Lupus Nephritis, often caused by systemic lupus erythematosus (SLE), is an auto-immune kidney disease.1Ramakrishnan, M. and Leslie, S.W., 2023. Thin Basement Membrane Nephropathy (Benign Familial Hematuria). In StatPearls [Internet]. StatPearls Publishing. Lupus itself is a range of autoimmune diseases that trigger your immune cells to attack your body parts. In the case of lupus nephritis, that organ is your kidneys.2Liao, Y.W., Chen, Y.M., Hsieh, T.Y., Hung, W.T., Hsu, C.Y., Wen, M.C., Chen, Y.H. and Huang, W.N., 2023. Renal Histopathology Associated with Kidney Failure and Mortality in 526 Lupus Nephritis Patients, a Long-Term Realworld Data Study. The Journal of Rheumatology.
Kidneys perform myriad biological functions, all of which are crucial for maintaining the sustainability of our lives. They release hormones that regulate blood pressure, produce active vitamin D necessary for healthy bones and muscles, make red blood cells, and, most importantly, filter out blood and balance the different minerals and salts in our blood.
The damage caused by this condition causes kidneys to prevent them from performing all of these necessary functions. This can become complicated as well, with severity causing renal failure or end-stage renal disease where patients require dialysis or kidney transplants.
Risk Factors for Lupus Nephritis
There are certain groups of people in which Lupus nephritis is more common. Ethnically, individuals originating from African, Hispanic, and Asian origins have a 2 to 3 times higher probability of developing lupus nephritis as compared to people of Caucasian descent.3Diagnosis and classification of renal disease in systemic lupus erythematosus. Up To Date website. Updated March 24, 2016. Accessed October 19, 2016 Lupus nephritis is also significantly more common in women than men.4 Hahn, B.H., Mcmahon, M.A., Wilkinson, A., Wallace, W.D., Daikh, D.I., Fitzgerald, J.D., Karpouzas, G.A., Merrill, J.T., Wallace, D.J., Yazdany, J. and Ramsey‐Goldman, R., 2012. American College of Rheumatology guidelines for screening, treatment, and management of lupus nephritis. Arthritis care & research, 64(6), pp.797-808.
This condition is a manifestation of systemic lupus erythematosus (SLE); therefore, it is much more susceptible in SLE patients. In fact, according to medical research, there is up to a 60% chance of SLE exaggerating into Lupus nephritis.5Saxena, R., Mahajan, T. and Mohan, C., 2011. Lupus nephritis: current update. Arthritis research & therapy, 13, pp.1-12. Other factors such as environment, genetics, or medications can also put you at risk of developing this disease.
Cause of Lupus Nephritis
It is an autoimmune condition. Nephritis is the inflammation of the kidneys, and if it happens with SLE, it is called lupus nephritis. Autoimmune diseases mean that the body becomes hyper-reactive to itself. The body forms antibodies, which fight cells against the body’s healthy tissue and start causing destruction. Autoimmune diseases can be idiopathic or triggered by infection, drugs, or inheritance.
Symptoms of Lupus Nephritis
Despite the severity, its symptoms are not very apparent and could sometimes even be overlooked. The most visible initial symptom is swelling in the lower body; over time, that swelling spreads to your hands and face.
Other symptoms of lupus nephritis include:
Weight Gain:
You would appear to gain weight suddenly due to fluid build-up in the body due to declining kidney function.
Swelling of the Limbs:
Also known as edema, it is the overdeposition of fluid in your limbs or the area around your eyes. Since the kidneys are not functioning properly, the body has extra fluid. The most common presentation of this swelling is lower leg edema.6Su, Y.J., Lin, I.C., Wang, L., Lu, C.H., Huang, Y.L. and Kuo, H.C., 2018. Next-generation sequencing identifies miRNA-based biomarker panel for lupus nephritis. Oncotarget, 9(46), p.27911.
Foamy Urine:
Due to glomerular malfunctioning, there is an excess of proteins in the urine. This condition is also called proteinuria and gives your urine a foamier-than-usual appearance.7Musa, R., Brent, L.H. and Qurie, A., 2018. Lupus nephritis. Foamy urine can also be due to glycosuria and sugars in urine.
