Paroxysmal atrial fibrillation (PAF) is a type of atrial fibrillation (A-fib), which is an irregular and often rapid heart rhythm originating in the atria of the heart. PAF is characterized by sudden, intermittent episodes of irregular heartbeats that start and stop spontaneously. These episodes typically last less than seven days, with most resolving within 24 hours without medical intervention.1National Heart, Lung, and Blood Institute. (n.d.). *Types of Atrial Fibrillation*. Retrieved from [https://www.nhlbi.nih.gov/health/atrial-fibrillation/types]
Unlike persistent or permanent atrial fibrillation, PAF does not require continuous treatment to terminate the arrhythmia, although it may still necessitate management to prevent recurrence or complications. PAF often occurs without an apparent trigger, but factors like stress, alcohol consumption, dehydration, or underlying heart conditions may increase the likelihood of an episode. The overall prevalence is estimated to range from 2% to 4% in the general population and tends to rise with advancing age. However, the actual prevalence remains uncertain due to under-detection.2Brieger D, Amerena J, Attia J, et al., NHFA CSANZ Atrial Fibrillation Guideline Working Group. National Heart Foundation of Australia and the Cardiac Society of Australia and New Zealand: Australian clinical guidelines for the diagnosis and management of atrial fibrillation 2018. Heart Lung Circ2018;27:1209-66. doi:10.1016/j.hlc.2018.06.1043 pmid:30077228
Causes of Paroxysmal Atrial Fibrillation
Some factors that can increase the chances of developing health issues like Paroxysmal Atrial fibrillation are:
- A-fib may occur during illness or surgery.
- Problems with the heart or heart valves, such as Congestive heart failure (when the heart doesn’t pump blood properly), cardiomyopathy (when the heart muscle is weak), and pericarditis (when the area around the heart gets inflamed).
- Low levels of potassium or magnesium lead to paroxysmal atrial fibrillation. These minerals affect muscle contraction. Dietary deficiency of these minerals can put you at risk of A-fib.
- People present with Paroxysmal Atrial Fibrillation after binge drinking (consuming excessive alcohol in a short time). A-fib from binge drinking after holidays is known as “holiday heart syndrome.”
- Certain substances make A-fib more likely. These include methylphenidate, pseudoephedrine, cocaine, nicotine (found in tobacco), and caffeine (found in coffee and energy drinks).
- Increased thyroid hormone levels (hyperthyroidism) may also lead to A-fib.
- Having a family history of atrial fibrillation.
- Being overweight or obese.
It is important to note that whatever the cause, A-Fib can coexist with other heart comorbidities such as heart failure. This is because they share common risk factors. Both of them together have been associated with increased mortality.
How does Paroxysmal Atrial Fibrillation Present?
When someone has atrial fibrillation (AF), their symptoms can vary widely. AF may be discovered incidentally during an electrocardiogram (ECG) without causing noticeable symptoms. However, AF can also have more severe consequences, such as an undiagnosed irregular rhythm leading to a stroke.
The most common symptoms of AF are similar to other arrhythmias and may include:3Ludhwani D, Wieters JS. Paroxysmal Atrial Fibrillation [Internet]. PubMed. Treasure Island (FL): StatPearls Publishing; 2020. Available from: https://www.ncbi.nlm.nih.gov/books/NBK535439/
- Palpitations: You may feel a rapid, irregular, or fluttering heartbeat.
- Dyspnea: You may feel shortness of breath (both at rest and during exertion).4van der Velden RMJ, Hermans ANL, Pluymaekers NAHA, Gawalko M, Elliott A, Hendriks JM, Franssen FME, Slats AM, van Empel VPM, Van Gelder IC, Thijssen DHJ, Eijsvogels TMH, Leue C, Crijns HJGM, Linz D, Simons SO. Dyspnea in patients with atrial fibrillation: Mechanisms, assessment and an interdisciplinary and integrated care approach. Int J Cardiol Heart Vasc. 2022 Jul 19;42:101086. doi: 10.1016/j.ijcha.2022.101086. PMID: 35873859; PMCID: PMC9304702.
- Angina-like Symptoms: You may feel chest discomfort or pain resembling a heart attack.
- Fatigue or Decreased Exercise Tolerance: You may feel tired or have difficulty with physical activities.
- Lightheadedness: you may feel dizzy or light-headed.
- Diaphoresis: You will sweat excessively.
- Dizziness: You might feel faint or dizzy.
- Pre-sync and Syncope: You may have pre-syncopal episodes (near-fainting episodes) or syncope (fainting or loss of consciousness).

It’s important to note that these symptoms can vary from person to person. If you or someone you know is experiencing these symptoms, seek medical attention for proper evaluation and guidance.
