Ergotism is a serious medical condition caused by the consumption of toxic alkaloids produced by the fungus Claviceps purpurea. This fungus infects cereal grains, particularly rye, and produces compounds that can disrupt multiple body systems. The condition can also result from the misuse of ergot-derived medications, such as those used to treat migraines, or the consumption of contaminated grain in regions with poor storage conditions.1Puschner, B. (2020). Ergot alkaloids – toxicology and clinical significance. Journal of Veterinary Diagnostic Investigation, 32(2), 183–191.
https://doi.org/10.1177/1040638719895455
Ergotism presents in two distinct medical conditions, which impact separate body systems: gangrenous and convulsive. Blood vessel constriction from gangrenous ergotism results in tissue death, but convulsive ergotism triggers neurological symptoms that include seizures, together with hallucinations. The correct diagnosis and treatment of this condition requires understanding its dual nature.2Bove, F. J. (1970). The Story of Ergot. Karger Publishers.
Ergotism has gained new attention during the past few years because of growing interest in natural medicines and historical studies. Healthcare providers, especially in agricultural or rural settings, must remain vigilant for this condition.
Historical Significance & Modern Relevance:
Ergotism was historically known as St. Anthony’s Fire, referring to the burning sensations and severe pain experienced by sufferers. During the Middle Ages, multiple outbreaks devastated communities across Europe, where bread made from infected rye was a dietary staple.3Matossian, M. K. (1989). Poisons of the Past: Molds, Epidemics, and History. Yale University Press. While some researchers have speculated a link between ergot poisoning and the Salem witch trials (a series of prosecutions in 1692 Massachusetts where individuals, mostly women, were accused of witchcraft under mysterious physical and behavioral symptoms), this theory remains debated and is not widely accepted.
Ergotism occurs in modern times when people either take ergot-based medications too much or incorrectly use them for migraine treatment with ergotamine. The fungus exists sporadically in unregulated grain storage facilities, which are common in developing countries.
Causes & Sources of Ergotism
Ergot Fungus & Ergot Alkaloids:
The Claviceps purpurea fungus is a microscopic organism that causes ergotism. The pathogen attacks the flower-bearing ends of cereal grains, with rye being the primary target, although wheat and barley, and oats also become infected. The fungus thrives in humid storage conditions with improper grain storage practices to create dark, horn-shaped structures named sclerotia, which replace the grain kernels.
Common Sources of Exposure:
Ergotism exposure typically happens in one of two main ways:
- Dietary Exposure: Occurs when people eat bread or cereal made from contaminated grains. Historically, this was the main route of infection.
- Pharmaceutical Exposure: Seen today in individuals using ergot-derived medications such as:
- Ergotamine (used for migraines)
- Methylergometrine (used to control postpartum bleeding and pregnancy complications)
- Dihydroergotamine (used intravenously or nasally for headaches)

Other contributing factors that increase the risk of exposure include:
- Poor agricultural storage techniques
- Inadequate pharmaceutical regulation
- Ignorance of potential drug interactions
Recognizing Ergotism Symptoms
When people ingest large amounts, they develop acute symptoms that manifest as severe immediate reactions. A diagnosis of chronic ergotism becomes challenging because it emerges from prolonged low-dose exposure to ergot alkaloids.
Acute Symptoms:
- Nausea and vomiting start suddenly as the first symptoms appear.
- The limbs experience severe burning sensations and tingling effects.
- Rapid muscle spasms or seizures
- Cold extremities and loss of sensation
Chronic Symptoms:
- Persistent headaches
- The condition leads to mood swings that produce depression alongside anxiety symptoms.
