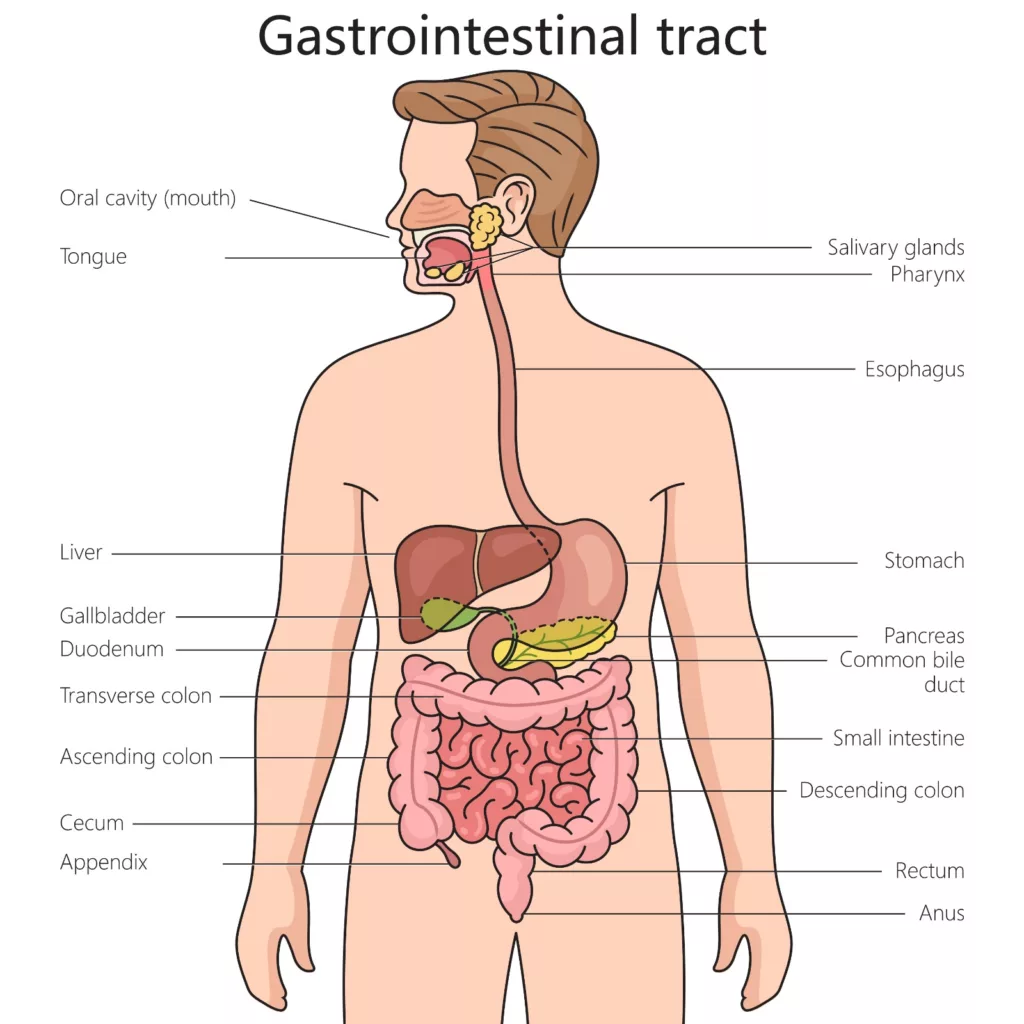
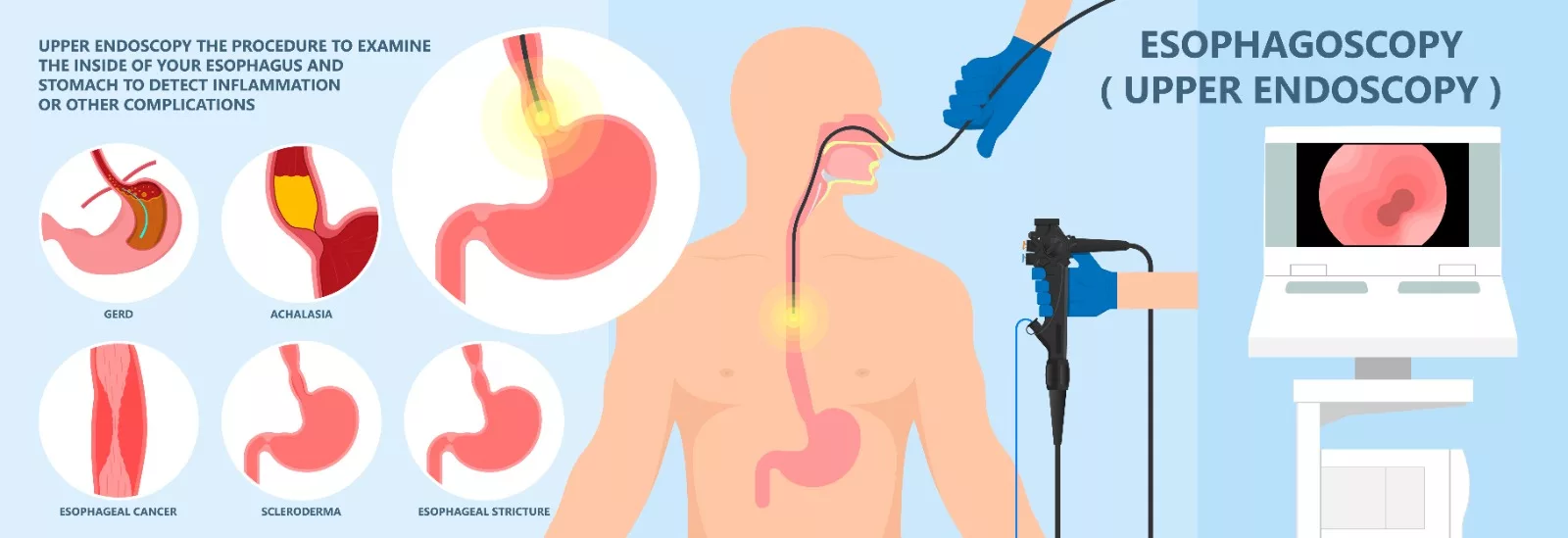
EGD (Esophagogastroduodenoscopy), also called upper GIT (Gastrointestinal tract) endoscopy, is a procedure used to visualize the proximal parts of the gastrointestinal tract, such as the oropharynx, esophagus, stomach, and proximal duodenum. The esophagus is a hollow muscular tube that is located behind the trachea. It begins after the cricoid cartilage and continues till the cardiac orifice of the stomach. The stomach is located below the diaphragm and begins at the cardiac portion. Then comes the fundus, body, pylorus, and finally, the stomach ends at the pyloric antrum, from which the duodenum continues. The duodenum is the first portion of the small intestine, which connects to the jejunum at the level of the ligament of Treitz.
EGD is one of the most common diagnostic endoscopic procedures used by gastroenterologists.1Ahlawat R, Hoilat GJ, Ross AB. Esophagogastroduodenoscopy. [Updated 2023 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK532268/ It consists of a small flexible endoscope, a light source, and a camera that uses video chips or fiber optics for image transmission.2Medscape. (n.d.). Esophagogastroduodenoscopy (EGD) Technique: Upper Gastrointestinal Endoscopy, Complications. Retrieved from https://www.medscape.com/viewarticle/759334
Purpose of EGD
EGD is used to diagnose and treat esophageal, gastric, and small intestine disorders. During the procedure, the doctor or endoscopist can obtain diagnostic biopsies or perform therapies to achieve homeostasis and dilate strictures. EGD is generally safe and well-tolerated if a skilled technician performs it. Its availability and use in the pediatric population have also increased recently. Still, a critical review of this tool’s use is required to get the maximum desired results and minimize the risks.
What are the indications of an EGD?
You should consider getting an EGD if your doctor advises you because of the following indications:
Diagnostic:
- Continuous abdominal pain or pain associated with alarming symptoms such as anorexia or weight loss
- Chronic or severe symptoms of Gastrointestinal Reflux Disease (GERD) such as heartburn, chronic cough, etc.
