Omphalocele is an inborn disorder in which a defect in your child’s central abdominal wall causes protrusion of the abdominal contents or organs outside the belly covered by a thin membrane layer.
What is Omphalocele?
Omphalocele, also called exomphalos, is a congenital disorder characterized by a central umbilical defect with protrusion of the abdominal contents (intestines and liver) on the abdominal surface. These contents are covered with three layers of membrane (peritoneum, Wharton’s jelly, and amnion) in continuity with the umbilical cord.1Kirby, R. S. (2017). The prevalence of selected major birth defects in the United States. Seminars in Perinatology, 41(6), 338–344. https://doi.org/10.1053/j.semperi.2017.07.004
The frequency of omphalocele reported in the United States of America is about 1.5-2 % per live birth. This frequency increased up to 11% from 1999-2007. It most commonly affects females and the black race.2Zahouani, T. (2023, May 23). Omphalocele. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK519010/#:~:text=Thus%2C%20large%20omphaloceles%20need%20a,gastroesophageal%20reflux%2C%20and%20occasionally%20esophagitis.
Types of Omphalocele
There are two types of omphaloceles. These are:
Omphalocele Minor
Omphalocele minor is a small less than 5cm defect with no liver involvement. This defect is closed easily by surgery.
Omphalocele Major
Omphalocele major is a large defect that is greater than 5 cm and contains multiple organs. This syndrome is repaired in staged surgical procedures.
When do Omphaloceles Occur?
Usually, during embryogenesis, during the 6th to 10th week of pregnancy, when the intestine and other organs grow, they are pushed into the umbilical cord. However, during the 11th week of pregnancy, the intestine and other organs return into the abdomen. If the intestines do not return to the abdomen or remain in the amniotic cavity, it causes omphalocele.
Causes & Risk Factors of Omphalocele
The exact cause of this condition is still unknown. It may be genetically induced or acquired. Some risk factors contribute to this condition in infants. These factors are related to the mother. These are:
- Women who have a history of smoking (1-2 packs per day) are at greater risk of having a baby with omphalocele than others.
- Drinking alcohol
- Some medications increase the risk of having omphalocele. Women who have a history of using serotonin reuptake inhibitors (SSRI) are more likely to have a child with omphalocele.
- Obese women are also at higher risk of getting omphalocele.
It is also associated with other syndromes such as Beckwith-Wiedemann syndrome, trisomy 13, trisomy 21 (down syndrome), charge syndrome, Carpenter syndrome, and Meckle-gruber syndrome.
Symptoms of Omphalocele
The clinical presentation varies from infant to infant, depending upon the severity of the disease. This condition can be seen clearly on the abdomen, but its features depend on the size of the defect. In small-sized omphaloceles, the intestine is the only content of the omphalocele. Comparatively, the intestine, the liver, and the spleen are present in a large amount of omphalocele.
How to Diagnose Omphalocele?
Almost all omphaloceles are diagnosed prenatally on ultrasound by the end of 1st trimester of pregnancy and postnatally by history and clinical examination. Evaluating the patient is necessary to rule out other inborn disorders like Beckwith-Wiedemann Syndrome.
History:
During history, your doctor may ask some questions related to your disease. These are:
- Do you smoke or not? If yes, then how many packs per day?
- Do you drink alcohol during pregnancy?
- Do you have a positive history of omphalocele?
- Weight of the mother during pregnancy?
- Any history of drug intake during pregnancy? If yes, then which drug did you use?
- Family history of omphalocele
These questions are necessary to figure out the exact cause of omphalocele.
Clinical Examination:
During the examination, your doctor will thoroughly examine your child to look for any other abnormality or syndrome related to omphalocele.
Other Tests:
Omphelocel can also result from other congenital anomalies. Therefore, your doctor may advise genetic testing to rule out other congenital disorders. Other tests are:
Amniocentesis
It is an invasive procedure in which the sample is taken from the amniotic fluid that surrounds the fetus. This test is recommended for the 2nd trimester of pregnancy.