- Poor circulation, especially in the fingers and toes
- Gradual loss of motor coordination
Gangrenous Ergotism:
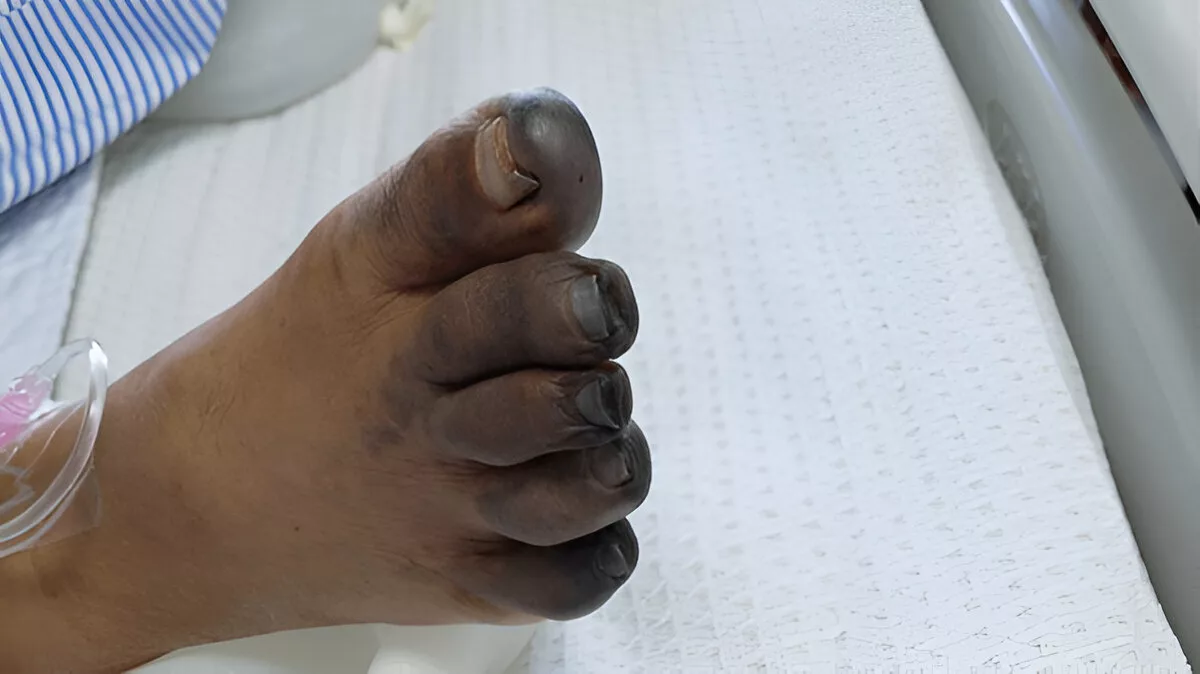
Ergot alkaloids trigger this type of ergotism because of their strong vasoconstrictive effects. The blood vessels constrict until blood flow becomes severely impaired, which causes tissue ischemia and necrosis.4Van Dongen, P. W. J., & de Groot, A. N. (1995). History of ergot alkaloids from ergotism to ergometrine. European Journal of Obstetrics & Gynecology and Reproductive Biology, 60(2), 109–116.
https://doi.org/10.1016/0028-2243(95)02247-7
Key signs include:
- Tingling or numbness in the extremities
- Skin that appears pale, cold, and eventually darkens
- Swelling and formation of blisters
- Severe pain followed by a loss of sensation
Patients may not realize the severity until irreversible tissue damage has occurred.
Convulsive Ergotism and Hallucinations:
Convulsive ergotism primarily affects the central nervous system. It was historically responsible for mass outbreaks of seizures, delusions, and hallucinations.5Smith, A. G., & Sullivan, J. B. (2003). Ergot alkaloids: Toxicologic overview and historical perspectives. Clinical Toxicology, 41(6), 807–811.
https://doi.org/10.1081/CLT-120024153
Typical symptoms include:
- Muscle twitching and tremors
- Intense, painful cramps
- Auditory or visual hallucinations
- Paranoia, mania, and confusion
- Sleep disturbances and disorganized speech
Diagnosing Ergotism
Clinical History & Symptom Assessment:
The following key steps are included in the history and examination:6Richard, J. L., & Bennett, G. A. (1999). Analysis of ergot alkaloids in livestock feed and human foods. Journal of AOAC International, 82(5), 1006–1012.
- Dietary habits – recent consumption of rye or grain-based products
- Geographical exposure – living in or traveling to areas with known ergot contamination
- Symptom onset and duration – gradual vs. sudden
- Neurological signs – visual disturbances, muscle spasms, seizures
- Circulatory issues – cold extremities, numbness, tingling, or gangrene
- Skin and limb assessment – looking for necrosis, especially in the digits
Laboratory & Toxicological Tests:
Once ergotism is suspected, lab tests can help confirm the diagnosis.
