an adjunct to surgical excision, to accelerate worm migration. But, some evidence suggests that these antiparasitic medications do more harm than good–they cause abnormal migration of worms to sites other than the skin in the body. This increases the likelihood of consequent complications.8Jean-Philippe Chippaux, Mebendazole treatment of dracunculiasis, Transactions of The Royal Society of Tropical Medicine and Hygiene, Volume 85, Issue 2, March-April 1991, Page 280, https://doi.org/10.1016/0035-9203(91)90056-5
- Apart from this, you should also consult an infectious disease specialist to help with management and follow-up care.
- The hospital staff should inform public health authorities and comply with epidemiological protocol, especially when a patient reports in a non-endemic area.
Medical Procedure for Worm Extraction in Dracunculiasis:
The traditional worm extraction or the stick method is the definitive treatment for dracunculiasis. Here is a detailed breakdown of this process:
- The potential exit site of the worm is marked by the presence of a blister. If you have one, your doctor will advise you to soak that area in water. This not only helps soothe the irritation but also speeds up the worm emergence process.
- When the worm is about to emerge, the blister erupts, forming an ulcer there, with a whitish worm head popping up in its centre. Once this happens, doctors start the extraction process by wrapping the worm around a stick or a gauze piece. This helps maintain that tension and prevents the worm from slipping back.
- Then, doctors slowly pull the worm out, a few centimeters at a time. Remember, this is a lengthy and painful process that may take days to weeks to complete.
- Healthcare professionals execute this whole process in an aseptic environment with sterilized apparatus to minimize the risk of secondary infections. Once the extraction is complete, doctors clean the wound, apply topical antibiotics, and prescribe medicines to help with pain and inflammation.
- Another alternative method is the surgical extraction of the worm. It’s done under local anesthesia. Surgeons usually give a nick in the skin to access the worm. The next steps are similar to those described above.
- Doctors also advise the patients to avoid shared water sources throughout this process, to prevent the disease from spreading any further.

Can I die from Dracunculiasis?
No, dracunculiasis is rarely fatal. But due to the incapacitating pain and disabling complications, it can severely affect your quality of life. Especially in cases when it affects the joints, you might end up with permanent or at least temporary disability, costing you months of work time or school life.
How to prevent Dracunculiasis?
There is no vaccine available for Dracunculiasis. The primary preventative strategy is the provision of safe drinking water and community health education to break the chain of transmission.
- Populations at risk should have access to safe drinking water. This can be done by offering piped water systems, boreholes, protected springs, etc, to make sure there is no contact with potentially contaminated water that might be harbouring infected water fleas.
- Water filtration techniques employing portable filters with a minimum pore size of 150 μm should be made widely available.
- People in endemic areas need to be educated about safe water practices and about avoiding consuming unfiltered or potentially contaminated water.
- Patients should be made aware of the community risks of re-entering water sources while they are still infected.
- Temephos, a WHO-approved chemical larvicide, can also be used to eliminate copepods from stagnant water bodies.9Grunert, R., Box, E., Garrett, K., Yabsley, M., & Cleveland, C. (2022). Effects of Temephos (Abate®), Spinosad (Natular®), and Diflubenzuron on the Survival of Cyclopoid Copepods. The American journal of tropical medicine and hygiene, 106(3), 818–822. https://doi.org/10.4269/ajtmh.21-0818
- Active surveillance and prompt case containment should be made a priority.
Conclusion
Dracunculiasis is a parasitic illness that causes significant morbidity and disability. It presents with painful blisters, ulcers, and abscesses, especially at the worm’s exit site. The diagnosis is primarily clinical. There is no definitive cure for it yet, except for the daunting process of worm extraction. The prevention is focused on community health education and safe water supply. Despite its near-eradication status, it still poses public health concerns in areas where it is endemic, necessitating intensifying the final efforts to get our planet free of guinea-worm disease.
Refrences
- 1Guinea worm case totals. (n.d.). The Carter Center. https://www.cartercenter.org/health/guinea_worm/case-totals.html
- 2Rawla, P., & Jan, A. (2023, August 22). Dracunculiasis. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK538231/
- 3Cleveland, C. A., Eberhard, M. L., Thompson, A. T., Smith, S. J., Zirimwabagabo, H., Bringolf, R., & Yabsley, M. J. (2017). Possible Role of Fish as Transport Hosts for Dracunculus spp. Larvae. Emerging infectious diseases, 23(9), 1590–1592. https://doi.org/10.3201/eid2309.161931 .
- 4Molyneux, D., & Sankara, D. P. (2017). Guinea worm eradication: Progress and challenges- should we beware of the dog?. PLoS neglected tropical diseases, 11(4), e0005495. https://doi.org/10.1371/journal.pntd.0005495
- 5Hopkins, D. R., Ruiz-Tiben, E., Eberhard, M. L., Weiss, A., Withers, P. C., Roy, S. L., & Sienko, D. G. (2018). Dracunculiasis Eradication: Are We There Yet?. The American journal of tropical medicine and hygiene, 99(2), 388–395. https://doi.org/10.4269/ajtmh.18-0204
- 6Hopkins DR, Weiss AJ, Yerian S, Zhao Y, Sapp SG, Cama VA. Progress Toward Global Dracunculiasis (Guinea Worm Disease) Eradication, January 2023–June 2024. MMWR Morb Mortal Wkly Rep 2024;73:991–998. DOI: http://dx.doi.org/10.15585/mmwr.mm7344a1.
- 7A. Issaka-Tinorgah, P. Magnussen, P. Bloch, A. Yakubu, Lack of effect of ivermectin on prepatent guinea-worm: a single-blind, placebo-controlled trial, Transactions of The Royal Society of Tropical Medicine and Hygiene, Volume 88, Issue 3, May 1994, Pages 346–348, https://doi.org/10.1016/0035-9203(94)90111-2
- 8Jean-Philippe Chippaux, Mebendazole treatment of dracunculiasis, Transactions of The Royal Society of Tropical Medicine and Hygiene, Volume 85, Issue 2, March-April 1991, Page 280, https://doi.org/10.1016/0035-9203(91)90056-5
- 9Grunert, R., Box, E., Garrett, K., Yabsley, M., & Cleveland, C. (2022). Effects of Temephos (Abate®), Spinosad (Natular®), and Diflubenzuron on the Survival of Cyclopoid Copepods. The American journal of tropical medicine and hygiene, 106(3), 818–822. https://doi.org/10.4269/ajtmh.21-0818