- Difficulty in swallowing, pain during swallowing, or feeding problems
- Persistent vomiting of unknown cause or hematemesis
- Irritable child with unexplained cause
- Chronic diarrhea or malabsorption symptoms such as weight loss, difficulty to-flush stool, lethargy
- Iron deficiency anemia with presumed chronic blood loss, when colonoscopy is normal or an upper GI source, is suspected clinically
- Inspect for malignancy in patients with premalignant conditions of the upper gastrointestinal tract, such as previous caustic ingestion, Barrett esophagus, or polyposis syndromes
- To assess for acute injury after caustic ingestion
Therapeutic:
- Removal of foreign body
- Stenting and dilatation of strictures
- Ligation of esophageal varices
- Controlling Upper GI bleed
- Placing of feeding or draining tubes
- Management of achalasia (balloon dilation or botulinum toxin)3Ahlawat R, Hoilat GJ, Ross AB. Esophagogastroduodenoscopy. [Updated 2023 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK532268/
Contraindications of an EGD
Your doctor will advise you against EGD if its risks outweigh its benefits. Some of the absolute and relative contraindications are:
Absolute:
- Suspected or known GIT perforation or peritonitis
- Wound dehiscence
- Severe sepsis, hypotension, or shock
- Respiratory distress, hypoxemia, stridor
Relative:
- Zenker’s diverticulum, an obstructing pharyngeal or laryngeal lesion, severe hypopharyngeal trauma
- Severe coagulopathy (INR > 3.0, platelet count <30,000/cumm)4Cappell MS, Friedel D. The role of esophagogastroduodenoscopy in the diagnosis and management of upper gastrointestinal disorders. Med Clin North Am. 2002 Nov;86(6):1165-216. doi: 10.1016/s0025-7125(02)00075-5. PMID: 12510452.
What are the preparations made for an EGD?
The doctor will perform an EGD in an outpatient setting using parenteral or general anesthesia. He may also do it at the bedside in a hospital or an operative room.5Ahlawat R, Hoilat GJ, Ross AB. Esophagogastroduodenoscopy. [Updated 2023 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK532268/
Patient Education & Consent
The doctor will inform you about the procedure’s indications, nature, risks, benefits, alternatives, and complications and will give you a consent form to ask for your consent.
Pre-Procedure Planning
After you’ve consented, the doctor will ask for your complete medical history and perform a physical exam to determine that you are fit for the procedure. He’ll document the significant findings in your medical record and give special attention to certain illnesses that might hinder the endoscopy, such as pulmonary and cardiovascular diseases. He’ll also ask you for a history of drug allergies and previous abdominal surgeries.
Afterward, you will undergo baseline tests such as Complete Blood Count (CBC), blood cross-matching, coagulation studies, urinalysis, electrolytes, pregnancy testing, Electrocardiography (ECG), and chest X-ray. These tests are based on the patient’s symptoms, and the doctor may suggest skipping them altogether if the patient is healthy and opting for an elective outpatient endoscopy. You’ll also be recommended antibiotic prophylaxis if you have an underlying high-risk health condition for infectious complications or are undergoing a high-risk endoscopic procedure. Specific recommendations for antibiotic prophylaxis based on the type of endoscopic procedure are available from the American Society for Gastrointestinal Endoscopy (ASGE).
Equipment
The medical staff or doctor will inform you about the type of endoscope they will use for your procedure. Several different types of endoscopes are available from various manufacturers. They may use a conventional endoscope or opt for a flexible ultrathin fiberoptic and video endoscope without sedation.

There are some newer endoscopes that have been introduced that provide higher resolution and magnifying endoscopy to evaluate certain GIT diseases. An advanced video endoscopy called narrow-band imaging (NBI) has recently been introduced, which uses optical filters and high relative intensity of blue light for imaging and characterization of mucosal morphology. An ultrasonic endoscopic has been developed to allow the simultaneous performance of EGD and EUS (Endoscopic ultrasound).6Medscape. (n.d.). Esophagogastroduodenoscopy (EGD) Technique: Upper Gastrointestinal Endoscopy, Complications. Retrieved from https://www.medscape.com/viewarticle/759334
Diet
The night before your EGD procedure, eat your largest meal before 6 pm. You can have a light snack till midnight but do not eat any solid food after midnight. You can have clear liquids until 4 hours before you arrive at your hospital.7Cappell MS, Friedel D. The role of esophagogastroduodenoscopy in the diagnosis and management of upper gastrointestinal disorders. Med Clin North Am. 2002 Nov;86(6):1165-216. doi: 10.1016/s0025-7125(02)00075-5. PMID: 12510452.