Tests may include:
- Blood serum analysis: Checking for markers of tissue necrosis, renal function, or electrolyte imbalance.
- Urine tests: To detect metabolites of ergot alkaloids.
- Tissue biopsies: In cases where gangrene is present, to assess the extent of necrosis.
- Grain or feed testing: For suspected dietary exposure, analyzing food samples is essential.7Panaccione, D. G. (2005). Ergot alkaloids: Genetics and evolution. Natural Product Reports, 22(5), 622–631.
https://doi.org/10.1039/B501995C
Differential Diagnosis of Ergotism
Ergotism can look strikingly similar to a number of other diseases and toxicological syndromes. This complicates diagnosis and increases the chance of inappropriate treatment.
Conditions commonly confused with ergotism include:
| Differential Diagnosis | Key Distinctions |
| Raynaud’s Phenomenon | Episodic vasospasm triggered by cold/stress, reversible |
| Vasculitis (e.g., Buerger’s) or bleeding disorders | Inflammatory vascular disease with systemic signs |
| Serotonin Syndrome | Hyperthermia, hyperreflexia, often medication-related |
| Neuroleptic Malignant Syndrome | Fever, rigidity, altered mental status, and medication history |
| Peripheral Arterial Disease | Atherosclerosis-related claudication and ischemia |
Ergotism Treatment Options
Discontinuation of Ergot Exposure:
The primary therapeutic step for treating ergotism requires removing the source that caused the condition. Patients should stop taking ergot-based drugs right away while they switch to food products that are free from contamination.
Key actions include:
- Discarding suspected food or grain supplies
- Withholding ergot-derived medications
- The digestive system needs to be flushed in the case of acute poisoning
- The exposed animals should be placed in isolation to monitor their health status
Even though patients stop their exposure to ergot alkaloids, their bodies will continue to show deteriorating symptoms due to the remaining toxins in their systems. Fast medical intervention plays a crucial role in reducing permanent tissue damage.
Medical & Supportive Therapies:
After the removal of the exposure source, supportive care takes precedence in the treatment process. The treatment plan depends on whether the patient has convulsive or gangrenous symptoms.
For Convulsive Ergotism:
- Anticonvulsants such as diazepam help control seizures.8Southwell, I. A., & Lowe, R. (1999). Natural Products in Australian Agriculture. CSIRO Publishing.
- Sedatives are prescribed for the management of agitation and hallucinations
- Intravenous fluids for hydration
- Nutritional support to correct imbalances
For Gangrenous Ergotism:
- Vasodilators help increase blood circulation (e.g., nitroprusside)9Schardein, J. L. (1993). Chemically Induced Birth Defects. CRC Press. [Details on the vasoconstrictive effects of ergot]
- Antiplatelet agents or anticoagulants to prevent blood clotting
- Pain management, often with opioids
- Surgical intervention that may include amputation
Ergot alkaloids lack an antidote for medical treatment. The need for supportive care and quick removal from exposure stands as the key factor for recovery success. Patients need extended therapy that last between weeks and months based on their condition’s severity.10Coulombe, R. A. (2003). Ergot alkaloids in agriculture and food: Toxicology and safety concerns. Toxicon, 42(4), 355–369.
https://doi.org/10.1016/S0041-0101(03)00244-4
Prevention Strategies
Agricultural & Food Safety:
The initial step of ergotism prevention happens on farms, and protection continues through all stages of food production. The grains, together with grasses, should maintain zero fungal contamination.
Best practices include:
- The use of disease-resistant grain varieties represents the most effective prevention method.
- The practice of crop rotation helps minimize fungal accumulation in the soil.
- Grains need to be properly dried and stored after harvest.
- Ergot sclerotia need to be inspected regularly in all feed and food products
Farmers, together with livestock owners, need to receive proper education. Farmers should recognize the appearance of infected grains, which appear as black, elongated, hard structures, to stop animals from consuming dangerous feed.
Medication Use & Monitoring:
Ergot-derived medications show effectiveness for migraine treatment as well as postpartum hemorrhage management and other medical conditions, yet they present certain dangers. Safe usage of these drugs requires following specific guidelines, which include:
- The patient needs to follow the prescribed dosing regimen precisely.
