What is Patellofemoral Pain Syndrome?
Patellofemoral Pain Syndrome (PFPS), often called runner’s knee, is one of the most common causes of knee pain, especially among athletes. This condition accounts for up to 25% of knee injuries treated in sports medicine clinics.1Dutton, R. A., Khadavi, M. J., & Fredericson, M. (2016). Patellofemoral Pain. Physical medicine and rehabilitation clinics of North America, 27(1), 31–52. https://doi.org/10.1016/j.pmr.2015.08.002
The pain usually occurs at the front, behind, or around the kneecap (patella), and it’s common in runners and those who engage in sports involving a lot of running and jumping. While most people find relief with conservative treatments, the discomfort can persist for years in some cases.2Bump JM, Lewis L. Patellofemoral Syndrome. [Updated 2023 Feb 13]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK557657/
If left untreated, patellofemoral pain can limit your activities and potentially lead to chronic joint problems. So, addressing symptoms early is crucial for maintaining an active lifestyle.
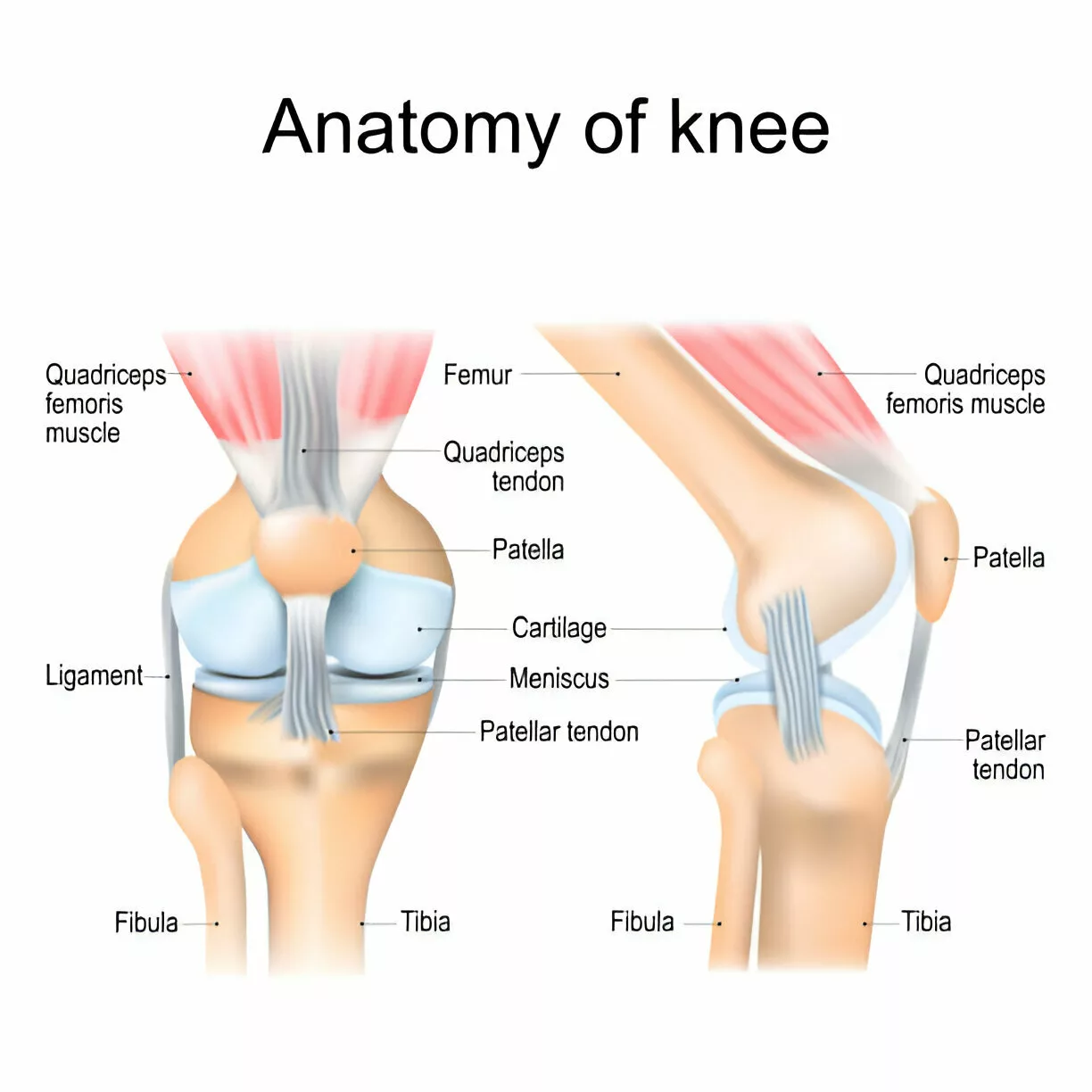
Overview of the Knee Joint
The knee joint is one of the most complex joints in the body, crucial for supporting body weight and allowing a wide range of activities such as walking, running, and jumping. It consists of several bones and tissues that provide stability, flexibility, and movement. Here is an overview of the knee joint’s structure:
Bones
- Femur: The thigh bone, forming the upper part of the knee joint.
