Malignant hyperthermia is a sudden, severe onset of muscle rigidity, hypermetabolism, respiratory failure, and cardiovascular compromise in a patient in response to the anesthetic gases.
What Is Malignant Hyperthermia?
Malignant hyperthermia is a hereditary disorder of your muscle in response to the anesthetic gases or the muscle relaxant succinylcholine that your doctor uses during the induction of anesthesia. Its symptoms include muscle stiffness, tachycardia (increased heart rate), rapid breathing, low blood pressure, an increase in oxygen consumption, and a rise in body temperature. Most of these gases are halogens gases like nitrous oxide and xenon. However, non-halogen gases also cause this condition.1Rosenberg, H., Pollock, N., Schiemann, A., Bulger, T., & Stowell, K. (2015). Malignant hyperthermia: a review. Orphanet journal of rare diseases, 10, 93. https://doi.org/10.1186/s13023-015-0310-1
Incidence Of Malignant Hyperthermia
Exact statistics about the incidence of malignant hyperthermia are unknown. However, according to research, its incidence is one in one lac adults and 1 in 30,000 children. Moreover, its incidence also depends on the geographical area. It is more common in Wisconsin and the Midwest.
Moreover, its prevalence in New York is one in one lac patients having surgery.2Brady, J. E., Sun, L. S., Rosenberg, H., & Li, G. (2009). Prevalence of this condition due to anesthesia in New York State, 2001-2005. Anesthesia and analgesia, 109(4), 1162–1166. https://doi.org/10.1213/ane.0b013e3181ac1548
Causes & Risk Factors Of Malignant Hyperthermia
The following are the causes and risk factors of malignant hyperthermia:
Anesthetic Gases:
Anesthetic gases like isoflurane, halothane, sevoflurane, and desflurane cause malignant hyperthermia during the course of anesthesia.
Muscle Relaxants:
Depolarizing muscle relaxants like succinylcholine that your anaesthesiologist uses during induction of general anesthesia can also cause malignant hyperthermia.
Medical Conditions:
Certain medical conditions like sepsis, neuroleptic malignant syndrome, and King-Denborough syndrome can also cause this condition.
Family History:
A family history is also a risk factor for malignant hyperthermia during the course of anesthesia.
Past History:
If you have previous episodes of malignant hyperthermia, you are at risk of developing it in the next anesthesia.
Genetic Factors:
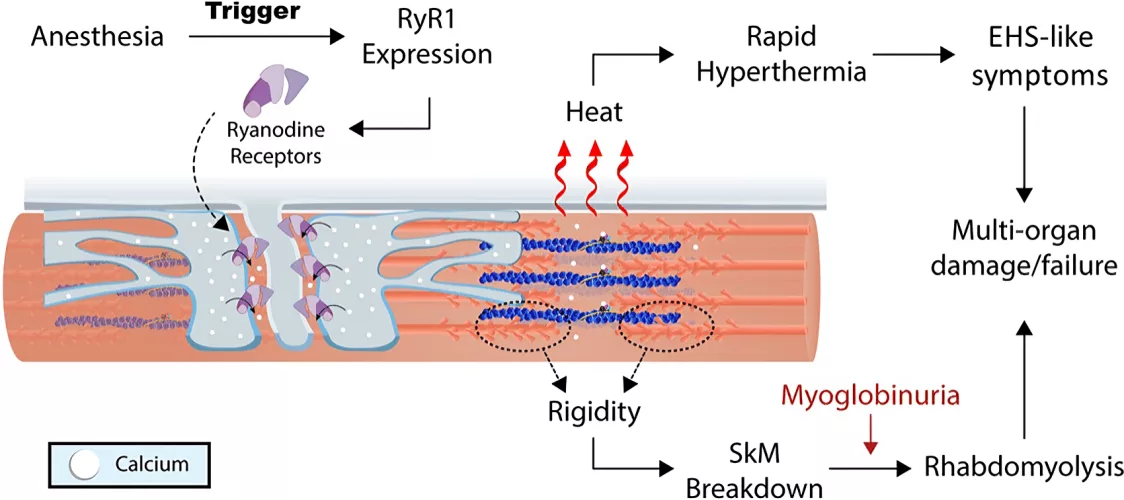
Genetic factors also play an important role in causing this condition. A mutation in the RYR1 gene that is associated with your ryanodine receptors is associated with malignant hyperthermia.3Hopkins, P. M., Gupta, P. K., & Bilmen, J. G. (2018). Malignant hyperthermia. Handbook of clinical neurology, 157, 645–661. https://doi.org/10.1016/B978-0-444-64074-1.00038-0
Other Factors:
Some factors like heat, infection, high internal body temperature, and exercise also trigger malignant hyperthermia crises.4Michelucci, A., Paolini, C., Boncompagni, S., Canato, M., Reggiani, C., & Protasi, F. (2017). Strenuous exercise triggers a life-threatening response in mice susceptible to malignant hyperthermia. FASEB journal: official publication of the Federation of American Societies for Experimental Biology, 31(8), 3649–3662. https://doi.org/10.1096/fj.201601292R
Symptoms Of Malignant Hyperthermia
Some of the symptoms are:
Initial Symptoms:
Initially, you may experience the following symptoms:
Muscle Rigidity
There is stiffness in the muscles, particularly the muscles of your jaw, limbs, and neck.
