Ovarian Fibroma is a prevalent benign tumor found in the ovary, accounting for approximately 1% to 4% of non-cancerous ovarian tumors. These tumors vary in size, ranging from small growths to larger tumors measuring up to 14 cm. While commonly observed in perimenopausal or postmenopausal women, ovarian fibromas can occur in females after puberty, although childhood cases are exceedingly rare.
In most cases, ovarian fibromas do not cause symptoms until they grow large enough to exert pressure on nearby organs, such as the bladder. Large fibromas cause abdominal pain, frequent urination, and fluid accumulation in the abdomen (ascites).
Ovarian fibroma can be tricky to diagnose before surgery and is sometimes confused with uterine myomas due to how it looks on ultrasound. The primary treatment for ovarian fibroma typically involves surgical removal.
Ovarian Fibroma- What Is It?
Ovarian fibroma is a non-cancerous growth in the ovary. It is a benign tumor and typically consists of fibrous connective tissue. The size of ovarian fibroma varies from 1.2 to 14cm1Parwate, N. S., Patel, S. M., Arora, R., & Gupta, M. (2016). Ovarian Fibroma: A Clinico-pathological Study of 23 Cases with Review of Literature. Journal of obstetrics and gynecology of India, 66(6), 460–465. https://doi.org/10.1007/s13224-015-0717-6. Small fibromas are often asymptomatic and do not cause any problems. However, a large fibroma can cause severe abdominal pain in women, making day-to-day activities difficult. Large fibromas also require surgical removal and medical therapy. They usually happen around menopause, with the average age being about 52 years2Singh, S., Sahu, P., Selvan, A. T., & Naik, S. (2022). Diagnostic Dilemma: Parasitic Ovarian Fibroma With Degeneration. Cureus, 14(12), e32739. https://doi.org/10.7759/cureus.32739.
Ovarian Fibroma Causes – Why Does It Happen?
Most of the ovarian fibroma cases are benign with no known cause. However, here are some risk factors that can cause ovarian benign growths in women:
Genetic Factors
Different genetic mutations cause ovarian fibroma. Researchers have identified PTCH1 and SMARCA4 gene mutations in ovarian fibroma patients3Higashimoto, T., Smith, C. H., Hopkins, M. R., Gross, J., Xing, D., Lee, J. W., Morris, T., & Bodurtha, J. (2022). Case report of bilateral ovarian fibromas associated with de novo germline variants in PTCH1 and SMARCA4. Molecular genetics & genomic medicine, 10(9), e2005. https://doi.org/10.1002/mgg3.2005. Although genetic changes are present, ovarian fibromas are rarely present before puberty.
Hormonal Changes
Changes in hormone levels, particularly estrogen, can contribute to the formation of ovarian fibromas. Since there’s a decline in estrogen production in perimenopause and menopausal women, ovarian fibroma starts growing.
Age
Age is a major risk factor for ovarian fibromas. Studies have identified that these benign growths are more common in women during their reproductive years and menopausal period4Reitere, D., Mašinska, M., Līdaka, L., Franckeviča, I., Baurovska, I., & Apine, I. (2021). Bilateral ovarian fibromas in a 15-year-old primary amenorrhea patient: a case report. Radiology case reports, 17(2), 368–372. https://doi.org/10.1016/j.radcr.2021.11.002.
Endometriosis
Endometriosis and ovarian fibromas usually coexist, and the two may be correlated. The former means the growth of the lining of the uterus outside it.
Radiation Exposure
As for many other diseases as well, prolonged radiation exposure is a potential risk factor for developing ovarian fibromas.
Ovarian Fibroma Pathology- How Does It Happen?
Ovarian fibroma is classified as a sex cord/stromal tumor. It typically originates in the ovary; its primary component is fibrous connective tissue. Ovarian fibromas are often solid masses with a firm consistency.
The exact pathophysiology of ovarian fibromas is not fully understood, but they are thought to arise from the ovarian stromal cells. These are the supportive tissue cells of the ovary. In ovarian fibroma patients, there is an abnormal proliferation of fibrous connective tissue within the ovary. Hormonal factors may influence this excessive growth, as ovarian stromal cells are responsive to hormones like estrogen. Genetic factors may also play a role. Ovarian fibromas can be linked to genetic syndromes like Gorlin syndrome or basal cell nevus syndrome. They may also associate with luteinized thecomas, tumors of the ovarian stroma.
How Does Ovarian Fibroma Look Like?
The features of ovarian fibroma are described below:
Gross Appearance
Ovarian fibroma is a solid, round, or oval-shaped mass within the ovary. It has well-defined borders and has a smooth surface. The size of ovarian fibromas can vary, ranging from small nodules to larger growths.