- Tibia: The shin bone, forming the lower part of the knee joint.
- Patella: The kneecap, a small, triangular bone that protects and supports joint movement.
Cartilage
- Articular Cartilage: Cushions the ends of the femur, tibia, and patella, ensuring smooth movement of the knee joint.
Ligaments
- Ligaments: Provide stability by connecting bones within the joint.
Tendons
- Tendons: Connect muscles to bones, enabling movement.
Causes of the PFPS
Multiple factors cause patellofemoral pain syndrome. They may include;
Overuse/Repetitive Movement:
It is the most common cause of pain. Repetitive movements like running and jumping increase the workload on the kneecap, causing irritation under it.
Muscular Imbalance:
If the muscles around your hip and knee, especially the quadriceps, are weak or tight, they may cause PFPS. If the quadriceps are weak, they are unable to support your knee during the movement. Similarly, if they are tight, they may put increased tension on your knee.
Enhanced Training Level:
If you suddenly start any new activity or increase the intensity of your training, you may develop PFPS.
Malalignment of Patella:
If your knee has a structure different from normal biomechanics by birth, you may feel pain from PFPS.
Patellar Trauma:
Direct or indirect injury to the patella or kneecap can damage the patella and cause PFPS.
Symptoms of PFPS
The pain from patellofemoral pain syndrome is usually dull and achy, but sometimes, you may feel a sharp pain in or around your patella. You may also experience:3Willy, R. W., Hoglund, L. T., Barton, C. J., Bolgla, L. A., Scalzitti, D. A., Logerstedt, D. S., Lynch, A. D., Snyder-Mackler, L., & McDonough, C. M. (2019). Patellofemoral Pain. The Journal of orthopedic and sports physical therapy, 49(9), CPG1–CPG95. https://doi.org/10.2519/jospt.2019.0302
- Worsening pain while squatting, stair climbing, running, or prolonged sitting
- You may feel like your kneecap is moving while walking
- Pain can limit your ability to work, play sports, or engage in physical activities
Risk factors of PFPS
The risk factors for developing patellofemoral pain syndrome include;
- PFPS typically affects adolescents and adult people younger than 60 years
- Women are more prone to developing this condition
- Sports like running and jumping increase the tendency to develop PFSP
- Weakness of the quadriceps muscle greatly contributes to developing this pain
- An unstable patella increases the chance of getting PFS
- Foot abnormalities are also a risk factor for pain
Diagnosis of Patellofemoral Pain Syndrome
The diagnosis of patellofemoral pain syndrome is usually clinical.4Duong, V., Oo, W. M., Ding, C., Culvenor, A. G., & Hunter, D. J. (2023). Evaluation and Treatment of Knee Pain: A Review. JAMA, 330(16), 1568–1580. https://doi.org/10.1001/jama.2023.19675 Your doctor may:
- Ask about your symptoms.
- A detailed physical examination may be performed to evaluate joint inflammation, movement ranges, redness, weakness, and tenderness, comparing the affected side with the unaffected side. Examining gait, posture, and footwear as well.5Gaitonde, D. Y., Ericksen, A., & Robbins, R. C. (2019). Patellofemoral Pain Syndrome. American Family Physician, 99(2), 88–94.