Tachycardia
Tachycardia or increased heart rate occurs in the episode of malignant hyperthermia.
Increase In Oxygen Consumption
Your body starts consuming oxygen in greater concentration, increasing oxygen demand.
Tachypnea
Your breathing rate starts increasing rapidly.
Rise In Body Temperature
The body temperature initially increases slightly but starts rising more rapidly later.
Progressive Symptoms:
With time, the symptoms start worsening, and the following symptoms appear:
Severe Hyperthermia
The temperature starts rising rapidly and may rise greater than forty-two degrees Celsius or 109 Fahrenheit.5Nelson T. E. (2001). Heat production during anesthetic-induced malignant hyperthermia. Bioscience Reports, 21(2), 169–179. https://doi.org/10.1023/a:1013696124358
Hypertension
The blood pressure of the patient starts rising rapidly.
Arrhythmias
The workload on your heart increases, showing abnormal rhythms (arrhythmias).
Seizures
Patients may experience seizures.
Sweating
The patient starts sweating profusely.
Muscle Necrosis
With time, damage to the muscle fibers occurs, and their necrosis begins. Moreover, the levels of creatine kinase rise in your body.
Vitreous Haze
The patient’s eyes may become cloudy or foggy.
Late Symptoms:
Patients may experience the following symptoms after some time if the doctors don’t start the treatment early:
- Cardiac Arrest
- Respiratory Failure
- Coma
- Multi-organ failure
- Metabolic acidosis6Larach MG, Brandom BW, Allen GC, Gronert GA, Lehman EB. Malignant hyperthermia deaths related to inadequate temperature monitoring, 2007-2012: a report from the North American malignant hyperthermia registry of the malignant hyperthermia association of the United States. Anesth Analg. 2014 Dec;119(6):1359-66. doi: 10.1213/ANE.0000000000000421. PMID: 25268394.
How Is Malignant Hyperthermia Diagnosed?
If you are at increased risk for malignant hyperthermia, your doctor will begin the diagnostic process with a comprehensive medical history and physical examination. Following this initial assessment, your doctor may recommend a range of diagnostic tests to further evaluate your condition.
History:
Your doctor may ask the following questions while taking your history :
- Did you have any previous surgery? If yes, were there any complications during the surgery? Was there any muscle stiffness or muscle problems after surgery? What kind of drugs were used in that surgery? How did your body interact with the anesthetic gases?
- Do you have a history of malignant hyperthermia? Do you have a family history of MH? Do you have a family history of any muscle disorder? Did any of your family members have a history of unusual symptoms like fever or muscle problems during surgery?
- Do you have any muscle disorder, diabetes, or hypertension?
Examination:
After a thorough history, your doctor performs a complete general physical examination along with a systemic examination, particularly focusing on your vitals, muscles, neurological, and cardiovascular systems.