Cell-Free Fetal DNA Testing
In this screening test, healthcare providers collect a sample from the mother to examine fetal DNA. A positive result requires further diagnostic evaluation.
Fetal karyotyping
After the baby’s birth, healthcare providers take a blood sample from the child to detect chromosomal abnormalities.
Imaging Studies:
In suspicious cases, your doctor may advise imaging studies:
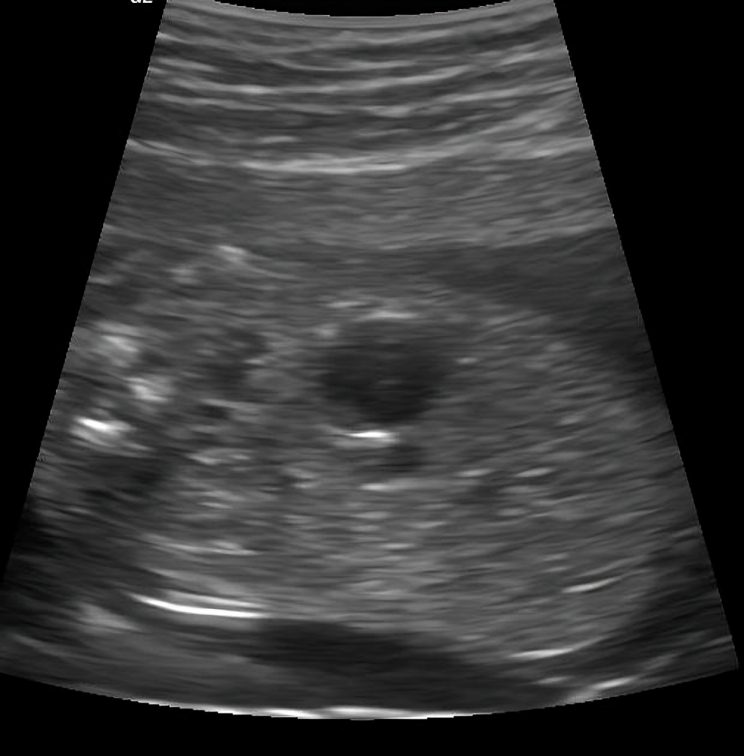
- Ultrasonography is the first line of investigation that helps your doctor to look into your abdomen. Prenatal ultrasound can detect all the possible structural anomalies. Therefore, this test is advised for diagnostic and screening purposes during pregnancy.
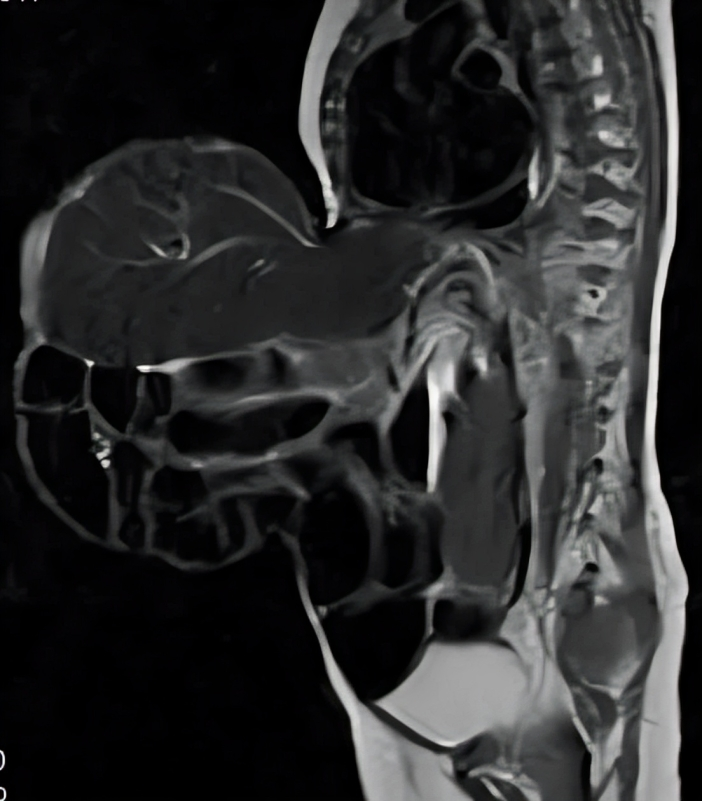
- MRI of the fetus helps to see the internal structure of the baby, which can not be seen on ultrasound
- Fetal echocardiogram: A simple, noninvasive test in which the heart rate is monitored to check the viability of the fetus.3Omphalocele. (n.d.). https://www.nationwidechildrens.org/conditions/omphalocele-fc
Care of the baby with Omphalocele
If your baby has this condition on prenatal ultrasound scan. Ensure your delivery at the tertiary care hospital for you and your child’s safety. When the baby is born with omphalocele, admit him to the nursery intensive care unit (NICU) for monitoring. In NICU a neonatologist will look after your child.