Medications
Consult your doctor about medications you can stop taking and which medicines you should continue. A week before the procedure, you’ll be advised to stop taking iron, aspirin, aspirin products, or Pepto Bismol. Five days before the procedure, you must stop taking non-steroidal anti-inflammatories (NSAIDs) such as Advil (ibuprofen), Celebrex, Motrin, etc. You’ll not be allowed to eat or drink (NPO) at least 8 hours before the procedure. Only medications can be taken 4 hours before examination with little sips of water.8Atlantic General Hospital. (n.d.). Upper Endoscopy Preparation. Retrieved from https://www.atlanticgeneral.org/documents/content/Upper-Endoscopy-preparation.pdf
Patient Preparation
Anesthesia/Sedation & Monitoring
The anesthesiologist will give you a numbing medicine (anesthesia) to prevent discomfort and to provide amnesia for the procedure. The anesthesiologist will evaluate your medical and drug history to see if it’s safe for you to undergo anesthesia.9Ahlawat R, Hoilat GJ, Ross AB. Esophagogastroduodenoscopy. [Updated 2023 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK532268/ Anesthesia is of two types: topical and general. Topical anesthesia, such as Cetacaine or Lidocaine, requires less time for the overall procedure, eliminates the risk of sedation, and decreases the cost of the procedure by reducing recovery time and nursing staff. It also has disadvantages like obstacles in performing the procedure on a patient who may not be still and discomfort.10Medscape. (n.d.). Esophagogastroduodenoscopy (EGD) Technique: Upper Gastrointestinal Endoscopy, Complications. Retrieved from https://www.medscape.com/viewarticle/759334
If you’re going through routine upper endoscopy, you’ll be sedated by giving IV propofol. For therapeutic endoscopic procedures and in young and uncooperative patients, general anesthesia will be given. Your vital signs and cardiopulmonary status will be continuously monitored throughout the endoscopic procedure.11ASGE Standards of Practice Committee. Early DS, Lightdale JR, Vargo JJ, Acosta RD, Chandrasekhara V, Chathadi KV, Evans JA, Fisher DA, Fonkalsrud L, Hwang JH, Khashab MA, Muthusamy VR, Pasha SF, Saltzman JR, Shergill AK, Cash BD, DeWitt JM. Guidelines for sedation and anesthesia in GI endoscopy. Gastrointest Endosc. 2018 Feb;87(2):327-337. ECG is also monitored in patients with cardiopulmonary disease, elderly patients, or during a prolonged procedure. Anesthetic agents used in EGD include Benzodiazepines, opioids, and reversal agents.
Positioning
You’ll be placed in a left lateral position.
What is the Procedure for an EGD?
The doctor administers topical and IV sedation to facilitate the procedure and minimize gagging. Additionally, they may administer an antispasmodic agent such as atropine, glucagon, or cimetropium bromide to suppress gastrointestinal peristalsis. A bite block is then placed to prevent damage to the endoscope and facilitate its passage through the mouth.