- Plain radiographs are not helpful. However, if your pain shows no response, radiography is used to rule out other conditions, such as osteoarthritis, osteochondritis, and patellar fracture.
Treatment for Patellofemoral Pain Syndrome
Treatment for patellofemoral pain syndrome follows a conservative approach and is typically divided into two phases: the acute phase, focused on pain reduction, and the recovery phase, aimed at correcting the issue through a rehabilitation plan.
Acute Phase:
The primary goal during this phase is to alleviate pain and discomfort. This is achieved through:
Activity Modification
If you engage in sports or activities that stress the knee joint, such as running or squatting, it is important to avoid these activities to relieve pressure on the knee temporarily.
Medication
Your doctor may prescribe medication (analgesics) to manage pain and reduce its intensity.
Cold Therapy
Applying cold packs or using ice therapy is helpful as it can reduce swelling and alleviate pain.
Recovery Phase:
The recovery phase involves a personalized physical therapy plan to help you regain strength and flexibility for daily activities. It is the mainstay of treatment if you have patellofemoral pain syndrome. Under the guidance of a physical therapist, the plan includes 6Dixit, S., DiFiori, J. P., Burton, M., & Mines, B. (2007). Management of patellofemoral pain syndrome. American Family Physician, 75(2), 194–202.
Exercise Therapy
They focus on strengthening your muscles around the hip and knee, especially the quadriceps. Exercise therapy for patellofemoral pain syndrome (PFPS) can significantly reduce pain, improve functional ability, and promote long-term recovery.7van der Heijden, R. A., Lankhorst, N. E., van Linschoten, R., Bierma-Zeinstra, S. M., & van Middelkoop, M. (2015). Exercise for treating patellofemoral pain syndrome. The Cochrane database of systematic reviews, 1(1), CD010387. https://doi.org/10.1002/14651858.CD010387.pub2
Patellar Taping:
Patellar taping is helpful for correcting biomechanical issues that cause patellofemoral pain, such as the sideways movement of the patella. This technique reduces pain and pressure on the patella and supports the hip and knee muscles during movements like running.

However, taping alone is less effective than when combined with physical therapy or exercises.8Logan, C. A., Bhashyam, A. R., Tisosky, A. J., Haber, D. B., Jorgensen, A., Roy, A., & Provencher, M. T. (2017). Systematic Review of the Effect of Taping Techniques on Patellofemoral Pain Syndrome. Sports Health, 9(5), 456–461. https://doi.org/10.1177/1941738117710938
Bracing & Orthotics
Physical Therapists, after assessing your condition, may suggest braces or knee orthotics to correct biomechanics issues contributing to the pain.9Smith, T. O., Drew, B. T., Meek, T. H., & Clark, A. B. (2015). Knee orthoses for treating patellofemoral pain syndrome. The Cochrane database of systematic reviews, 2015(12), CD010513. https://doi.org/10.1002/14651858.CD010513.pub2
Prevention from Patellofemoral Pain Syndrome
Knee pain can arise from various factors. However, following these measures may help prevent patellofemoral pain syndrome:
- Muscle Strength: Strong leg muscles support the knee joint and help prevent pain during movement.
- Maintaining Body Weight: If you are overweight, try to lose some weight. Extra weight stresses large joints, including the knee joint, causing pain.
- Move Safely: Always move, jump, run, or do daily activities with caution to avoid injuries.
- Training Safely: Warm up and do gentle stretching exercises before training. This improves joint and muscle flexibility.
- Proper Footwear: To avoid pain and discomfort, ensure you wear shoes that fit well and are suitable for your feet and activities.
Physical Therapy & Exercises for Patellofemoral Pain Syndrome
Physical therapy is essential for reducing pain and improving muscle strength and flexibility. It helps alleviate short- and long-term pain, whether at rest or during activity. Strengthening the muscles around the hip and knee significantly improves knee pain and function.
Straight Leg Raise:
- Lie on your back with the unaffected leg slightly bent and the affected leg straight.
- Lift the affected leg toward the ceiling.
- Hold for 10 seconds, then lower the leg.
- Repeat ten times for three sets.