- The treatment duration should not exceed the recommended time frame.
- The patients should be aware of drug interactions (e.g., with antibiotics or antivirals)
- Regular monitoring for early symptoms
Healthcare providers need to teach patients about ergot poisoning warning signs while performing scheduled medication assessments, especially for elderly patients with circulatory issues.
Risk Factors for Developing Ergotism
Demographics & Health Conditions:
The combination of genetic factors with environmental conditions and health-related elements makes specific groups more likely to develop ergotism. The knowledge of risk profiles enables clinicians to take preventive measures before symptoms manifest.
High-risk groups include:
- Migraine patients who regularly take ergotamine or dihydroergotamine face a higher risk.
- Postpartum women require ergot-based medications for managing bleeding complications.
- The elderly population faces an increased risk because they experience poor circulation and their bodies react differently to medication.
- People with peripheral vascular disease: Ergot alkaloids exacerbate poor blood flow.
- The combination of specific medications, such as protease inhibitors with macrolide antibiotics and antifungals, leads to elevated ergot levels in the human body.
Poor health status, together with inadequate veterinary supervision and unregulated drug use, dramatically raises the danger level.
Geographic & Environmental Risk:
The risk areas are located in specific geographic locations:
- The growth of fungi flourishes best in temperate climates with high humidity levels
- Countries with less-regulated food safety systems
- Rural areas utilizing home-grown or improperly stored grains
- The fungal infestation tends to thrive in pastures with inadequate drainage systems and excessive shade coverage
Ergotism becomes more widespread when climatic changes lead to increased fungal growth. Unusual wet weather followed by heat enables Claviceps purpurea to reach its peak development potential.
Complications of Untreated Ergotism
Long-term Neurological Damage:
The main risk of wrong ergotism diagnosis includes permanent nervous system damage. Ergot alkaloids cause neurotoxicity by disrupting serotonin and dopamine pathways in the body.11Flieger, M., Wurst, M., & Shelby, R. (1997). Ergot alkaloids—sources, structures and analytical methods. Folia Microbiologica, 42(1), 3–30. https://doi.org/10.1007/BF02817427
Potential neurological outcomes include:
- Memory loss and cognitive decline
- Chronic seizures or epilepsy
- Motor dysfunction, such as tremors or paralysis
- Persistent hallucinations or psychosis
The brain tissues continue to experience damage from residual toxins, together with inflammation and oxidative stress, which persist even after exposure has stopped. The long-term effects of this damage primarily affect children and older adults.
Tissue Necrosis & Amputations:
As ergot alkaloids restrict blood flow, tissues starve of oxygen and begin to die. Signs of necrosis include:
- Cold, numb extremities
- Skin that turns dark or purple
- Ulcers or blisters that do not heal
- Foul-smelling tissue or visible black gangrene
Most affected areas are fingers, toes, and the tip of the nose. In animals, ears, tails, and hooves can suffer the same fate. The treatment for severe cases requires surgical removal of dead tissue or total limb removal to stop systemic infection.12Riet-Correa, F., & Medeiros, R. M. T. (2001). Ergotism in livestock and humans. Toxicon, 39(7), 1025–1032.
Public Health and Ergotism
Though rare today, ergotism still holds potential for public health crises, especially in regions with poor food regulation. Health departments and agricultural ministries should detect contaminated grain supplies or medication overdoses early.
Public health measures include:
- Routine testing of cereal grain shipments for ergot contamination
- Creating emergency response protocols for outbreaks in rural communities
- Collaborating with veterinary departments when livestock are affected.13Strickland, J. R., Looper, M. L., Matthews, J. C., Rosenkrans, C. F., Flythe, M. D., & Brown, K. R. (2011). Board-invited review: St. Anthony’s Fire in livestock: Causes, diagnosis, and mitigation. Journal of Animal Science, 89(5), 1603–1626. https://doi.org/10.2527/jas.2010-3462
When there is a suspected contamination, immediate coordination between local clinics and food safety organizations, and public health agencies is required. Fast identification of the source allows prevention of further exposure and facilitates contaminated product recalls.
Advances in Research & Medicine
As with many other diseases, technology is transforming how ergotism is detected and managed. New diagnostic tools help medical professionals identify this condition before permanent damage can occur.
