Glomerular disease refers to a set of diseases that affect the filtering elements of the kidney, the glomeruli. Damaged glomeruli cannot filter the blood, resulting in the excretion of plasma proteins and sometimes red blood cells in the urine. Moreover, it leads to waste and water accumulation in the body and causes edema. Long-standing glomerular disease gives rise to serious complications and permanent loss of kidney function.
What is Glomerular Disease?
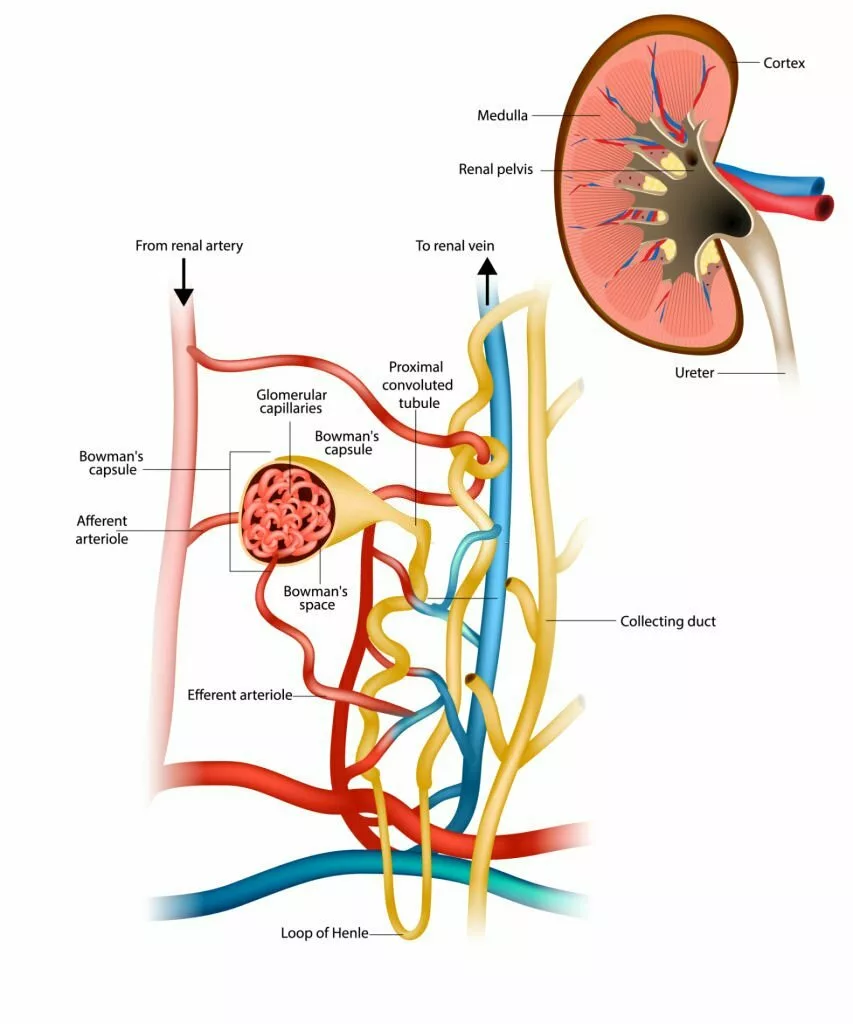
Glomerular disease refers to a group of conditions that affect the kidney’s filtering structures, the glomeruli—tiny clusters of capillaries within each nephron responsible for filtering waste, excess fluids, and toxins from the blood. Each kidney contains about a million glomeruli, which play a crucial role in maintaining fluid balance and removing harmful substances.1Murray IV, Paolini MA. Histology, Kidney and Glomerulus. [Updated 2023 Apr 17]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK554544/ When the glomeruli are impaired, proteins—particularly albumin—and sometimes red blood cells leak into the urine. The loss of albumin disrupts fluid balance, leading to swelling in various parts of the body. Common symptoms include edema, foamy or pink-tinged urine, and high blood pressure.