- If your child has breathing difficulty, the doctor will place a breathing tube/oxygen support to maintain his oxygen saturation.
- An IV line is inserted on your child’s hand, leg, or head to give fluid and antibiotic access and avoid dehydration.
- The omphalocele sac is covered with a sterile dressing to avoid infection.
- Your doctor will pass a nasogastric tube to decompress your child’s abdomen.
How to treat Omphalocele?
Your baby will stay in the NICU till the doctors plan surgery. Surgical repair is the only option to treat the omphalocele. Before surgery, your baby will stay in the NICU, and a surgeon will insert a special intravenous catheter called a peripherally inserted central catheter (PICC). This catheter gives nutrition to your child; this type of nutrition is total parenteral nutrition (TPN). Total parenteral nutrition contains all the nutrients that are essential for the growth of the child.4Ţarcă, E., Cojocaru, E., Trandafir, L. M., Luca, A. C., Tiutiucă, R. C., Butnariu, L. I., Costea, C. F., Radu, I., Moscalu, M., & Ţarcă, V. (2022). Current Challenges in the Treatment of the Omphalocele-Experience of a Tertiary Center from Romania. Journal of Clinical Medicine, 11(19), 5711. https://doi.org/10.3390/jcm11195711
Surgery:
Surgical repair is the first-line treatment for omphalocele. However, the surgery depends upon the type of omphalocele (large or small). The main goal of the surgery is to put back your child’s abdominal organs into the abdomen and close the central abdominal defect. 5Verla, M. A., Style, C. C., & Olutoye, O. O. (2019). Prenatal diagnosis and management of omphalocele. Seminars in pediatric surgery, 28(2), 84–88. https://doi.org/10.1053/j.sempedsurg.2019.04.007
Primary Surgical Repair
It is a simple procedure suitable for babies with a small omphalocele. The doctors advise this procedure after a few days of birth. In this procedure, the abdominal contents that are present inside the omphalocele are put back into your Child’s abdomen, and the muscular defect is repaired.
Staged Repair
Surgeons perform omphalocele surgery in stages for large defects. They remove the sac, place viscera in a silo, and gradually push them into the abdomen. When all the viscera are passed back into the abdomen (which may take a few days or weeks), the abdominal defect is closed via a patch.6Facs, J. G. G. M. M. (n.d.). Pediatric omphalocele and gastroschisis (Abdominal wall Defects) treatment & management: approach considerations, medical care, surgical care. https://emedicine.medscape.com/article/975583-treatment#d1
What happens after the Surgery?
After the surgery, your baby will move to the NICU to monitor your child. In the NICU, your doctor will give the following post-surgery care:
- Oxygen support to your baby to maintain saturation
- Antibiotics to avoid infection
- Painkillers to avoid pain
- Electrolytes to avoid dehydration
- The doctor will insert a nasogastric tube until your baby’s intestine works properly.