Sometimes, there can be areas with comatose features (fibrosarcoma). In certain cases, having an ovarian fibroma can lead to ovarian torsion.
Imaging techniques such as ultrasound or MRI are often used to visualize and assess the gross morphology of ovarian fibromas.

Case courtesy of Andrew Dixon, Radiopaedia.org. From the case rID: 9583
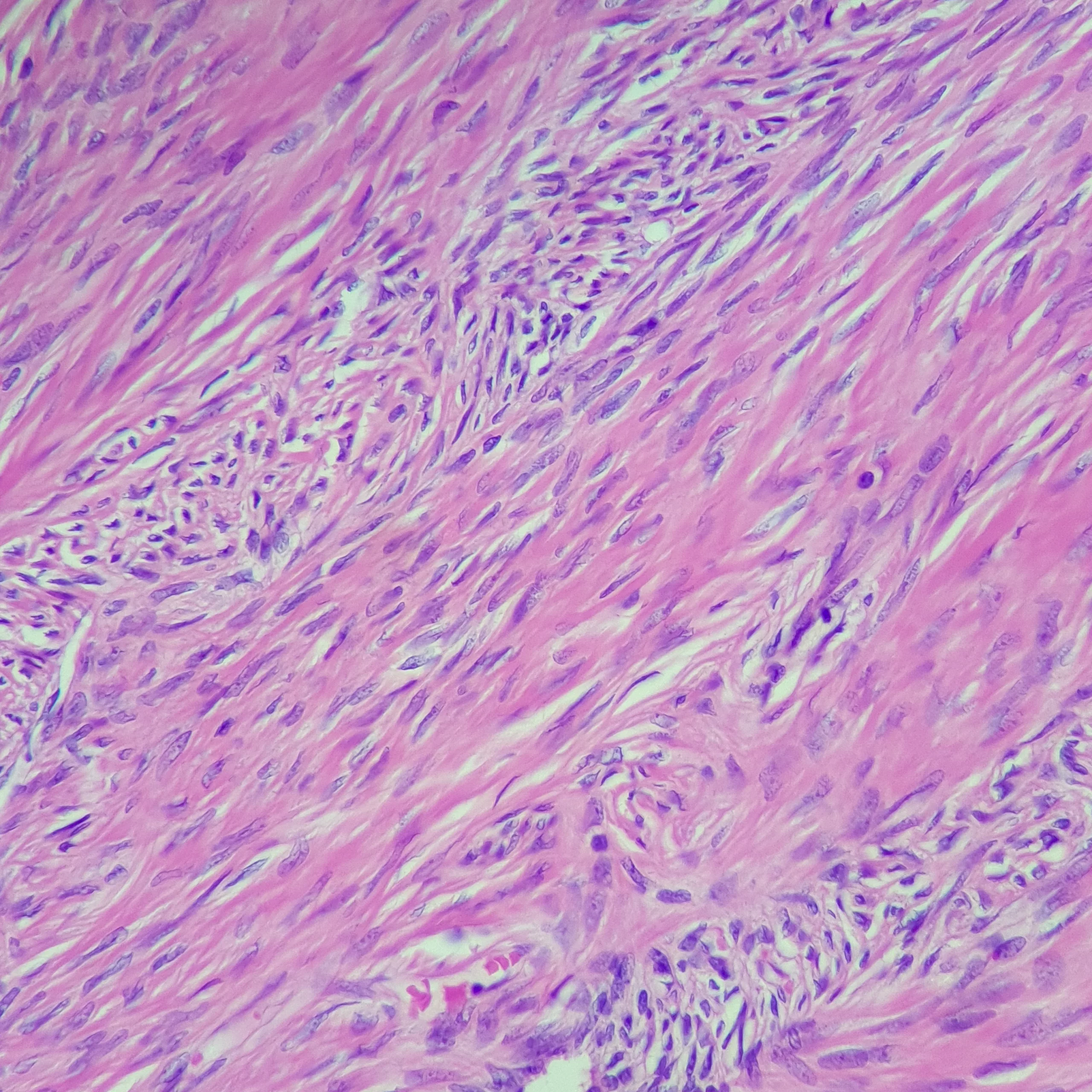
Microscopic Appearance
Ovarian fibromas are characterized by spindle-shaped cells arranged in a pattern resembling fibrous tissue. The cells produce collagen, a protein that forms the structural framework of various tissues in the body. This excessive collagen production contributes to the firmness of the tumor.
Ovarian Fibroma – Symptoms
The majority of ovarian fibromas do not cause any symptoms. They keep growing silently until detected on a gynecological examination.
Large ovarian fibromas can cause abdominal pain, mainly if the fibroma twists or turns the ovaries. Other less common signs include:
- Irregular periods or bleeding after menopause.