Glomerular Disease Causes
This disease can be due to a disease directly affecting the kidney or another underlying medical condition. Also, glomerular disease can either be acute or chronic. Some common causes of glomerular disease are:
- Infections
- Medications that damage the kidneys.
- Diseases that cause inflammation and sclerosis in the glomeruli.
- Diseases that infect the entire body and also the kidneys, for example, diabetes and lupus.
- Unknown cause (idiopathic glomerular disease)
Glomerular Disease Symptoms
Following are some characteristic symptoms that appear in individuals affected by glomerular disease:
- Proteinuria: Damaged glomeruli cannot filter proteins in the blood, thus causing leakage of proteins in urine. Urine containing plasma proteins appears foamy.2Cameron, S. (2008) Proteinuria and progression in human glomerular diseases, Karger Publishers. Retrieved 18 November 2023 https://karger.com/ajn/article-abstract/10/Suppl.%201/81/24312/Proteinuria-and-Progression-in-Human-Glomerular?redirectedFrom=PDF
- Hematuria: Glomerular disease causes the drainage of blood cells in urine, i.e., hematuria. Blood in urine renders it pink or light brown in colour.
- Oedema: Diseased glomeruli cannot excrete sufficient fluid, resulting in fluid accumulation in the body, i.e., edema. Fluid retention causes swelling in body areas like the hands, face, and ankles.
- Raised Blood pressure
- Inefficient filtration causes uremia, i.e., the accumulation of toxins in the blood.
- Acidosis (abnormal pH regulation of blood)
- Anaemia (due to reduced red blood cell production)
Glomerular Disease Diagnosis
Your physician would initially take a medical history. They might recommend a urine or a blood test to look for the primary signs of glomerular disease. Additionally, they might recommend an ultrasound or kidney biopsy to determine the nature and extent of glomerular disease.
Urinalysis
Urine is analysed for proteins and blood cells; a positive result indicates glomerular disease. White blood cells (leukocytes) in urine indicate a kidney infection. Pink-colored urine shows red blood cells, and foamy urine shows proteins in the urine. All these findings suggest damaged glomeruli and reduced kidney function.
Blood Tests
Blood tests evaluate parameters like plasma protein level, creatinine, and urea nitrogen. A reduction in plasma protein levels is a sign of protein leakage in the urine. Moreover, elevated levels of serum creatinine show reduced kidney function. A high blood urea nitrogen level is due to the accumulation of wastes in the blood, i.e., uremia.
Glomerular Filtration Rate (GFR) Test
The GFR test is the most accurate test for evaluating kidney activity. It measures the rate of blood filtration from the kidney. Unhealthy glomeruli filter blood at a rate lower than the normal glomerular filtration rate. The GFR test is complex to perform directly, so it is not usually preferred.
A more feasible way is to determine the estimated GFR based on the level of waste products in the blood. Creatinine levels in the blood are commonly used to estimate the glomerular filtration rate. It is a muscle breakdown product that accumulates in the blood in cases of declining kidney function. Creatinine levels in the blood depend on various factors, like diet, muscle size, activity, metabolism, etc.
However, some professionals consider Cystatin C3Rigalleau a e, V. et al. (2008) Cystatin C improves the diagnosis and stratification of chronic kidney disease, and the estimation of glomerular filtration rate in diabetes, Diabetes & Metabolism. Retrieved 18 November 2023 https://www.sciencedirect.com/science/article/abs/pii/S1262363608001468 a more accurate parameter for determining GFR. Cystatin C is a protein independent of muscle activity, size, and diet.
Imaging Tests
Ultrasound is the most commonly used imaging technique for the assessment of kidney function. Confirming the glomerular disease after the initial signs of blood and proteins in the urine and a reduced GFR is recommended. Moreover, it shows the size of the kidneys and helps estimate the duration of kidney disease.