Bloody Urine:
If you have lupus nephritis, your urine may have a pinkish or brown hue. This is because the glomerular disease causes blood to leak into your urine.
Fever:
Patients of LN get random spells of fever with no known cause.
Muscular & Joint Pain:
Lupus nephritis weakens the muscles and joints, resulting in inflammation and swelling, which in turn causes pain.
Hypertension:
Since lupus nephritis affects the kidneys, which help regulate blood pressure, you might see signs of high blood pressure.
Frequent Urination:
Due to kidney dysfunction, fluid builds up in the body. Therefore, the body frequently produces urine to expel it all out, especially at night.
Kidney issues frequently emerge concurrently with or shortly after the onset of lupus symptoms. These problems may manifest as:
- Joint pain or swelling
- Muscle discomfort
- Unexplained fever
- A distinctive red rash, commonly found on the face, spanning the nose and cheeks, is often called a butterfly rash due to its characteristic shape.
Stages of Lupus Nephritis
It progresses through six different stages or classifications:
Class I – Minimal Mesangial Lupus Nephritis:
This is a preliminary stage, during which only minor abnormalities under the microscope can be discovered. Your kidneys continue to perform in perfect condition, with no real symptoms.
Class II – Mesangial Proliferative Lupus Nephritis:
In this stage, the glomeruli blood vessels show mild inflammation, leading to their thickening. While your kidneys continue to work properly, mild symptoms may start appearing.
Class III – Focal Lupus Nephritis:
Here, less than half the affected glomeruli have inflammation. In focal lupus nephritis, symptoms such as foamy urine and high blood pressure may start to appear, while kidney function also begins to sabotage.
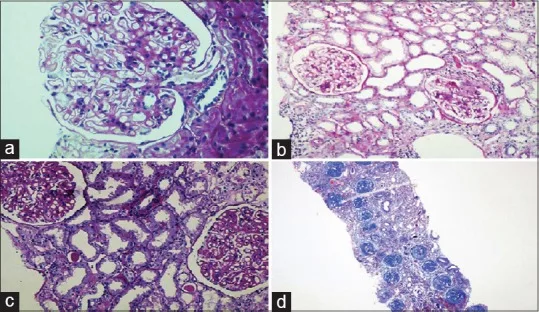
Class IV – Diffuse Lupus Nephritis:
This is where the severity of lupus nephritis begins to rise, there is widespread inflammation, and over half of the glomeruli become scarred. More severe symptoms become apparent, which can lead to serious kidney damage.
Class V – Membranous Lupus Nephritis:
In this stage, the glomerular basement membrane begins to thicken, and symptoms such as proteinuria and edema become more severe.
Class VI – Advanced Sclerosing Lupus Nephritis:
In the last and most severe stage of lupus nephritis, kidney tissue damage is at its worst, with extensive scarring and fibrosis. As a result, kidney function is also declining, and it is very probable to develop End-Stage Renal Disease (ESRD) at this point.
Every patient with LN doesn’t need to experience each of these stages; in fact, most patients will have a normal life expectancy.
Complications
Lupus Nephritis can have serious complications. The most common complication of lupus nephritis is kidney failure or permanent kidney damage. In fact, according to statistics, 49% of patients with lupus nephritis show signs of serious complications, including sepsis, cardiovascular disease, thrombosis, and avascular necrosis of bones.8Bono, L., Cameron, J.S. and Hicks, J.A., 1999. The very long-term prognosis and complications of lupus nephritis and its treatment. Qjm, 92(4), pp.211-218.
Patients are expected to lead normal lives with proper care and routine medical attention.
How Is Lupus Nephritis Diagnosed?
Lupus nephritis can be tricky to diagnose; sometimes, its symptoms are interchanging, while other times, if you are already taking medication for lupus, you can have false symptoms of lupus nephritis.
However, if symptoms are apparent, your doctor would begin your diagnosis by taking your family and medical history. They may order lab tests to help with the diagnosis. These tests include:
Urinary Test:
A urinary test is the most common diagnostic test for lupus nephritis. A urinalysis checks for unusual amounts of red or white blood cells and a high percentage of proteins in the urine. This is done via a urine dipstick. It is a bedside test that gives results in minutes. However, a 24-hour urinary protein test may be ordered if a positive result is obtained.