- Peritonitis and shock if a cyst breaks open.
- Enlarged abdomen.
- Fluid in the abdomen (ascites).
- Feeling like you need to pee frequently.
- A constant pressure on the bladder.
- Pain during or after sexual intercourse.
- Irregularities in the menstrual cycle.
Diagnosing Ovarian Fibroma
Doctors typically diagnose ovarian fibroma by reviewing medical history, conducting physical exams, using imaging tests, and occasionally performing biopsies. The diagnostic process may include:
Medical History:
Your doctor will inquire about your symptoms, medical history, and any relevant family history of ovarian or other reproductive tract conditions.
Physical Examination:
A pelvic examination may be performed to check for any palpable masses or abnormalities in the pelvic region.
Imaging studies:
Radiology is the standard intervention for diagnosing ovarian fibromas.5Borukh, E., Ilyaev, B., Muminiy, S. N., Babayev, M., Musheyev, Y., & Levada, M. (2023). Ovarian Fibroma Presents As Uterine Leiomyoma in a 61-Year-Old Female: A Case Study. Cureus, 15(3), e36264. https://doi.org/10.7759/cureus.36264 Radiographic features refer to how things appear in medical imaging. Doctors use ultrasound, MRI, and CT scans to view ovarian fibromas.
Ultrasound
When using ultrasound, fibromas typically appear as solid masses with lower echoes. Hypoechoic or lower echo appearance means the structure being viewed is less dense. Ovarian fibroma might look like a certain type of uterine fibroid on ultrasound.
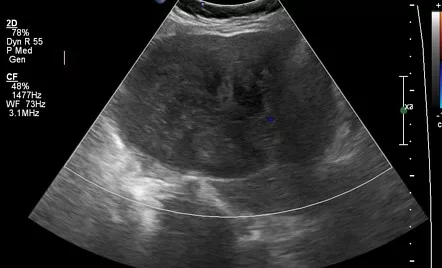
Case courtesy of Hala Maher, Radiopaedia.org. From the case rID: 90376
CT Scan
CT scans show fibromas as slightly dark masses with slow contrast enhancement. Calcifications (hardenings) are not very common in these tumors.
MRI Scan
MRI scans display well-defined masses with low signal intensity. Some areas might look brighter due to swelling or fluid. During dynamic contrast-enhanced MRI, fibromas don’t light up as much as the normal parts of the uterus or fibroids.
Ovarian Fibroma Treatment
Almost all ovarian fibromas are benign, and the primary treatment for ovarian fibromas is surgical removal.6Son, C. E., Choi, J. S., Lee, J. H., Jeon, S. W., Hong, J. H., & Bae, J. W. (2011). Laparoscopic surgical management and clinical characteristics of ovarian fibromas. JSLS: Journal of the Society of Laparoendoscopic Surgeons, 15(1), 16–20. https://doi.org/10.4293/108680810X12924466009087
The specific type of surgical procedure depends on factors such as the size of the tumor, its characteristics, and whether there are any associated complications.
Here are the main treatment options:
Oophorectomy
It is a Greek term that means “removing the ovary.” This procedure removes the affected ovary.
Oophorectomy is usually indicated in postmenopausal women in which preservation of fertility is not a primary concern.7Najmi, Z., Mehdizadehkashi, A., Kadivar, M., Tamannaie, Z., & Chaichian, S. (2014). Laparoscopic approach to a large ovarian fibroma: a case report. Journal of reproduction & infertility, 15(1), 57–60.
Ovarian Cystectomy
This surgical approach only removes the fibrous growth and preserves the ovary. It is done in young women of reproductive age. Ovarian Cystectomy is indicated when the fibroma is small, and preserving fertility is a priority.
Hysterectomy
Hysterectomy means the “removal of the uterus.” Sometimes, there is a torsion of ovarian fibroma, meaning the fibroma gets twisted around the ovarian ligaments. This condition requires total or partial hysterectomy8Erekson, E. A., Martin, D. K., & Ratner, E. S. (2013). Oophorectomy: the debate between ovarian conservation and elective oophorectomy. Menopause (New York, N.Y.), 20(1), 110–114. https://doi.org/10.1097/gme.0b013e31825a27ab.
It is also done in the case of multiple ovarian fibromas in postmenopausal women.
Laparoscopic Surgery
It is a minimally invasive surgery using small incisions and a camera for guidance.
It is appropriate for smaller fibromas and may result in faster recovery than traditional open surgery. However, surgeons are hesitant towards this approach because it is difficult to take out the cancerous growth safely.
Exploratory Laparotomy
It is the traditional open surgery with an abdominal incision. This is not a good approach due to the risks of severe infection. However, this extensive procedure may be required in complicated cases and extremely large fibromas.