Kidney Biopsy
The kidney biopsy involves removing a minor section of the renal cortex (which contains glomeruli) of the kidney with a certain needle. The removed tissue is observed under the microscope for signs of renal damage. Any inflammation, protein deposition, or scarring indicates glomerular disease. Kidney biopsy is a preferable option for the differential diagnosis of various kidney diseases.4Jennette M.D, J.C. et al. (2005) Diagnosis and management of Glomerular Diseases, Medical Clinics of North America. Retrieved 17 November 2023 https://www.sciencedirect.com/science/article/abs/pii/S0025712505705381
Glomerular Disease Treatment & Management
The treatment options for glomerular disease aim to relieve symptoms, lower the risk of complications, and delay the damage caused to the kidneys. There is no particular treatment for all types of glomerular diseases, as it depends on the cause and severity of the disease. Following are some general strategies for the management of all types of glomerular diseases:
Controlling Blood Pressure
Your healthcare provider would prescribe you medications to lower your blood pressureas maintaining optimal blood pressure reduces strain on the kidneys, minimizes protein loss, and helps slow disease progression. Angiotensin-converting enzyme (ACE) inhibitors and angiotensin II receptor blockers (ARBs) are commonly used for this purpose.5Maki, D.D. (1995) Long-term effects of antihypertensive agents on proteinuria and renal function, Archives of Internal Medicine. Retrieved 17 November 2023 https://jamanetwork.com/journals/jamainternalmedicine/article-abstract/620558 Additionally, they might order a diuretic to remove excess waste from the body along with fluid and ultimately reduce blood pressure. In severe cases, two or more medicines are required for sufficient blood pressure control.
Dietary Modification
If you have glomerular disease, your physician might recommend various dietary modifications to avoid the worsening of symptoms.
- Limit salt consumption
- Reduce fluid intake
- Take low-protein diet
- Avoid saturated fats to reduce blood cholesterol
Immunosuppression
It is a common practice to prescribe immunosuppressants to manage kidney disease caused by a problem in the immune system. Immunosuppressive agents make the immune system less responsive and reduce inflammation. Commonly recommended immunosuppressants are corticosteroids, cyclophosphamide6RJ;, D.J. (1993) Immunosuppressive drug therapy in lupus nephritis, American journal of kidney diseases : the official journal of the National Kidney Foundation. Retrieved 17 November 2023 https://pubmed.ncbi.nlm.nih.gov/8447299/, rituximab, etc.
Other Treatment Options
Other treatment options may include medications to treat the underlying disease that causes glomerular damage. In case of kidney failure, the only available option is either dialysis or kidney transplant. Some commonly prescribed medications are:
- Statins to reduce blood cholesterol
- Antibiotics for treating bacterial and viral infections that may cause glomerular disease
- Sodium-glucose transporter 2 (SGLT-2) inhibitors to treat diabetic nephropathy
- Dialysis or kidney transplant (to treat kidney failure)
Glomerular Disease Classification
This diseases come in two main forms: nephritic and nephrotic syndrome. Nephritic and nephrotic syndromes have different clinical presentations but have a common symptom: proteinuria. A normal kidney excretes 150 mg of protein daily, but a kidney with diseased glomeruli excretes more protein than normal. Glomerular disease adversely affects the kidney’s filtration function, leading to the excretion of proteins in urine.