Investigations:
The following investigations are important:
Caffeine Halothane Contracture Test
The gold standard investigation is the caffeine-halothane contracture test. In this test, your doctor exposes one of your live muscle fibers to caffeine or halothane and checks the response of the muscle fiber to that volatile anesthetic.7Larach, M. G., Landis, J. R., Bunn, J. S., & Diaz, M. (1992). Prediction of malignant hyperthermia susceptibility in low-risk subjects. An epidemiologic investigation of caffeine halothane contracture responses. The North American Malignant Hyperthermia Registry. Anesthesiology, 76(1), 16–27. https://doi.org/10.1097/00000542-199201000-00003
Genetic Testing
Genetic testing is becoming more common nowadays. It tests for a mutation in the RYR1 gene or any other gene involved in malignant hyperthermia.8Brandom B. W. (2006). Genetics of malignant hyperthermia. TheScientificWorldJournal, 6, 1722–1730. https://doi.org/10.1100/tsw.2006.289
Muscle Biopsy
Your doctor may perform a muscle biopsy to diagnose or assess malignant hyperthermia susceptibility.
Anesthetic Challenge Test
In an anesthetic challenge test, your doctor administers a small number of anesthetic gases to assess malignant hyperthermia response. However, this test is rarely performed.
Complete Blood Count (CBC)
Your doctor may advise a complete blood count (CBC) to check anemia, leukocytosis, or thrombocytopenia.
Serum Electrolytes
Your doctor may advise serum electrolytes to check hyperkalemia, hyperphosphatemia, or metabolic acidosis.
Creatinine Kinase (CK)
Your doctor may advise Creatinine Kinase levels to access muscle damage.
Lactate Dehydrogenase (LDH)
Lactate dehydrogenase (LDH) levels also help assess muscle damage.
Blood Gas Analysis
Arterial blood gas analysis (ABGs) are helpful in assessing metabolic acidosis or alkalosis.
Treatment Of Malignant Hyperthermia
The steps of management are:
Discontinue Triggering Gases:
The first step in treating this condition is discontinuing the triggering gases immediately and replacing them with alternate gases that are not harmful to the patient and do not cause malignant hyperthermia.
Hyperventilation:
The next step is hyperventilation to ensure maximum oxygen supply to the patient. Doctors use hundred percent oxygen to hyperventilate the patient. Moreover, a doctor must reduce the end-tidal carbon dioxide to a minimum value.
Call For Help:
A doctor must call senior anaesthesiologists along with a team of medical experts, including neurologists, trained nurses, intensivists, pharmacists and internists, to manage this condition and its complications. This interprofessional collaborative approach is helpful in improving patient outcomes.
Dantrolene:
In the next step, your doctor gives the patient intravenous dantrolene as soon as possible. The dose is 2.5 milligrams per kilogram, but the doctor may give it up to 10 milligrams per kilogram until the reaction subsides. The doctor continues it at the dose of 1 milligram per kilogram every four hours for the next 24 to 48 hours.9Ratto D, Joyner RW. Dantrolene. 2023 Apr 3. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan–. PMID: 30571019.

Cooling Measures:
The next step in the treatment is to follow cooling measures. The doctor gives you cold intravenous fluids and applies ice packs to reduce your body temperature.
Treatment Of Arrhythmias:
Your doctor will then treat arrhythmias. For this, the doctor prefers amiodarone and avoids calcium channel blockers, particularly verapamil, because they can cause hypotension and hyperkalemia.
Urine Output:
The doctors ensure adequate urine output by adding 3g of mannitol to each vial of dantrolene.
Correction Of Metabolic Abnormalities:
While treating this condition, your doctor must correct metabolic abnormalities like acidosis and hyperkalemia.
Repeat laboratory Investigations:
The doctors repeat laboratory investigations, such as arterial blood gas analysis (ABGs), serum electrolytes, particularly potassium, coagulation profile, and urine analysis, to detect myoglobin in the blood.10Frassanito, L., Fabio Sbaraglia, Piersanti, A., Vassalli, F., Lucente, M., Nicoletta Filetici, Bruno Antonio Zanfini, Stefano Catarci, & Gaetano Draisci. (2023). Real Evidence and Misconceptions about Malignant Hyperthermia in Children: A Narrative Review. Journal of Clinical Medicine, 12(12), 3869–3869. https://doi.org/10.3390/jcm12123869
Shifting Of Patient In Intensive Care Unit (ICU):
After stabilizing the patient, the doctors shift the patient to the intensive care unit (ICU) for monitoring for 24 hours because there is the risk of redundancy as well. The risk of redundancy is greater in patients who have greater muscle or are exposed to anesthetic gases for more than one hundred fifty minutes.
