Intracranial hematoma is a serious and life-threatening condition characterized by the collection of blood in the brain. It is usually caused by leakage of blood from a burst vessel in the brain or due to any head injury. Intracranial hematoma needs an emergency intervention to avoid adverse effects.
The brain is a vital organ of your body enclosed in a bony skull. The skull protects your brain from direct injury. Injury to your head can cause damage to your brain either by directly hitting the skull bone or by hematoma formation. Hematoma exerts pressure on your brain tissue or vessels and causes brain injury, possibly leading to brain function loss.
This blog provides an easy understanding of signs and symptoms, types, causes, risk factors, and treatment of intracranial hematoma. Let’s get into the details of intracranial hematoma.
Classification of Intracranial Hematoma
Intracranial hematoma is classified into three different types according to the location. 1Intracranial Hematoma. (2021, July 21). Columbia Neurosurgery in New York City. https://www.neurosurgery.columbia.edu/patient-care/conditions/intracranial-hematoma These are:
- Subdural hematoma
- Epidural hematoma
- Intracerebral hematoma
Before getting into the details of intracranial hematoma, it is necessary to discuss the layers of the meninges. There are three layers of the brain’s meninges.
- Dura mater (outermost layer)
- Arachnoid mater (middle layer)
- Pia mater (innermost layer)
Intracranial hematoma is divided into subtypes according to its location in different brain parts.
Subdural Hematoma
A subdural hematoma is formed when clotted blood is collected between the skull and the outer layer of the brain meninges (dura mater). It occurs due to trauma to the head or rupture of the vessel, leading to accumulation of blood in subdural space.
About 25% of the people present in clinical emergencies after head injuries with subdural hematoma. 2Tenny, S. (2023, February 13). Intracranial Hemorrhage. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK470242/ Subdural hematoma is further divided into three types:
- Acute:
It is a life-threatening form of subdural hematoma. Its symptoms usually begin to appear right after a few hours of injury. It should be diagnosed early and treated accordingly to avoid major side effects. It can also cause the patient’s death if left untreated. - Subacute:
As the name indicates, it is a less severe subdural hematoma. Its symptoms begin after a few days or weeks of head injury. - Chronic:
It usually affects older people. Symptoms of chronic hematoma appear late, like after a week or a couple of months after a head injury. It most commonly remains asymptomatic and is diagnosed on a dating CT scan.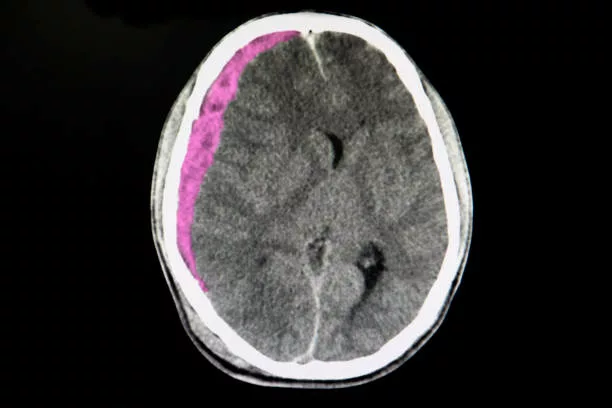
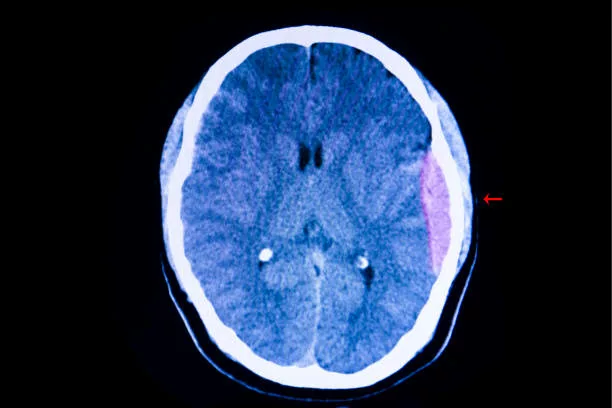
A CT scan of the brain of a patient with a traffic accident shows acute subdural hematoma. Intracerebral hemorrhage.