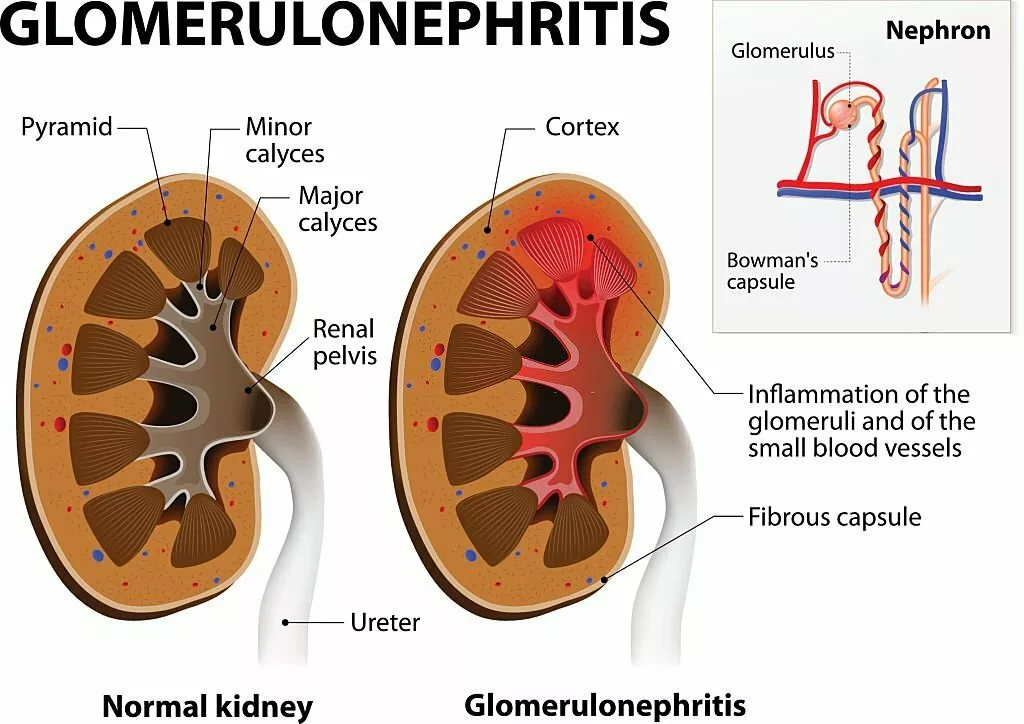
Nephritic Syndrome (Glomerulonephritis):
Glomerulonephritis is an inflammatory glomerulopathy caused by an infection or immune response. Nephritic syndrome is a clinical condition presented by hematuria (evident under the microscope) and proteinuria (>2g/day).7 Bitzan, M. (1970) Glomerular diseases, SpringerLink. Retrieved 17 November 2023 https://link.springer.com/chapter/10.1007/978-3-642-12483-9_3 Individuals with mild nephritic syndrome might be asymptomatic for many years until blood and protein become visible in the urine. In severe cases of nephritic syndrome, individuals present with hematuria, proteinuria, declining kidney function, and edema. Nephritic syndrome is commonly caused by conditions like lupus, immunoglobulin A (IgA) nephropathy8 Rosen, S. et al. (1981) Glomerular disease – ScienceDirect, Glomerular disease, Human Pathology, Volume 12, Issue 11. Retrieved 17 November 2023 https://www.sciencedirect.com/science/article/abs/pii/S0046817781802535, C3 glomerulopathy, Alport syndrome, and vasculitis.
Nephrotic Syndrome:
Nephrotic syndrome is a non-inflammatory glomerular syndrome caused by metabolic or systemic disorders like diabetes, neoplasia, and hypertension. Protein in the urine is the hallmark of nephrotic syndrome. Individuals with nephrotic syndrome commonly show proteinuria (>3.5g/day) but rarely blood in urine (hematuria). Moreover, there is a decline in kidney function, along with low serum albumin, high blood cholesterol, and edema, in nephrotic syndrome. Nephrotic syndrome results from conditions such as diabetic nephropathy, IgA nephropathy, focal segmental glomerulosclerosis, and primary amyloidosis.
Prognosis of Glomerular Disease
Early diagnosis and treatment of this disease results in a better outcome. The target of treatment is to retard the damage to the kidney and preserve the normal kidney function. The ultimate solution is dialysis or kidney transplant if the disease worsens and causes kidney failure.
Complications of Glomerular Disease
This disease advances slowly over time but can cause serious complications in the long run. Some common complications are:
- Hypertension: There is a persistent rise in blood pressure due to salt and water retention in the body.
- Chronic kidney disease (CKD): Chronic kidney disease is due to the progressive loss of kidney function with a reduced ability to remove waste products from the body. CKD is the most serious complication of glomerular disease.
- Nephrotic syndrome: This condition is clinically manifested as symptoms like high blood cholesterol, low plasma albumin levels, high protein concentration in urine, and swelling in the body due to fluid accumulation.
- Kidney failure: Kidney failure occurs when more than 85% of kidney function is lost. Symptoms like nausea, loss of appetite, vomiting, and intense swelling occur as a result of kidney failure.