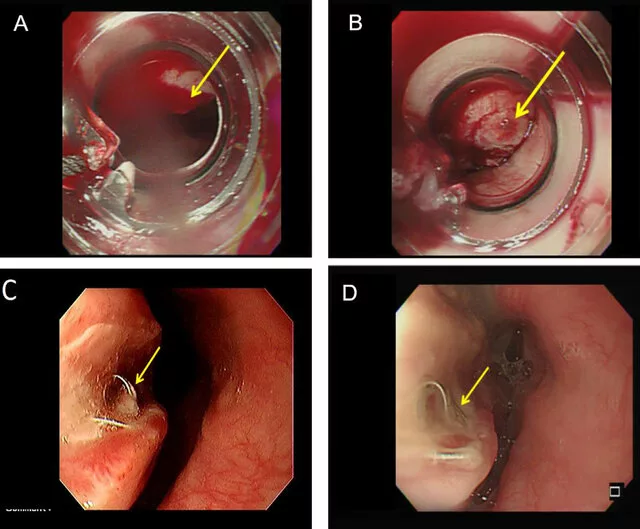
The doctor passes the endoscope through the pharynx, esophagus, stomach, and into the duodenum under direct vision, carefully inspecting both insertion and slow withdrawal. They insufflate air to distend the lumen for a better view and aspirate liquid and particulate matter through the suction channel. The findings are documented with pictures or a video system. The doctor may also obtain biopsy specimens by passing forceps and taking small mucosal samples for inspection on histology sites. During the endoscopy, the surgeon can perform various therapeutic procedures. The duration of the procedure may range from 5 to 30 minutes or longer, depending on the therapeutic or diagnostic maneuvers used.12Medscape. (n.d.). Esophagogastroduodenoscopy (EGD) Technique: Upper Gastrointestinal Endoscopy, Complications. Retrieved from https://www.medscape.com/viewarticle/759334
What are the Potential Complications of an EGD?
EGD is a safe procedure; its complications are relatively uncommon, with only one complication per 1000 procedures.13Cappell MS, Friedel D. The role of esophagogastroduodenoscopy in the diagnosis and management of upper gastrointestinal disorders. Med Clin North Am. 2002 Nov;86(6):1165-216. doi: 10.1016/s0025-7125(02)00075-5. PMID: 12510452. They most likely result from a prolonged or therapeutic EGD for procedures such as sclerotherapy, electrocautery, or dilations. Some of them are:
- Pulmonary complications such as aspiration pneumonia, asthmatic attack, or respiratory depression
- Cardiac complications such as hypotension, pulmonary edema, or myocardial infarction
- Medication hypersensitivity such as rash, bronchospasm, or anaphylaxis
- Perforation
- Bleeding
- Neurologic complications such as seizures and stroke
- Laryngeal Injury
- Infectious complications such as cellulitis, endocarditis, or septic phlebitis14Cappell MS, Friedel D. The role of esophagogastroduodenoscopy in the diagnosis and management of upper gastrointestinal disorders. Med Clin North Am. 2002 Nov;86(6):1165-216. doi: 10.1016/s0025-7125(02)00075-5. PMID: 12510452.
What is the post-op care of a patient who has just gone EGD?
After the procedure, you’ll be transferred to a recovery room, where an endoscopy nurse will monitor you. The nurse will observe your vitals and notify your attendant when you’re awake. Once alert and mobile, you can leave the recovery room with an attendant. You’ll be given some instructions regarding your diet and activity and advised to return immediately to the doctor in case of any alarming symptoms, such as:
- Fever
- Stomach cramps
- Signs and symptoms of GI Bleeding
The medical staff will arrange a follow-up appointment with your primary care physician or endoscopist, and then they will discharge you.15Medscape. (n.d.). Esophagogastroduodenoscopy (EGD) Technique: Upper Gastrointestinal Endoscopy, Complications. Retrieved from https://www.medscape.com/viewarticle/759334 In some cases, such as treating bleeding from esophageal varices, the medical team will schedule a follow-up plan, including a short-interval repeat endoscopy procedure for the patient, and prescribe medications until the varices are removed.
Patients diagnosed with gastric ulcers must take Proton Pump Inhibitors (PPIs) or H2 antagonists and undergo testing for H. pylori infection. Patients who have undergone dilation of peptic or esophageal strictures will also receive PPI therapy.16Cohen J, Safdi MA, Deal SE, Baron TH, Chak A, Hoffman B, Jacobson BC, Mergener K, Petersen BT, Petrini JL, Rex DK, Faigel DO, Pike IM; ASGE/ACG Taskforce on Quality in Endoscopy. Quality indicators for esophagogastroduodenoscopy. Am J Gastroenterol. 2006 Apr;101(4):886-91. doi: 10.1111/j.1572-0241.2006.00676.x. PMID: 16635232.
How long does it take to recover after an EGD?