Epidural Hematoma
An epidural hematoma is also known as an extradural hematoma. It is a traumatic or pathological blood collection between the skull’s inner part and the stripped-off layer of the dural membrane. 3Fana, D. S. L. M. F. F. (n.d.). Epidural Hematoma: Background, Pathophysiology, Epidemiology. https://emedicine.medscape.com/article/1137065-overview#:~:text=Epidural%20hematoma%20complicates%202%25%20of,remained%20stable%20over%20many%20years
Pathological causes of epidural hematoma include infections, brain abscesses, malformation of vessels, brain tumors, and coagulopathies (bleeding disorders).
An epidural hematoma accounts for only 2% of cases, followed by head trauma (about 40000 cases/year). Head trauma can be due to accidental falls, head collisions with hard objects, and physical assault.
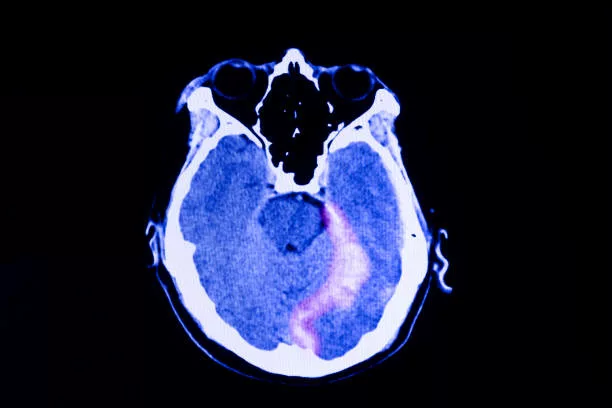
Intracerebral Hematoma:
An intracerebral hematoma is a collection of blood inside the brain parenchyma. A cerebral contusion can also cause an intracerebral hematoma. It is usually caused by hypertension (high blood pressure) and amyloid angiopathy. Basal ganglions are the most common site for intracerebral hematoma. It causes primary tissue damage and secondary tissue damage. Primary damage is due to neuronal injuries and edema, while secondary damage occurs due to cellular breakdown.
Subdural Hematoma vs. Intracranial Hemorrhage
Subdural hematoma and intracranial hemorrhage are both serious and life-threatening medical emergencies due to bleeding in the brain or skull. A subdural hematoma occurs due to the collection of blood between the outer layer of the brain and the dura mater. This can be due to head trauma or bleeding disorders.
In comparison, intracranial hemorrhage occurs due to bleeding from ruptured vessels in the brain tissues. Various factors, including trauma, aneurysms, stroke, and hypertension (high blood pressure), can cause a hematoma. Emergency medical attention is required for both of these conditions. Intracranial hematoma and intracranial hemorrhage have different treatment approaches. The prognosis depends on the underlying cause, affected site, and severity of the condition.
Concluding, intracranial hematoma is defined as an enclosed blood clot between the skull and layers of the brain, while intracranial hemorrhage is not enclosed bleeding; it is profuse bleeding from the ruptured artery.
How is Intracranial Hematoma Formed?
Intracranial hematoma is formed when there is an injury to the brain or a rupture of the vessels due to chronic hypertension. When the vessels rupture, the blood leaks into the surroundings and collects in a space that forms a hematoma.
Intracranial Hematoma & Aneurysm
Hematoma results when the vessels burst and blood leaks into the surrounding tissues in an enclosed space, forming a hematoma. It is usually in the clotted form. An aneurysm (cerebral aneurysm) is the ballooning or bulging of the vessels due to weakness in the vessel wall.
A ruptured aneurysm leads to potentially fatal hemorrhagic stroke or subarachnoid hemorrhage. Intracranial hematoma and aneurysm are different conditions but usually present with the same symptoms. These symptoms include headaches, drowsiness, nausea and vomiting, and confusion.
What are the Causes & Risk Factors of Intracranial Hematoma?
Causes:
Head injury followed by a road traffic accident (contusion and collision)is the most common cause of intracranial hematoma. It can also result from physical assault. Other causes include vascular abnormalities that lead to rupture of the vessels, infections, bleeding disorders, brain tumors, and hypertension.