Ovarian Fibroma Prognosis
Almost all cases of ovarian fibroma can be completely treated with surgical removal, so the condition has a good prognosis. The recurrence rate of these benign growths is also very low.
Ovarian Fibroma Vs. Ovarian Cancer
Ovarian fibroma and ovarian cancer are two distinct conditions affecting the ovaries. The former is a benign tumor, meaning it is non-cancerous. These tumors typically consist of fibrous connective tissue and are not considered life-threatening.
On the other hand, ovarian cancer is a malignant condition in which there is an abnormal and uncontrolled growth of cells in the ovaries. Unlike ovarian fibromas, ovarian cancer poses a serious health risk. The cancerous cells can invade nearby tissues and, in advanced stages, spread to other organs. Ovarian fibromas may cause symptoms like abdominal or pelvic pain. However, they do not cause vaginal bleeding. On the other side, ovarian cancer typically causes extensive vaginal bleeding and unintentional weight loss. Early detection of ovarian cancer is important for effective treatment, as symptoms may not be noticeable in the initial stages.
What is Meigs’ Syndrome?
Meigs’ syndrome is a rare but significant condition associated with ovarian fibromas. It is characterized by the triad of an ovarian fibroma (or fibroma-like tumor), ascites (the accumulation of fluid in the abdomen), and pleural effusion (the accumulation of fluid in the pleural cavity around the lungs). Despite its alarming presentation, Meigs’ syndrome is benign and resolves once the ovarian tumor is surgically removed. The exact mechanism behind the fluid accumulation is not fully understood, but it is thought to be related to the inflammatory response and pressure effects of the tumor. Recognizing Meigs’ syndrome is crucial for distinguishing it from more malignant conditions and for ensuring appropriate surgical treatment.
In conclusion, ovarian fibromas are prevalent benign tumors of the ovary that can present diagnostic challenges. Despite their benign nature, prompt diagnosis and appropriate management are crucial. Surgical removal remains the mainstay of treatment, and ongoing research aims to improve diagnostic accuracy and therapeutic outcomes for affected individuals.
Refrences
- 1Parwate, N. S., Patel, S. M., Arora, R., & Gupta, M. (2016). Ovarian Fibroma: A Clinico-pathological Study of 23 Cases with Review of Literature. Journal of obstetrics and gynecology of India, 66(6), 460–465. https://doi.org/10.1007/s13224-015-0717-6
- 2Singh, S., Sahu, P., Selvan, A. T., & Naik, S. (2022). Diagnostic Dilemma: Parasitic Ovarian Fibroma With Degeneration. Cureus, 14(12), e32739. https://doi.org/10.7759/cureus.32739
- 3Higashimoto, T., Smith, C. H., Hopkins, M. R., Gross, J., Xing, D., Lee, J. W., Morris, T., & Bodurtha, J. (2022). Case report of bilateral ovarian fibromas associated with de novo germline variants in PTCH1 and SMARCA4. Molecular genetics & genomic medicine, 10(9), e2005. https://doi.org/10.1002/mgg3.2005
- 4Reitere, D., Mašinska, M., Līdaka, L., Franckeviča, I., Baurovska, I., & Apine, I. (2021). Bilateral ovarian fibromas in a 15-year-old primary amenorrhea patient: a case report. Radiology case reports, 17(2), 368–372. https://doi.org/10.1016/j.radcr.2021.11.002
- 5Borukh, E., Ilyaev, B., Muminiy, S. N., Babayev, M., Musheyev, Y., & Levada, M. (2023). Ovarian Fibroma Presents As Uterine Leiomyoma in a 61-Year-Old Female: A Case Study. Cureus, 15(3), e36264. https://doi.org/10.7759/cureus.36264
- 6Son, C. E., Choi, J. S., Lee, J. H., Jeon, S. W., Hong, J. H., & Bae, J. W. (2011). Laparoscopic surgical management and clinical characteristics of ovarian fibromas. JSLS: Journal of the Society of Laparoendoscopic Surgeons, 15(1), 16–20. https://doi.org/10.4293/108680810X12924466009087
- 7Najmi, Z., Mehdizadehkashi, A., Kadivar, M., Tamannaie, Z., & Chaichian, S. (2014). Laparoscopic approach to a large ovarian fibroma: a case report. Journal of reproduction & infertility, 15(1), 57–60.
- 8Erekson, E. A., Martin, D. K., & Ratner, E. S. (2013). Oophorectomy: the debate between ovarian conservation and elective oophorectomy. Menopause (New York, N.Y.), 20(1), 110–114. https://doi.org/10.1097/gme.0b013e31825a27ab