Complications Of Malignant Hyperthermia
It is an emergency condition that needs immediate management. It can lead to very severe complications that include:
Cardiac Arrest:
The heart undergoes arrhythmias during the attack of malignant hyperthermia. It can also lead to cardiac arrest in these patients.
Myocardial Infarction:
Myocardial infarction may occur due to increased workload and ischemia of heart muscles.
Rhabdomyolysis:
This condition damages the muscles of your body and can lead to rhabdomyolysis, in which muscle breakdown occurs in your body.
Acute kidney Injury:
The products of muscle breakdown affect your kidneys and lead to acute kidney injury and renal failure in severe cases. Moreover, ischemic changes also damage your kidneys.
Respiratory Complications:
Respiratory complications like respiratory depression, acute respiratory distress syndrome, and respiratory failure can occur in a patient with malignant hyperthermia.
Neurological Complications:
Neurological complications like seizures, stroke, and brain damage can occur.
Metabolic Problems:
Metabolic problems like acidosis, hyperkalemia, and hypocalcemia can occur.
Coagulation Problems:
Coagulation problems like disseminated intravascular coagulation (DIC) and thrombocytopenia can occur in malignant hyperthermia.
Such conditions can lead to multi-organ failure and even death.
Malignant Hyperthermia Vs. Neuroleptic Malignant Syndrome:
| Malignant Hyperthermia | Neuroleptic Malignant Syndrome | |
| Definition
Symptoms |
Malignant hyperthermia is a condition of muscle rigidity, hypermetabolism, cardiovascular compromise, and respiratory problems due to the effect of volatile anesthetic gases.
Its symptoms include hyperthermia, muscle rigidity, tachycardia, tachypnea, hypertension, arrhythmias, and acidosis. |
Neuroleptic malignant syndrome is a condition that occurs in response to antipsychotic medicines. Its symptoms include fever, rigidity, altered level of consciousness, and cardiovascular and respiratory problems.
Symptoms of neuroleptic malignant syndrome include:
|
| Cause And Pathophysiology | It occurs due to volatile anesthetic gases like isoflurane, halothane, sevoflurane, and desflurane, which cause abnormal calcium release in the sarcoplasmic reticulum of skeletal muscles. | It occurs due to antipsychotic drugs like haloperidol and risperidone that cause dopamine blockage and imbalance of neurotransmitters in your brain as a result. |
| Muscle Damage
Temperature |
Muscle damage is severe in this condition.
Your body temperature can reach up to 109 Fahrenheit in malignant hyperthermia. |
Muscle damage is less severe in neuroleptic malignant syndrome as compared to malignant hyperthermia.
Your body temperature ranges from 103 Fahrenheit to 106 Fahrenheit in neuroleptic malignant syndrome. |
Prognosis Of Malignant Hyperthermia
This condition needs immediate management. Complete recovery is possible if your doctor recognizes it early and starts the treatment immediately. However, delay in treatment can lead to multi-organ failure and even death. However, in some cases, deaths occur despite early detection and treatment. Its mortality rate is less than 5 percent.11Rosenberg, H., Davis, M., James, D., Pollock, N., & Stowell, K. (2007). Malignant hyperthermia. Orphanet journal of rare diseases, 2, 21. https://doi.org/10.1186/1750-1172-2-21
Is Malignant Hyperthermia A Genetic Condition?
Yes, It is a genetic disorder with an autosomal dominant pattern of inheritance. It is associated with a mutation in the RYR1 gene. If you have a family history, you are at risk of developing it.
Can Malignant Hyperthermia Occur Outside The Operation Theater?
Yes, It can also occur outside the operation theatre. Though it occurs mostly in the operation theatre due to anesthetic gases, it can occur outside the operation theatre as well if you are getting muscle relaxants for other medical procedures.