Risk factors:
Multiple risk factors are involved in the formation of intracranial hematoma. These are:
- Chronic hypertension
- Positive family history of intracranial hematoma
- Heavy alcohol drinking
- Smoking
- Aneurysm
- Aging
- Strenuous exercises
- Arteriovenous malformation
- Coagulopathy
- Use of medications that affect blood coagulation
- Use of blood thinners
Signs & Symptoms of Intracranial Hematoma
Signs and symptoms of intracranial hematoma may begin right after the head injury, or it can take a few days or weeks to appear. With time, hematoma exerts pressure on the surrounding structures of your brain. Indicators of expanding hematoma are:
- Progressive worsening of headache
- Drowsiness and loss of consciousness that can be progressive or sudden
- Progressive weakness of the limbs
- Deterioration of health
- Nausea and vomiting
If the general status of a person with intracranial hematoma deteriorates further, it is a warning sign.
Other common symptoms of intracranial hematoma are:
- Vomiting
- Confusion
- Fits
- Apathy
- Difficulty speaking
- Limb paralysis
- Lethargy
- Difficulty walking
- Dementia (loss of memory)
- Skin color changes
- Sweating
- Irritability
- One pupil size is greater than the other
When to See Your Doctor?
Immediately book your appointment with your neurosurgeon if you have these symptoms:
- Seizures or convulsions
- Loss of consciousness
Early diagnosis and prompt treatment can save the life of patients.
How to Diagnose Intracranial Hematoma?
The following methods are used to diagnose intracranial hematoma:
CT Scan:
It is one of the best radiological techniques to diagnose intracranial hematoma in emergencies. The findings of the CT scan are different depending on the location and size of the hematoma.
Subdural hematoma is concave or crescent-shaped (also called banana-shaped). While epidural hematoma is convex (lemon-shaped).
Magnetic Resonance Imaging (MRI):
This radiological imaging technique is used to diagnose intracranial hematoma that remained undiagnosed on a CT scan.
CT Angiography:
CT angiography is one of the best modalities to diagnose intracranial hematoma. It indicates the exact location of the hematoma, its extent, and the location of the ruptured artery.
Other Investigations:
Apart from radiological imaging techniques, other investigations rule out the other causes of intracranial hematoma. These investigations are :
- Complete blood profile
- Coagulation profile
- Liver function tests (LFTs)
- Renal parameters
- Serum albumin level
- Serum creatinine level
- ECG
How will you Treat Intracranial Hematoma?
Treatment of intracranial hematoma depends on the severity of the disease and the size of the hematoma. Small-size hematomas require conservative management without any surgical intervention. Surgery is the treatment of choice for large-size hematomas. The treatment protocol is as follows:
Immediate:
Doctors follow ABCDE protocol if the person presents to the emergency department right after a road traffic accident leading to head injury or traumatic brain injury (TBI).
ABCDE Protocol:
- Secure airways if compromised
- Maintain breathing
- Maintain circulation
- Check for disability
- Exposure of the body
Definitive Treatment:
Definite treatment or the treatment of choice for intracranial hematoma is surgical treatment. This surgical procedure is :
Burr Hole Trephination:
It is an invasive surgical procedure in which surgeons drill a hole in the skull and remove a hematoma.
Craniotomy:
In this surgical intervention, a part of the skull is removed to reduce pressure and is replaced after the procedure.
Craniectomy:
It is a surgical procedure that includes removing a part of the skull for some time to allow swelling of the brain and replacing it when the swelling subsides without harming the brain itself. Decompressive craniectomy is suitable for patients with subdural hematoma with a poor prognosis. 4Kwon, Y. S., Yang, K. H., & Lee, Y. H. (2016). Craniotomy or Decompressive Craniectomy for Acute Subdural Hematomas: Surgical Selection and Clinical Outcome. Korean journal of neurotrauma, 12(1), 22–27. https://doi.org/10.13004/kjnt.2016.12.1.22
Follow-up:
A regular follow-up can prevent postoperative complications.
Take the following measures to hasten your recovery:
- Complete bed rest
- Good sleep
- Raise the head side of the affected person to minimize the risk of brain edema.
- Stay hydrated
- Noise-free area
- Avoid drinking alcohol
- Stop smoking
Preventive Measures
Ensure the following preventive measures for traumatic injuries to minimize the risk of injury.