Quadriceps Strengthening:
- Sit with your back supported and legs straight.
- Place a pillow or towel roll under the affected knee.
- Press the towel down with your knee to strengthen the quadriceps.
- Repeat ten times for three sets.
Abductor Strengthening:
- Lie on your side with the affected side on top, and the knees bent.
- Lift the affected knee toward the ceiling while keeping the hip stable.
- Repeat ten times for three sets.
Surgery for Patellofemoral Pain Syndrome
Surgery for patellofemoral pain is rare. However, your doctor may recommend it if you experience severe knee pain and conservative treatments are ineffective.
Your doctor may perform an arthroscopy, a minimally invasive surgery. They make small incisions around the knee and insert a long tube with a camera to examine its internal structure. This allows them to identify and repair or remove damaged tissue. The procedure typically results in less pain and a faster recovery than traditional surgery.
Recovery time
Recovery from patellofemoral pain typically takes six weeks or more with conservative treatment. Enhancing muscle strength and flexibility around the hip and knee is crucial for a gradual return to activity. Your physical therapist will design a rehabilitation program based on your needs, muscle strength, and activity level, usually spanning three to four weeks.
Conclusion
Patellofemoral pain syndrome is a musculoskeletal condition causing pain at the front, behind, or around the kneecap. It develops gradually and can worsen without treatment. This condition typically causes pain when bending the knee during activities like stair climbing, running, or squatting. Diagnosis is based on clinical evaluation.
Conservative treatments, such as physical therapy, patella taping, and orthotics for biomechanical correction, are the primary approaches. Prevention is crucial and involves wearing well-fitted shoes and gradually increasing training intensity. Surgery is rarely needed or effective for this condition. Recovery from patellofemoral pain syndrome usually takes 3-4 weeks.
Refrences
- 1Dutton, R. A., Khadavi, M. J., & Fredericson, M. (2016). Patellofemoral Pain. Physical medicine and rehabilitation clinics of North America, 27(1), 31–52. https://doi.org/10.1016/j.pmr.2015.08.002
- 2Bump JM, Lewis L. Patellofemoral Syndrome. [Updated 2023 Feb 13]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK557657/
- 3Willy, R. W., Hoglund, L. T., Barton, C. J., Bolgla, L. A., Scalzitti, D. A., Logerstedt, D. S., Lynch, A. D., Snyder-Mackler, L., & McDonough, C. M. (2019). Patellofemoral Pain. The Journal of orthopedic and sports physical therapy, 49(9), CPG1–CPG95. https://doi.org/10.2519/jospt.2019.0302
- 4Duong, V., Oo, W. M., Ding, C., Culvenor, A. G., & Hunter, D. J. (2023). Evaluation and Treatment of Knee Pain: A Review. JAMA, 330(16), 1568–1580. https://doi.org/10.1001/jama.2023.19675
- 5Gaitonde, D. Y., Ericksen, A., & Robbins, R. C. (2019). Patellofemoral Pain Syndrome. American Family Physician, 99(2), 88–94.
- 6Dixit, S., DiFiori, J. P., Burton, M., & Mines, B. (2007). Management of patellofemoral pain syndrome. American Family Physician, 75(2), 194–202.
- 7van der Heijden, R. A., Lankhorst, N. E., van Linschoten, R., Bierma-Zeinstra, S. M., & van Middelkoop, M. (2015). Exercise for treating patellofemoral pain syndrome. The Cochrane database of systematic reviews, 1(1), CD010387. https://doi.org/10.1002/14651858.CD010387.pub2
- 8Logan, C. A., Bhashyam, A. R., Tisosky, A. J., Haber, D. B., Jorgensen, A., Roy, A., & Provencher, M. T. (2017). Systematic Review of the Effect of Taping Techniques on Patellofemoral Pain Syndrome. Sports Health, 9(5), 456–461. https://doi.org/10.1177/1941738117710938
- 9Smith, T. O., Drew, B. T., Meek, T. H., & Clark, A. B. (2015). Knee orthoses for treating patellofemoral pain syndrome. The Cochrane database of systematic reviews, 2015(12), CD010513. https://doi.org/10.1002/14651858.CD010513.pub2