Blood Test:
Blood tests evaluate kidney function by measuring waste products like creatinine and urea in the blood, indicating how well the kidneys are filtering. They also assess for low blood protein levels and the presence of specific antibodies (e.g., anti-dsDNA), which are often elevated in lupus nephritis patients.
Imaging Tests:
Two main types of imaging tests are conducted on a patient with lupus nephritis: a sonogram and an intravenous pyelogram. During a sonogram, healthcare providers transmit ultrasound waves through the kidneys to assess for structural changes. In an intravenous pyelogram, the patient ingests dye, which accumulates in the kidneys. Then, x-rays reveal the dye’s location and outline the kidneys.
Kidney Biopsy:
A kidney biopsy is probably the most definitive test for diagnosing lupus nephritis.
Treatment for Lupus Nephritis
Despite all the medical equipment we have, lupus nephritis remains incurable. However, drug therapy, conservative treatments, and, in severe cases, dialysis or surgery are ways to prolong life expectancy and reduce the severity of the disease.
Dietary Changes:
Patients with lupus nephritis need to make certain immediate changes to their diet. Reducing the consumption of sodium and proteins (according to kidney function) while eating more vitamins and minerals, omega-3 fatty acids, and anti-inflammatory foods is helpful.
Hypertension Medication:
Blood pressure medications such as angiotensin-converting enzyme (ACE) inhibitors and angiotensin II receptor blockers (ARBs) help control blood pressure and prevent excessive protein leakage in the urine. These drugs block the enzymes and receptors, leading to decreased angiotensin II production and elevating blood pressure through vessel constriction. Diuretics help prevent fluid build-up by eliminating water.
Drug Therapy:
After diagnosis, your doctor will prescribe medication to weaken your immune system, preventing it from attacking healthy cells and reducing symptoms. These drugs include steroids, cyclosporine, tacrolimus, cyclophosphamide, azathioprine, mycophenolate, rituximab, and belimumab.
According to research, cyclophosphamide combined with steroids is the best way to preserve renal function in proliferative lupus nephritis.9Flanc, R.S., Roberts, M.A., Strippoli, G.F., Chadban, S.J., Kerr, P.G. and Atkins, R.C., 2004. Treatment for lupus nephritis. Cochrane Database of Systematic Reviews, (1). In another more recent study, mycophenolate is statistically determined to be most efficient in remission.10Henderson, L., Masson, P., Craig, J.C., Flanc, R.S., Roberts, M.A., Strippoli, G.F. and Webster, A.C., 2012. Treatment for lupus nephritis. Cochrane Database of Systematic Reviews, (12)
Dialysis:
Dialysis is usually used to restore kidney function. This means that the kidneys are no longer properly eliminating wastes like urea and creatinine and have become non-functional.
There are two types of dialysis: hemodialysis and peritoneal dialysis.11Gong, Y., Zhao, Y., Ran, L. and Liu, Y., 2022. Comparison Between Hemodialysis and Peritoneal Dialysis in the Risks for Disease Activity in LN-ESRD Patients: A Systematic Review and Meta-analysis. Alternative Therapies in Health & Medicine, 28(6).
Hemodialysis
Haem stands for blood. Hemodialysis is the cleaning of blood using an artificial device. The blood is taken out through tubes and then passed through a haemodialyser. Haemodialyser acts like the kidneys and cleans the blood of any toxins. It then pushes the clean blood back into the vein. Hemodialysis is a technical procedure, and we always do it in hospitals under supervision.

Peritoneal Dialysis
The peritoneal cavity is a space inside our abdomen that contains fluid. This fluid often contains waste and toxins, too. Peritoneal dialysis uses a catheter to drain the fluid in the cavity. This helps remove excessive fluid with wastes, allowing some rest for the kidneys.
One benefit of peritoneal dialysis is ease since it can be performed at home.
Surgery:
Surgery is usually the last resort for extremely severe cases where kidney function has declined significantly. Kidney transplant is the surgery of choice, requiring a donor. Despite it being a major and end-game procedure, a kidney transplant is not a permanent cure. Patients would have to continue taking immunosuppressants and lifelong monitoring, and there would still be a risk of complications.