- Wear helmets to avoid head injury in road traffic accidents
- Don’t cross your speed limit
- Wear seat belts
- Avoid driving if you are drunk
- Carefully cross the road
If you have hypertension, keep track of your blood pressure. Take your medications daily to prevent intracranial hemorrhage and intracranial hematoma. Moreover, it is critical to promptly treat nose and ear infections to avoid infection in the brain and abscess formation.
Complications of Intracranial Hematoma
As we have discussed, intracranial hematoma is a life-threatening emergency. If it remains undiagnosed and untreated, it can cause the following complications:
5Subdural hematoma : MedlinePlus Medical Encyclopedia. (n.d.). https://medlineplus.gov/ency/article/000713.htm#:~:text=Possible%20Complications&text=Brain%20herniation%20(pressure%20on%20the,permanent%20weakness%2C%20numbness%2C%20difficulty%20speaking
- Brain herniation
- Brain edema
- Respiratory arrest
- Brain death in late cases
- Death of the patients
Long-term complications of intracranial hematoma are:
- Headaches
- Anxiety and depression
- Motor deficits or paralysis of extremities
- Hydrocephalus (excessive cerebrospinal fluid in the fluid)
- Speech and language problems
- Vision problems
- Epilepsy
What is the Most Dangerous Type of Intracranial Hematoma?
Subdural hematoma is the most dangerous type of intracranial hematoma. Its symptoms usually appear after weeks or even months, making its diagnosis and treatment more challenging. It has several associated risk factors. Moreover, its treatment is also difficult.
When blood accumulates in the space between the brain and the outermost layer of the brain, also called dura matter, subdural hematoma is formed. Subdural hematoma exerts pressure on the surrounding brain structures, leading to various neurological problems, including paralysis of limbs.
Certain risk factors increase the incidence of subdural hematoma formation. These factors include older age, alcohol abuse, use of medications that alter the viscosity of the blood, and a history of trauma leading to head injury.
Subdural hematomas have a poor prognosis and higher mortality rate than other
hematomas. Its prognosis is poor in older patients with comorbidities like heart disease, diabetes, and hypertension. Additionally, surgical interventions are necessary to remove the hematoma if its size is large. Brain surgery for intracranial hematoma removal is a serious and life-threatening surgery due to the involvement of the dura mater. Postoperative complications like bleeding or infection are also challenging.
What are Some Long-Term Effects of Intracranial Hematoma?
The recovery process of intracranial hematoma is slow; it takes about three months or more to recover. There is no surety about the full recovery of the patient. There are some long-term effects that you can suffer even after the recovery, and these are:
- Limb weakness
- Limb paralysis
- Walking difficulty
- Short-term or long-term memory problems
Conclusion
Intracranial hematoma is an emergency most commonly caused by head injuries in road traffic accidents. Hematoma has a pressure effect on the brain tissues that causes brain damage. Diagnosing and treating it early is crucial to minimize complications and side effects. CT scan is the investigation of choice to diagnose intracranial hematoma. Surgical removal of the hematoma is the treatment of choice if surgical intervention is needed.
Refrences
- 1Intracranial Hematoma. (2021, July 21). Columbia Neurosurgery in New York City. https://www.neurosurgery.columbia.edu/patient-care/conditions/intracranial-hematoma
- 2Tenny, S. (2023, February 13). Intracranial Hemorrhage. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK470242/
- 3Fana, D. S. L. M. F. F. (n.d.). Epidural Hematoma: Background, Pathophysiology, Epidemiology. https://emedicine.medscape.com/article/1137065-overview#:~:text=Epidural%20hematoma%20complicates%202%25%20of,remained%20stable%20over%20many%20years
- 4Kwon, Y. S., Yang, K. H., & Lee, Y. H. (2016). Craniotomy or Decompressive Craniectomy for Acute Subdural Hematomas: Surgical Selection and Clinical Outcome. Korean journal of neurotrauma, 12(1), 22–27. https://doi.org/10.13004/kjnt.2016.12.1.22
- 5Subdural hematoma : MedlinePlus Medical Encyclopedia. (n.d.). https://medlineplus.gov/ency/article/000713.htm#:~:text=Possible%20Complications&text=Brain%20herniation%20(pressure%20on%20the,permanent%20weakness%2C%20numbness%2C%20difficulty%20speaking

