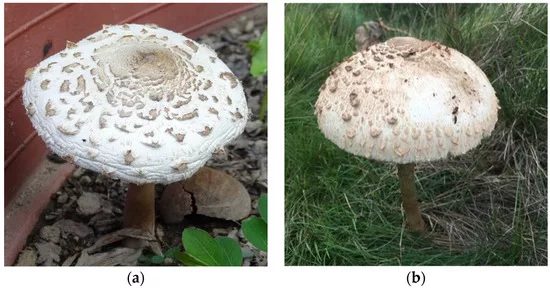
Mushroom poisoning refers to the toxic and sometimes fatal effects that result from ingesting mushrooms containing harmful substances. This condition typically arises when individuals consume wild mushrooms after mistakenly identifying a toxic species as edible, often due to the close resemblance in shape and color between poisonous and non-poisonous varieties. Mushrooms are the fruiting bodies of higher fungi, widely distributed across the world, and comprise thousands of species. Of these, around 100 species are known to be poisonous when eaten, and approximately 15 to 20 are potentially lethal upon ingestion.1Hendrickson, R.G. Mushroom Toxicity. 2023; Available from: https://emedicine.medscape.com/article/167398-overview.
There are an estimated 6000 ingestions of poisonous mushrooms in the United States, and over half of the exposures typically occur in children under the age of six.2Tran, H.H. and A.L. Juergens, Mushroom toxicity, in StatPearls [Internet]. 2023, StatPearls Publishing.
The severity of mushroom poisoning can vary significantly depending on several factors, including geographic location, environmental growth conditions, genetic characteristics of the mushroom, and the amount of toxin consumed. Notably, the toxicity of certain mushroom species remains unaffected by boiling, cooking, processing, or freezing.
Types of Mushroom Poisoning
Researchers classify mushroom poisoning based on the time of symptom onset, its clinical effects, and the affected organs. The major types of this condition are:
Types of Mushroom Poisoning According to the Symptom Onset:
Early-Onset
Symptoms of early-onset appear almost immediately, within six hours of ingestion, and most of the non-life-threatening cases fall into this category. Common presentations include allergic reactions, neurologic symptoms (e.g., confusion, dizziness), and gastrointestinal syndromes such as nausea, vomiting, and diarrhea.
Late-onset
Symptoms develop after more than six hours of ingestion. This type is typically associated with hepatotoxicity or nephrotoxicity, particularly due to amatoxins or orellanine.3White, J., et al., Mushroom poisoning: A proposed new clinical classification. Toxicon, 2019. 157: p. 53-65.
Delayed-Onset
Symptoms of this type arise more than 24 hours after ingestion. This is often linked to nephrotoxic mushrooms and may result in severe kidney damage (e.g., orellanine-induced nephropathy).4White, J., et al., Mushroom poisoning: A proposed new clinical classification. Toxicon, 2019. 157: p. 53-65.
Types based on Clinical Syndrome & Toxin Type:
A recent clinical classification proposes six major groups of mushroom poisoning based on the primary toxic component and the organ systems involved.5White, J., New classification of mushroom poisoning. Toxicologie Analytique et Clinique, 2018. 30(3): p. 157-158 The details about these six groups are given in the table:
| Group 1 | Symptom Type | Main toxins | Clinical Features | Example Mushrooms |
| 1 | Cytotoxic | Gyromitrin
Orellanine Amatoxins | Gyromitra esculenta, Cortinarius orellanus, Amanita phalloides | Gyromitra esculenta, Cortinarius orellanus, Amanita phalloids |
| 2 | Myotoxic | Myotoxins | Muscle breakdown | Tricholoma equestre, Russula spp. |
| 3 | Neurotoxic | Muscimol, ibotenic acid, psilocybin,
Psilocybin | Central nervous system effects, autonomic dysfunction, and hallucinations | Amanita muscaria, Psilocybe spp., Clitocybe spp. |
| 4 | Gastrointestinal irritants | Various low-molecular-weight compounds | Diarrhea, nausea
Vomiting without any major organ damage | Entoloma spp. Chlorophyllum molybdites |
| 5 | Endocrine or Metabolic | Polyporic acid
Coprine, Gyromitrin | Metabolic disturbances such as disulfiram-like reaction, hypoglycemia, etc. | Coprinus atramentarius, Podostroma spp., Gyromitra spp. |
| 6 | Miscellaneous | Various | Some unusual reactions, such as pancytopenia and dermatitis | Pleurocybella porrigens, paxillus involutus,
Shiitake |
Etiology of Mushroom Poisoning
The main causes of the mushroom poisoning include:
- Unintentional ingestion by a child while playing outdoors.