Lifestyle & Dietary Changes:
Since this is a lifelong condition, you would have to make due lifestyle changes to not only extend your life expectancy but also improve the quality of your life.
Alongside routine check-ups and medical treatment, you must adopt a healthier and more active lifestyle, limit or stop consuming alcohol, high-cholesterol and high-sodium foods, and monitor protein intake.
If you are a smoker, you must work hard to end your addiction and stop smoking, as it can have detrimental effects on your health.
If you have symptoms of edema, you must also monitor fluid intake while making sure to remain hydrated. You should also prioritize consuming antioxidant-rich foods, foods high in minerals and vitamins, and more omega-3 fatty acids.
It is also necessary to be mindful of other medications you take so that they do not reversely affect your kidneys. Some food items, such as grapefruit, should be avoided, as they do not mix well with the therapeutic medication for lupus nephritis.
Conclusion
As a serious complication of SLE, lupus nephritis presents diverse symptoms like fatigue, frequent urination, fever, urine changes, and body swelling. It’s incurable and can lead to various complications, sometimes requiring surgery.
Advanced health care now allows better prognosis for lupus. With simple steps such as drug therapy and making lifestyle changes to be healthier, you can lead a life with fulfillment. Hence, lupus nephritis, although long-term, is treatable and manageable.
Refrences
- 1Ramakrishnan, M. and Leslie, S.W., 2023. Thin Basement Membrane Nephropathy (Benign Familial Hematuria). In StatPearls [Internet]. StatPearls Publishing.
- 2Liao, Y.W., Chen, Y.M., Hsieh, T.Y., Hung, W.T., Hsu, C.Y., Wen, M.C., Chen, Y.H. and Huang, W.N., 2023. Renal Histopathology Associated with Kidney Failure and Mortality in 526 Lupus Nephritis Patients, a Long-Term Realworld Data Study. The Journal of Rheumatology.
- 3Diagnosis and classification of renal disease in systemic lupus erythematosus. Up To Date website. Updated March 24, 2016. Accessed October 19, 2016
- 4Hahn, B.H., Mcmahon, M.A., Wilkinson, A., Wallace, W.D., Daikh, D.I., Fitzgerald, J.D., Karpouzas, G.A., Merrill, J.T., Wallace, D.J., Yazdany, J. and Ramsey‐Goldman, R., 2012. American College of Rheumatology guidelines for screening, treatment, and management of lupus nephritis. Arthritis care & research, 64(6), pp.797-808.
- 5Saxena, R., Mahajan, T. and Mohan, C., 2011. Lupus nephritis: current update. Arthritis research & therapy, 13, pp.1-12.
- 6Su, Y.J., Lin, I.C., Wang, L., Lu, C.H., Huang, Y.L. and Kuo, H.C., 2018. Next-generation sequencing identifies miRNA-based biomarker panel for lupus nephritis. Oncotarget, 9(46), p.27911.
- 7Musa, R., Brent, L.H. and Qurie, A., 2018. Lupus nephritis.
- 8Bono, L., Cameron, J.S. and Hicks, J.A., 1999. The very long-term prognosis and complications of lupus nephritis and its treatment. Qjm, 92(4), pp.211-218.
- 9Flanc, R.S., Roberts, M.A., Strippoli, G.F., Chadban, S.J., Kerr, P.G. and Atkins, R.C., 2004. Treatment for lupus nephritis. Cochrane Database of Systematic Reviews, (1).
- 10Henderson, L., Masson, P., Craig, J.C., Flanc, R.S., Roberts, M.A., Strippoli, G.F. and Webster, A.C., 2012. Treatment for lupus nephritis. Cochrane Database of Systematic Reviews, (12)
- 11Gong, Y., Zhao, Y., Ran, L. and Liu, Y., 2022. Comparison Between Hemodialysis and Peritoneal Dialysis in the Risks for Disease Activity in LN-ESRD Patients: A Systematic Review and Meta-analysis. Alternative Therapies in Health & Medicine, 28(6).