The average recovery time after an upper endoscopic procedure is around 50 minutes, and you’ll be discharged on the same day after being observed for 6 hours (if anesthesia is given). Recovery time may differ depending on the patient’s condition, symptoms, and any complications. Patients who did not receive sedation tend to recover more quickly than those who did. Some patients may need extended hospital stays, such as patients who had:
- Bleeding (Variceal or Non-Variceal)
- Luminal Dilation and stenting
- Foreign body removal
- Percutaneous Endoscopic Gastrotomy (PEG)
- Endoscopic Mucosal Resection (EMR) and Endoscopic Submucosal Dissection
- Per Oral Endoscopic Myotomy (POEM)17Walke SS, Chauhan S, Pandey V, Jadhav R, Chaudhari V, Vishwanathan D, Kolhe K, Ingle M. When to Discharge a Patient After Endoscopy: A Narrative Review. Clin Endosc. 2022 Jan;55(1):8-14. doi: 10.5946/ce.2021.110. Epub 2022 Jan 27. PMID: 35135177; PMCID: PMC8831418.
After an EGD, you may feel nausea, bloating, or a sore throat. You might also feel groggy for about 30 minutes after the procedure, and the feeling will fade within that hour. It’ll take some time for the effects of anesthesia to wear off, so you should avoid making any big decisions that day, and an attendant should take you home.18“Preparing for Surgery: Upper Endoscopy.” American Society of Anesthesiologists, www.asahq.org/madeforthismoment/preparing-for-surgery/procedures/upper-endoscopy/.
Difference between an EGD & Endoscopy
Endoscopy is a procedure done to examine structures inside your body. It is done with an endoscope, which is an inspection instrument composed of an image sensor, an optical lens, a light source, and a mechanical device. There are many different types of endoscopy, and they’re named according to the part of the body that they inspect, such as bronchoscopy (to visualize the airways), hysteroscopy (to visualize the cervix and uterus), colonoscopy (to visualize the large intestine), sigmoidoscopy (to visualize the rectum and sigmoid colon), cystoscopy (to visualize the urinary bladder and urethra), etc. EGD is an endoscope that visualizes the upper GIT (oropharynx, esophagus, stomach, and proximal duodenum).
Difference between an EGD & Colonoscopy
The main difference between the two procedures lies in the areas they examine, with EGD focusing on the upper GIT, while colonoscopy focuses on the rectum and large intestine (colon). Colonoscopy’s main purpose is to screen and diagnose colon cancer in individuals aged 50 or older, while EGD is used for both diagnostic and therapeutic procedures of upper GIT symptoms.
The procedure lasts from 30 minutes to an hour in a colonoscopy. A patient is extensively prepared for a colonoscopy, with a special diet and restrictions on food intake. A day before the procedure, the patients must consume a low-fiber diet and only clear liquids. Doctors may also prescribe a stool softener or cleansing solution to clean the bowel thoroughly. The complications of both procedures are similar, such as bleeding, perforation, and infection, with a slightly higher risk of perforation during colonoscopy compared to EGD. The doctor may recommend further diagnostic tests or treatment depending on the endoscopy findings.19Understanding the Differences: Endoscopy vs. Colonoscopy.” Northlake Gastroenterology, www.northlakegastro.com/understanding-the-differences-endoscopy-vs-colonoscopy
Conclusion
To summarize, consider visiting a doctor and asking for an EGD if you’ve recurrent symptoms of upper GIT, such as abdominal pain, reflux symptoms, persistent vomiting, chronic diarrhea, or iron deficiency anemia. The EGD will visualize the proximal parts of the GIT and diagnose and treat the present disorders. It is a safe procedure with minimal risks and minimal recovery time. The medical team must rule out contraindications to this procedure and provide appropriate pre-op and post-op care to ensure a successful procedure. The biopsy results will further guide the management plan and ultimately result in the patient receiving complete treatment for the disease.
Refrences
- 1Ahlawat R, Hoilat GJ, Ross AB. Esophagogastroduodenoscopy. [Updated 2023 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK532268/
- 2Medscape. (n.d.). Esophagogastroduodenoscopy (EGD) Technique: Upper Gastrointestinal Endoscopy, Complications. Retrieved from https://www.medscape.com/viewarticle/759334
- 3Ahlawat R, Hoilat GJ, Ross AB. Esophagogastroduodenoscopy. [Updated 2023 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK532268/
- 4Cappell MS, Friedel D. The role of esophagogastroduodenoscopy in the diagnosis and management of upper gastrointestinal disorders. Med Clin North Am. 2002 Nov;86(6):1165-216. doi: 10.1016/s0025-7125(02)00075-5. PMID: 12510452.