Glomerular Vs. Tubular Disease
Glomerular disease primarily occurs as inflammatory and non-inflammatory glomerulopathies. However, secondary glomerular disease may result from tubular disease. Tubular disease, often termed tubulointerstitial disease, involves renal tubules and interstitium. Tubular disease is mostly idiopathic, but it may be due to an infection, drug toxicity, inflammation, or stress on tubules due to urinary obstruction.
Unlike the nephritic and nephrotic forms of glomerular disease, tubular disease comprises tubular atrophy, immune cell infiltration, and interstitial fibrosis.9 López-Novoa, J.M. et al. (2011) Etiopathology of chronic tubular, glomerular and renovascular nephropathies: Clinical Implications – Journal of Translational Medicine, BioMed Central. Retrieved 16 November 2023 https://translational-medicine.biomedcentral.com/articles/10.1186/1479-5876-9-13#:~:text=In%20early%20stages%2C%20glomerular%20filtration,GFR%20%5B45%E2%80%9347%5D. In glomerular disease, hypertension develops initially; however, tubular disease causes hypertension at an advanced stage. The protein excretion rate in glomerular disease can exceed up to 20 g/ day, while in tubular disease, the kidneys excrete less than 2 g of protein a day.
Final Words
Various medical and physiological conditions can damage the glomeruli. It is important to notice the initial signs of glomerular disease and consult a healthcare professional to avoid irreversible glomerular damage. Untreated glomerular disease may progress to chronic kidney disease and kidney failure. Adopt a healthy lifestyle to avoid circumstances that may damage your kidneys.
Refrences
- 1Murray IV, Paolini MA. Histology, Kidney and Glomerulus. [Updated 2023 Apr 17]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK554544/
- 2Cameron, S. (2008) Proteinuria and progression in human glomerular diseases, Karger Publishers. Retrieved 18 November 2023 https://karger.com/ajn/article-abstract/10/Suppl.%201/81/24312/Proteinuria-and-Progression-in-Human-Glomerular?redirectedFrom=PDF
- 3Rigalleau a e, V. et al. (2008) Cystatin C improves the diagnosis and stratification of chronic kidney disease, and the estimation of glomerular filtration rate in diabetes, Diabetes & Metabolism. Retrieved 18 November 2023 https://www.sciencedirect.com/science/article/abs/pii/S1262363608001468
- 4Jennette M.D, J.C. et al. (2005) Diagnosis and management of Glomerular Diseases, Medical Clinics of North America. Retrieved 17 November 2023 https://www.sciencedirect.com/science/article/abs/pii/S0025712505705381
- 5Maki, D.D. (1995) Long-term effects of antihypertensive agents on proteinuria and renal function, Archives of Internal Medicine. Retrieved 17 November 2023 https://jamanetwork.com/journals/jamainternalmedicine/article-abstract/620558
- 6RJ;, D.J. (1993) Immunosuppressive drug therapy in lupus nephritis, American journal of kidney diseases : the official journal of the National Kidney Foundation. Retrieved 17 November 2023 https://pubmed.ncbi.nlm.nih.gov/8447299/
- 7Bitzan, M. (1970) Glomerular diseases, SpringerLink. Retrieved 17 November 2023 https://link.springer.com/chapter/10.1007/978-3-642-12483-9_3
- 8Rosen, S. et al. (1981) Glomerular disease – ScienceDirect, Glomerular disease, Human Pathology, Volume 12, Issue 11. Retrieved 17 November 2023 https://www.sciencedirect.com/science/article/abs/pii/S0046817781802535
- 9López-Novoa, J.M. et al. (2011) Etiopathology of chronic tubular, glomerular and renovascular nephropathies: Clinical Implications – Journal of Translational Medicine, BioMed Central. Retrieved 16 November 2023 https://translational-medicine.biomedcentral.com/articles/10.1186/1479-5876-9-13#:~:text=In%20early%20stages%2C%20glomerular%20filtration,GFR%20%5B45%E2%80%9347%5D.