Recent innovations include:
- Portable toxin detection kits: For use in the field or small clinics
- Genetic tests: Identifying susceptibility to alkaloid toxicity
- Advanced imaging, Such as MRI angiography, to assess vascular damage
- Real-time monitoring apps: For tracking symptoms in patients using ergot medications
These diagnostic tools reduce the gap between urban hospitals and rural clinics, while serving patients who require prompt identification of their condition.
The speed and precision of ergot testing for feed samples have improved in veterinary laboratories, which enables quick responses to suspected animal outbreaks.
Conclusion
Modern society views ergotism as a historical phenomenon, yet this silent threat continues to endanger people in the present day. The dangers of ergotism exist through food contamination and pharmaceutical misuse, which require public attention. The condition affects people, along with communities and pet animals, and even cultural memory.
Healthcare providers need to stay alert to its warning signs. Farmers, together with veterinarians, need to identify the dangers that exist in their agricultural lands and feed. People need to stay informed about ergot to prevent accidental contact.
Research combined with global awareness and proactive healthcare strategies enables ergotism to stay both rare and manageable. The presence of ergot creates danger because it thrives under constant surveillance.14Tudzynski, P., & Scheffer, J. (2004). Claviceps purpurea: Molecular aspects of a unique pathogenic lifestyle. Molecular Plant Pathology, 5(5), 377–388. https://doi.org/10.1111/j.1364-3703.2004.00237.x
Refrences
- 1Puschner, B. (2020). Ergot alkaloids – toxicology and clinical significance. Journal of Veterinary Diagnostic Investigation, 32(2), 183–191.
https://doi.org/10.1177/1040638719895455 - 2Bove, F. J. (1970). The Story of Ergot. Karger Publishers.
- 3Matossian, M. K. (1989). Poisons of the Past: Molds, Epidemics, and History. Yale University Press.
- 4Van Dongen, P. W. J., & de Groot, A. N. (1995). History of ergot alkaloids from ergotism to ergometrine. European Journal of Obstetrics & Gynecology and Reproductive Biology, 60(2), 109–116.
https://doi.org/10.1016/0028-2243(95)02247-7 - 5Smith, A. G., & Sullivan, J. B. (2003). Ergot alkaloids: Toxicologic overview and historical perspectives. Clinical Toxicology, 41(6), 807–811.
https://doi.org/10.1081/CLT-120024153 - 6Richard, J. L., & Bennett, G. A. (1999). Analysis of ergot alkaloids in livestock feed and human foods. Journal of AOAC International, 82(5), 1006–1012.
- 7Panaccione, D. G. (2005). Ergot alkaloids: Genetics and evolution. Natural Product Reports, 22(5), 622–631.
https://doi.org/10.1039/B501995C - 8Southwell, I. A., & Lowe, R. (1999). Natural Products in Australian Agriculture. CSIRO Publishing.
- 9Schardein, J. L. (1993). Chemically Induced Birth Defects. CRC Press. [Details on the vasoconstrictive effects of ergot]
- 10Coulombe, R. A. (2003). Ergot alkaloids in agriculture and food: Toxicology and safety concerns. Toxicon, 42(4), 355–369.
https://doi.org/10.1016/S0041-0101(03)00244-4 - 11Flieger, M., Wurst, M., & Shelby, R. (1997). Ergot alkaloids—sources, structures and analytical methods. Folia Microbiologica, 42(1), 3–30. https://doi.org/10.1007/BF02817427
- 12Riet-Correa, F., & Medeiros, R. M. T. (2001). Ergotism in livestock and humans. Toxicon, 39(7), 1025–1032.
- 13Strickland, J. R., Looper, M. L., Matthews, J. C., Rosenkrans, C. F., Flythe, M. D., & Brown, K. R. (2011). Board-invited review: St. Anthony’s Fire in livestock: Causes, diagnosis, and mitigation. Journal of Animal Science, 89(5), 1603–1626. https://doi.org/10.2527/jas.2010-3462
- 14Tudzynski, P., & Scheffer, J. (2004). Claviceps purpurea: Molecular aspects of a unique pathogenic lifestyle. Molecular Plant Pathology, 5(5), 377–388. https://doi.org/10.1111/j.1364-3703.2004.00237.x