- Nutrition via NG tube to avoid malnourishment
Survival Rate
Your baby’s survival depends upon the defect’s size and the associated abnormalities. Therefore, babies with large omphaloceles and associated congenital anomalies have a higher mortality rate than others. Babies with protrusion of the liver with omphalocele also show poor prognosis. The overall prognosis of this syndrome is good enough (80%) due to prenatal diagnosis through ultrasonography.7Malhotra, R., Malhotra, B., & Ramteke, H. (2023). Enhancing Omphalocele Care: Navigating Complications and Innovative Treatment Approaches. Cureus, 15(10), e47638. https://doi.org/10.7759/cureus.47638
Complications of Omphalocele
There are some complications related to this condition, depending on the size and time of occurrence. Large omphalocele can be ruptured, causing injury to the baby’s liver and other organs that increase the mortality.
Infants with this condition have small thorax; therefore, hypoplasia of the lungs can occur. Thus, mechanical ventilation is necessary until the baby’s lungs mature.
Babies with omphalocele are on total parenteral nutrition (TPN) through the catheter. Because they can not be tolerated orally, cholestasis and hepatomegaly (large liver size) can occur.
Large omphalocele required staged repair. Therefore, tracheostomy is sometimes indicated to maintain the airway until your baby’s lungs mature.8Fogelström, A., Caldeman, C., Oddsberg, J., Löf Granström, A., & Mesas Burgos, C. (2021). Omphalocele: national current birth prevalence and survival. Pediatric Surgery International, 37(11), 1515–1520. https://doi.org/10.1007/s00383-021-04978-z
Other complications can also occur, and these are:
- Difficulty in feeding
- Failure to thrive
- Inguinal hernia
- Gastroesophageal reflux disease (GERD)
- Esophagitis
When can I feed my baby with Omphalocele?
You can feed your baby with breast or formula milk when your baby’s intestine has healed properly. First, you have to give a small amount of breast or formula milk to check whether your baby tolerates it. If your child tolerates it, gradually increase the amount of breast milk or formula milk.
Your doctor will remove An IV catheter when your child takes and tolerates enough food orally to meet his daily nutrient requirements.
How can I Prevent having Omphalocele?
You can prevent this condition by adopting a healthy lifestyle and participating in activities that help reduce the chances of complications during pregnancy.
- Stop smoking
- Stop drinking alcohol
- Maintain your body mass index (BMI)
When should I call my Doctor?
You can call your doctor whenever you see the following signs and symptoms in your baby. These are:
- Blackening of the wound (necrosis)
- Discharge from the wound
- High-grade fever
- Greenish color vomiting
- When your child can not tolerate orally
Omphalocele vs Gastroschisis
Omphalocele is a congenital defect of the abdominal in which the abdominal contents (intestine, gallbladder, liver) herniate into the umbilical cord. The number of contents in the cord depends upon the size of the defect.
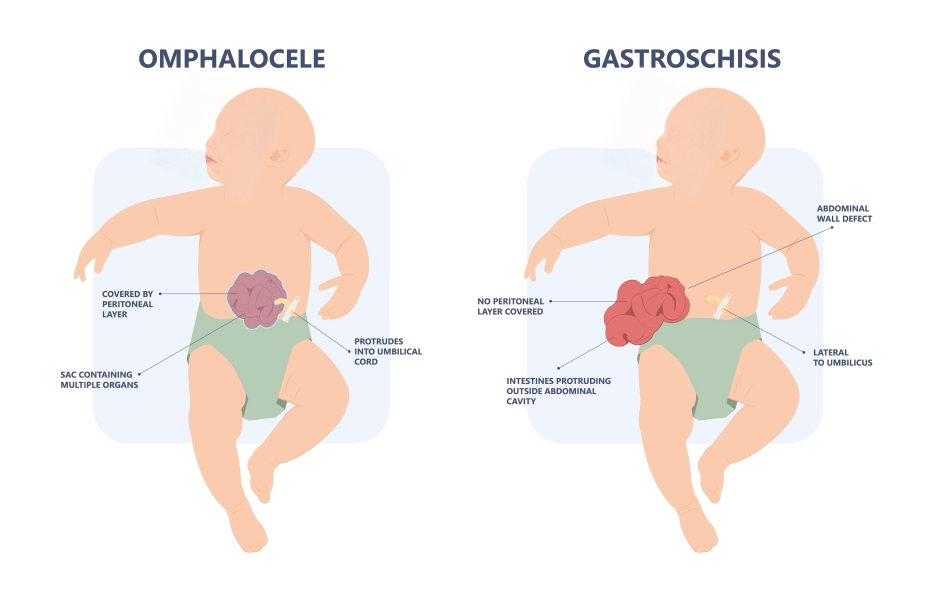
Gastroschisis also looks the same as omphalocele, but in this congenital anomaly, there is a weakness (defect) of the abdominal wall muscle near the umbilicus (belly button) through which the abdominal contents (intestine) protrude. In gastroschisis, a thin layer of membrane does not cover the abdominal contents. Surgical repair of the defect is the treatment of choice.