Which Anaesthetic Drugs Are Safe For The Patient With Previous History Of Malignant Hyperthermia?
For patients having a history of malignant hyperthermia, doctors prefer other anesthetic gases like non-halogens anesthetic gases, propofol, opioids (morphine, codeine), benzodiazepines (diazepam, midazolam), etomidate (an intravenous anesthetic), nitrous oxide and local anesthetics like xylocaine, bupivacaine.
Moreover, doctors use non-depolarizing muscle relaxants like rocuronium, atracurium, and vecuronium, as well as gallamine.
Conclusion:
This is a life-threatening complication of anesthesia with volatile anesthetic gases. Its symptoms include muscle stiffness, hyperthermia, respiratory depression, hypertension, arrhythmias, tachypnea, and tachycardia. Treatment involves dantrolene, hyperventilation, cooling the patient, correction of compilations, and monitoring in the intensive care unit (ICU). If your doctor recognizes it and starts treatment immediately, it has a good prognosis.
Refrences
- 1Rosenberg, H., Pollock, N., Schiemann, A., Bulger, T., & Stowell, K. (2015). Malignant hyperthermia: a review. Orphanet journal of rare diseases, 10, 93. https://doi.org/10.1186/s13023-015-0310-1
- 2Brady, J. E., Sun, L. S., Rosenberg, H., & Li, G. (2009). Prevalence of this condition due to anesthesia in New York State, 2001-2005. Anesthesia and analgesia, 109(4), 1162–1166. https://doi.org/10.1213/ane.0b013e3181ac1548
- 3Hopkins, P. M., Gupta, P. K., & Bilmen, J. G. (2018). Malignant hyperthermia. Handbook of clinical neurology, 157, 645–661. https://doi.org/10.1016/B978-0-444-64074-1.00038-0
- 4Michelucci, A., Paolini, C., Boncompagni, S., Canato, M., Reggiani, C., & Protasi, F. (2017). Strenuous exercise triggers a life-threatening response in mice susceptible to malignant hyperthermia. FASEB journal: official publication of the Federation of American Societies for Experimental Biology, 31(8), 3649–3662. https://doi.org/10.1096/fj.201601292R
- 5Nelson T. E. (2001). Heat production during anesthetic-induced malignant hyperthermia. Bioscience Reports, 21(2), 169–179. https://doi.org/10.1023/a:1013696124358
- 6Larach MG, Brandom BW, Allen GC, Gronert GA, Lehman EB. Malignant hyperthermia deaths related to inadequate temperature monitoring, 2007-2012: a report from the North American malignant hyperthermia registry of the malignant hyperthermia association of the United States. Anesth Analg. 2014 Dec;119(6):1359-66. doi: 10.1213/ANE.0000000000000421. PMID: 25268394.
- 7Larach, M. G., Landis, J. R., Bunn, J. S., & Diaz, M. (1992). Prediction of malignant hyperthermia susceptibility in low-risk subjects. An epidemiologic investigation of caffeine halothane contracture responses. The North American Malignant Hyperthermia Registry. Anesthesiology, 76(1), 16–27. https://doi.org/10.1097/00000542-199201000-00003
- 8Brandom B. W. (2006). Genetics of malignant hyperthermia. TheScientificWorldJournal, 6, 1722–1730. https://doi.org/10.1100/tsw.2006.289
- 9Ratto D, Joyner RW. Dantrolene. 2023 Apr 3. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan–. PMID: 30571019.
- 10Frassanito, L., Fabio Sbaraglia, Piersanti, A., Vassalli, F., Lucente, M., Nicoletta Filetici, Bruno Antonio Zanfini, Stefano Catarci, & Gaetano Draisci. (2023). Real Evidence and Misconceptions about Malignant Hyperthermia in Children: A Narrative Review. Journal of Clinical Medicine, 12(12), 3869–3869. https://doi.org/10.3390/jcm12123869
- 11Rosenberg, H., Davis, M., James, D., Pollock, N., & Stowell, K. (2007). Malignant hyperthermia. Orphanet journal of rare diseases, 2, 21. https://doi.org/10.1186/1750-1172-2-21