- 5Ahlawat R, Hoilat GJ, Ross AB. Esophagogastroduodenoscopy. [Updated 2023 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK532268/
- 6Medscape. (n.d.). Esophagogastroduodenoscopy (EGD) Technique: Upper Gastrointestinal Endoscopy, Complications. Retrieved from https://www.medscape.com/viewarticle/759334
- 7Cappell MS, Friedel D. The role of esophagogastroduodenoscopy in the diagnosis and management of upper gastrointestinal disorders. Med Clin North Am. 2002 Nov;86(6):1165-216. doi: 10.1016/s0025-7125(02)00075-5. PMID: 12510452.
- 8Atlantic General Hospital. (n.d.). Upper Endoscopy Preparation. Retrieved from https://www.atlanticgeneral.org/documents/content/Upper-Endoscopy-preparation.pdf
- 9Ahlawat R, Hoilat GJ, Ross AB. Esophagogastroduodenoscopy. [Updated 2023 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK532268/
- 10Medscape. (n.d.). Esophagogastroduodenoscopy (EGD) Technique: Upper Gastrointestinal Endoscopy, Complications. Retrieved from https://www.medscape.com/viewarticle/759334
- 11ASGE Standards of Practice Committee. Early DS, Lightdale JR, Vargo JJ, Acosta RD, Chandrasekhara V, Chathadi KV, Evans JA, Fisher DA, Fonkalsrud L, Hwang JH, Khashab MA, Muthusamy VR, Pasha SF, Saltzman JR, Shergill AK, Cash BD, DeWitt JM. Guidelines for sedation and anesthesia in GI endoscopy. Gastrointest Endosc. 2018 Feb;87(2):327-337.
- 12Medscape. (n.d.). Esophagogastroduodenoscopy (EGD) Technique: Upper Gastrointestinal Endoscopy, Complications. Retrieved from https://www.medscape.com/viewarticle/759334
- 13Cappell MS, Friedel D. The role of esophagogastroduodenoscopy in the diagnosis and management of upper gastrointestinal disorders. Med Clin North Am. 2002 Nov;86(6):1165-216. doi: 10.1016/s0025-7125(02)00075-5. PMID: 12510452.
- 14Cappell MS, Friedel D. The role of esophagogastroduodenoscopy in the diagnosis and management of upper gastrointestinal disorders. Med Clin North Am. 2002 Nov;86(6):1165-216. doi: 10.1016/s0025-7125(02)00075-5. PMID: 12510452.
- 15Medscape. (n.d.). Esophagogastroduodenoscopy (EGD) Technique: Upper Gastrointestinal Endoscopy, Complications. Retrieved from https://www.medscape.com/viewarticle/759334
- 16Cohen J, Safdi MA, Deal SE, Baron TH, Chak A, Hoffman B, Jacobson BC, Mergener K, Petersen BT, Petrini JL, Rex DK, Faigel DO, Pike IM; ASGE/ACG Taskforce on Quality in Endoscopy. Quality indicators for esophagogastroduodenoscopy. Am J Gastroenterol. 2006 Apr;101(4):886-91. doi: 10.1111/j.1572-0241.2006.00676.x. PMID: 16635232.
- 17Walke SS, Chauhan S, Pandey V, Jadhav R, Chaudhari V, Vishwanathan D, Kolhe K, Ingle M. When to Discharge a Patient After Endoscopy: A Narrative Review. Clin Endosc. 2022 Jan;55(1):8-14. doi: 10.5946/ce.2021.110. Epub 2022 Jan 27. PMID: 35135177; PMCID: PMC8831418.
- 18“Preparing for Surgery: Upper Endoscopy.” American Society of Anesthesiologists, www.asahq.org/madeforthismoment/preparing-for-surgery/procedures/upper-endoscopy/.
- 19Understanding the Differences: Endoscopy vs. Colonoscopy.” Northlake Gastroenterology, www.northlakegastro.com/understanding-the-differences-endoscopy-vs-colonoscopy