- Incorrect identification of a mushroom. The primary cause is the accidental ingestion of wild mushrooms. Many species are similar enough in appearance to confuse an insufficiently informed or inexperienced mushroom hunter.
- Intentional ingestion by a person with substance abuse.
- Inhalation of volatile compounds (rare), especially from Gyromitra species while cooking, which can release toxic hydrazines.
Symptoms of Mushroom Poisoning
Symptoms range from mild gastrointestinal upset to severe organ failure and death. The common symptoms include:
- Gastrointestinal Irritation: This can include nausea, vomiting, diarrhea, and abdominal pain.
- Dehydration: Severe nausea and vomiting can lead to dehydration, especially in children.
Severe & Delayed Effects:
- Organ Failure: Delayed symptoms include liver failure (amatoxins) or kidney failure (orellanine).
- Muscle Breakdown: Rhabdomyolysis can be fatal. It can occur with certain Tricholoma species and may lead to acute kidney injury.
- Neurologic Effects: Confusion, seizures, and hallucinations.
Diagnosis of Mushroom Poisoning
Diagnosing the condition involves a combination of clinical evaluation, taking a thorough medical history, and performing laboratory tests.
Clinical History:
History-taking is critical, as the timing and pattern of symptoms often provide key diagnostic clues. Symptom onset within six hours usually indicates a less severe form, typically involving gastrointestinal irritants. A well-documented symptom history can help narrow down the potential toxin involved. It’s also essential to gather details about where, when, and how the mushrooms were collected, stored, and prepared.
Important history components to relay to local poison control centers include:
- How much was eaten?
- Time to symptom onset after ingestion?
- Description of the mushroom, such as the color, cap appearance, and texture of the ingested mushrooms?
- Season and geographic location of collection?
- Are there any additional individuals who have consumed the same mushrooms?
Laboratory Tests:
The doctors access a basic serum metabolic profile to evaluate fluid and electrolyte imbalances in patients with severe vomiting and diarrhea. Baseline kidney function tests, including blood urea nitrogen concentrations, urinalysis, and creatinine levels, are used for screening renal function. Liver function tests (AST, ALT, bilirubin) are indicated, especially if hepatotoxic mushrooms like Amanita phalloides are suspected. Additionally, the doctor may also order a Coagulation profile (useful for monitoring hepatic synthetic function) and a Complete blood count (to detect cytopenias or infection).
Toxin-Specific Tests
The enzyme-linked immunosorbent assay (ELISA) is the most sensitive and technically simple test for detecting amatoxins in urine. It is reliable within 36 hours of mushroom ingestion. Amatoxins typically become undetectable in blood or urine after four days.6Tuğcan, M.O. and A.A. Akpınar, Mushroom poisoning: An updated review. Turkish Journal of Emergency Medicine, 2025. 25(1): p. 10-16.
Liquid chromatography-mass spectrometry (LC-MS) also helps in determining the presence of the main active substances.7Wennig, R., et al., Mushroom poisoning. Deutsches Ärzteblatt International, 2020. 117(42): p. 701.
The less commonly used tests include polymerase chain reaction (PCR), lateral flow immunoassay, and radioimmunoassay.
Treatment of Mushroom Poisoning
Effective management requires rapid decontamination, antidotes, and supportive care. Treatment strategies depend on the severity of the symptoms and toxins involved.
Decontamination:
Activated charcoal administered at 0.5-1 g/kg (max 50 g) reduces toxin absorption and interrupts the enterohepatic circulation of the amatoxins, especially within six hours of ingestion.
Gastric lavage is considered only if ingestion occurs within one to two hours.
Antidotes & Specific Therapies:
The toxin type and related antidote therapy are listed in the table:
| Toxin Type | Antidote/ Therapy and Key Considerations |
| Amatoxins |
|
| Gyromitrin | IV pyridoxine (vitamin B6) at 70 mg/kg for seizure control.. |
| Muscarine | To counteract the cholinergic symptoms, such as bronchorrhea or bradycardia, doctors recommend IV atropine 0.02 mg/kg. |
| Orellanine | Kidney transplantation for end-stage cases and hemodialysis for delayed renal failure. |
| Coprine | Supportive care for disulfiram-like reactions. If you are an alcohol addict, then avoid alcohol for 3 to 5 days after ingestion of this toxin.10Haberl, B., et al., Case series: Alcohol intolerance with Coprine-like syndrome after consumption of the mushroom Lepiota aspera (Pers.: Fr.) Quél., 1886 (Freckled Dapperling). Clinical Toxicology, 2011. 49(2): p. 113-114. |
Supportive Care:
Supportive care includes:
- Addressing dehydration with IV crystalloids.