Omphalocele vs. Umbilical Hernia
Omphalocele is a congenital disorder. A weakness of the central abdominal muscles of your baby’s abdominal wall causes it. The contents of the intestine are outside the abdomen and covered by a thin translucent layer of membrane. Omphalciele is mostly common in newborn infants. It does not occur in adults.
Umbilical hernia can also occur in infants, neonates, and adults. In an umbilical hernia, there is a defect in the muscle of the abdominal wall but not in the skin. Therefore, the abdominal contents protrude outside the abdomen and are covered by the skin. This hernia has a clinical correlation with coughing, laughing, and sneezing. During this condition, this hernia becomes bigger and more prominent.
Conclusion
To conclude, this condition is a congenital defect in which abdominal contents come out of the abdominal wall, and a thin membrane layer covers them. Alcohol intake, obesity, smoking, and antidepressants are the risk factors for this condition. The prognosis of this condition depends on the type of omphalocele. The presence of a small omphalocele with a timely prenatal diagnosis has a higher prognosis. Surgery is the treatment of choice for omphalocele.
Refrences
- 1Kirby, R. S. (2017). The prevalence of selected major birth defects in the United States. Seminars in Perinatology, 41(6), 338–344. https://doi.org/10.1053/j.semperi.2017.07.004
- 2Zahouani, T. (2023, May 23). Omphalocele. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK519010/#:~:text=Thus%2C%20large%20omphaloceles%20need%20a,gastroesophageal%20reflux%2C%20and%20occasionally%20esophagitis.
- 3Omphalocele. (n.d.). https://www.nationwidechildrens.org/conditions/omphalocele-fc
- 4Ţarcă, E., Cojocaru, E., Trandafir, L. M., Luca, A. C., Tiutiucă, R. C., Butnariu, L. I., Costea, C. F., Radu, I., Moscalu, M., & Ţarcă, V. (2022). Current Challenges in the Treatment of the Omphalocele-Experience of a Tertiary Center from Romania. Journal of Clinical Medicine, 11(19), 5711. https://doi.org/10.3390/jcm11195711
- 5Verla, M. A., Style, C. C., & Olutoye, O. O. (2019). Prenatal diagnosis and management of omphalocele. Seminars in pediatric surgery, 28(2), 84–88. https://doi.org/10.1053/j.sempedsurg.2019.04.007
- 6Facs, J. G. G. M. M. (n.d.). Pediatric omphalocele and gastroschisis (Abdominal wall Defects) treatment & management: approach considerations, medical care, surgical care. https://emedicine.medscape.com/article/975583-treatment#d1
- 7Malhotra, R., Malhotra, B., & Ramteke, H. (2023). Enhancing Omphalocele Care: Navigating Complications and Innovative Treatment Approaches. Cureus, 15(10), e47638. https://doi.org/10.7759/cureus.47638
- 8Fogelström, A., Caldeman, C., Oddsberg, J., Löf Granström, A., & Mesas Burgos, C. (2021). Omphalocele: national current birth prevalence and survival. Pediatric Surgery International, 37(11), 1515–1520. https://doi.org/10.1007/s00383-021-04978-z