- Use ondansetron for symptom control, such as vomiting and nausea.
- Use benzodiazepines for symptom control, such as hallucinations or agitation.
- For liver support (such as hepatic encephalopathy), the healthcare provider administers vitamin K, lactulose, and fresh frozen plasma.
Advanced Therapies:
The advanced therapies for mushroom poisoning include:
- Hemodialysis has limited utility for amatoxins, but can also be effective for orellanine-induced renal failure.
- Plasmapheresis removes circulating toxins and supports hepatocyte regeneration. It is generally recommended in case of severe phalloids.
- Liver transplantation is indicated for fulminant hepatic failure.
Differential Diagnosis
Differential diagnosis of mushroom toxicity includes:
- Foodborne toxin
- Ischemic hepatitis
- Acute viral hepatitis
- Alcoholic hepatitis
- Gastroenteritis
- Acetaminophen toxicity
- Carbamate toxicity
- Organophosphate toxicity
- Isoniazid toxicity
Prognosis
Most symptoms of mushroom ingestion recover without complications after receiving adequate supportive care. However, patients with Cortinarius ingestion had evidence of renal impairment and end-stage renal failure and ultimately received kidney transplantation. Most people with Gyromitra ingestion recover within one week with the initiation of prompt seizure management with supportive care. Patients with hepatotoxicity usually recover, while 2% of patients with Amanita toxicity ultimately require liver transplantation.11Tran, H.H. and A.L. Juergens, Mushroom toxicity, in StatPearls [Internet]. 2023, StatPearls Publishing.
Final Remarks
Mushroom poisoning has a broad range of manifestations that depend on the type of mushroom ingested by the individual. Most poisonings can result in mild to moderate gastrointestinal manifestations, but there is a variety of sequelae that can lead to organ failure and even mortality. Hence, foragers (particularly those who are new to this field) must know about the variety of differing mushroom species and potential look-alikes. Knowledge of toxic and local edible mushroom species is essential for professional foragers. After mushroom consumption, even mild nausea should require evaluation as it can be the initial clinical manifestation of a severe illness, and with early diagnosis and immediate treatment, severe damage can be prevented. The condition requires an interprofessional approach to care for the patient.
Refrences
- 1Hendrickson, R.G. Mushroom Toxicity. 2023; Available from: https://emedicine.medscape.com/article/167398-overview.
- 2Tran, H.H. and A.L. Juergens, Mushroom toxicity, in StatPearls [Internet]. 2023, StatPearls Publishing.
- 3White, J., et al., Mushroom poisoning: A proposed new clinical classification. Toxicon, 2019. 157: p. 53-65.
- 4White, J., et al., Mushroom poisoning: A proposed new clinical classification. Toxicon, 2019. 157: p. 53-65.
- 5White, J., New classification of mushroom poisoning. Toxicologie Analytique et Clinique, 2018. 30(3): p. 157-158
- 6Tuğcan, M.O. and A.A. Akpınar, Mushroom poisoning: An updated review. Turkish Journal of Emergency Medicine, 2025. 25(1): p. 10-16.
- 7Wennig, R., et al., Mushroom poisoning. Deutsches Ärzteblatt International, 2020. 117(42): p. 701.
- 8Ye, Y. and Z. Liu, Management of Amanita phalloides poisoning: A literature review and update. Journal of Critical Care, 2018. 46: p. 17-22.
- 9Tuğcan, M.O. and A.A. Akpınar, Mushroom poisoning: An updated review. Turkish Journal of Emergency Medicine, 2025. 25(1): p. 10-16.
- 10Haberl, B., et al., Case series: Alcohol intolerance with Coprine-like syndrome after consumption of the mushroom Lepiota aspera (Pers.: Fr.) Quél., 1886 (Freckled Dapperling). Clinical Toxicology, 2011. 49(2): p. 113-114.
- 11Tran, H.H. and A.L. Juergens, Mushroom toxicity, in StatPearls [Internet]. 2023, StatPearls Publishing.