Diagnosis
If your doctors suspect you have atrial fibrillation, they will ask about your family history. They will also ask about your coffee consumption, exercise intensity, lifestyle, etc. Your physician orders the following tests:
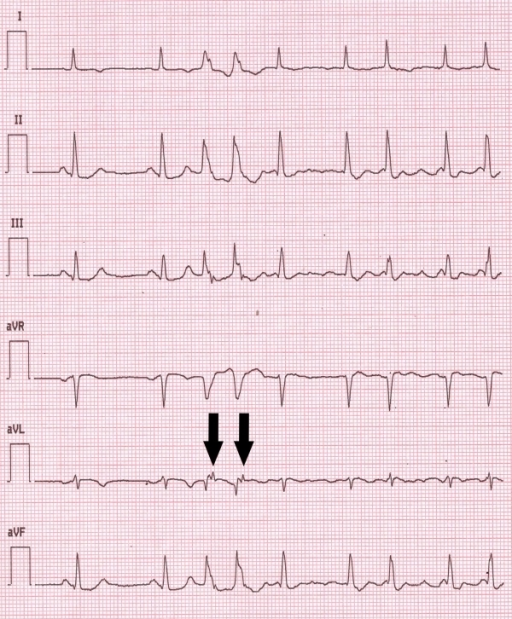
- Echocardiogram: It uses sound waves to create a picture of your heart, allowing doctors to assess its structure and function. Findings from a 12 lead ECG confirm the diagnosis of A-fib. These findings can include irregular “QRS complexes,” absence of” P waves,” etc. The following EKG is from a patient with Paroxysmal Atrial Fibrillation.5De Mattia, L., Brieda, M., Dametto, E., Del Bianco, F., & Nicolosi, G. L. (2012). Paroxysmal atrial fibrillation triggered by a monomorphic ventricular couplet in a patient with acute coronary syndrome. Indian pacing and electrophysiology journal, 12(1), 19–23. https://doi.org/10.1016/s0972-6292(16)30460-0
- Stress test: During a stress test, doctors monitor the heart’s performance while you exercise, providing valuable information about its function under exertion. This shows the severity of the condition and how well any medications are working and helps guide treatments.
- X-ray: An X-ray is for signs of heart problems or related issues. It is done to rule out pulmonary causes of A-fib. X-rays can also give information regarding the heart’s size, nearby blood vessels in the chest, etc.
Some doctors may ask you to wear monitors that record your Heart activity over time. These are to assess your heart rhythm and function. After diagnosis, Blood tests can help identify any underlying illnesses that may be causing fibrillation or contributing to heart problems.
The ICD-10 code for Paroxysmal Atrial fibrillation is “ICD-10-CM Diagnosis Code I48.0”. ICD-10 is a classification list by the WHO. It helps patients with diagnosis and medical insurance reimbursement purposes.6Centers for Medicare & Medicaid Services. (2024). 2024 ICD-10-CM Diagnosis Code I48.0: Paroxysmal atrial fibrillation. Retrieved from https://www.cms.gov/medicare/icd-10/2024-icd-10-cm

Treatment
Treatment for Paroxysmal Atrial Fibrillation targets two key areas. Doctors will either try to establish sinus rhythm (normal heart rhythm) or they will try to control the heart rate. During this, the patient will also be started on Antithrombotic therapy to prevent blood clots.
Antithrombic Therapy:
Doctors recommend antithrombic therapy (blood thinners) based on the patient’s underlying risk factors. Antithrombic therapy has well-documented benefits in high-risk patients. The choice of which antithrombotics to pursue will depend on the patient’s risk of stroke. There are two types of therapy available:
Non-vitamin K Direct Oral Anticoagulants (DOACs)
These include:
- Dabigatran
- Rivaroxaban
- Edoxaban
VKA(Vitamin K Antagonist)
These include:
Warfarin (Coumadin)
DOACs are generally prescribed over Warfarin, as warfarin requires constant monitoring. Both therapies have similar outcomes.7Gerfer, S., Djordjevic, I., Eghbalzadeh, K., Mader, N., Wahlers, T., & Kuhn, E. (2022). Direct oral anticoagulation in atrial fibrillation and heart valve surgery-a meta-analysis and systematic review. Therapeutic advances in cardiovascular disease, 16, 17539447221093963. https://doi.org/10.1177/17539447221093963 Warfarin is used for patients with artificial heart valves or a specific type of irregular heartbeat called valvular A-Fib.
Rhythm Control
Irregular heart rhythm is treated medically or electrically. Your physician will consider your specific symptoms, age, other health issues, drug side effects, and contraindications. Relying solely on medications may have side effects and a lower chance of success. In many cases, combination therapy with a procedure called direct current cardioversion (DCCV) is done.
DCCV
During DCCV (Direct Current Cardioversion), doctors use a general anesthetic and place electrodes on the chest. They pass an electrical impulse across the electrodes to restore normal heart rhythm. Combination therapy has a high success rate. DCCV is for those with low blood pressure or a recent A-Fib episode. Blood thinners may be necessary before and after the procedure. A-Fib can recur even after DCCV. Hence, doctors prescribe antiarrhythmics to reduce the chances of recurrence. If medications aren’t effective, physicians may suggest a catheter or surgical ablation.
Cardiac Ablation
This involves targeting and isolating specific problem areas in the heart. Patients who undergo ablation experience improved symptom relief and a better quality of life. Catheter ablation causes scarring on the inside of the heart by using small burns or freezes to help break up the electrical signals that cause irregular heartbeats.8 Mujović, N., Marinković, M., Lenarczyk, R., Tilz, R., & Potpara, T. S. (2017). Catheter Ablation of Atrial Fibrillation: An Overview for Clinicians. Advances in therapy, 34(8), 1897–1917. https://doi.org/10.1007/s12325-017-0590-z It is minimally invasive. Doctors use surgical ablation as an option when the patient requires heart surgery for other reasons. The risk associated with ablation is generally low. However, there is a small risk of heart valve damage.
Rate Control
If you have asymptomatic A-Fib, the preferred approach is rate control. Your doctor may try different anti-arrhythmic medications to control your heart rate. These include beta-blockers, calcium channel blockers, or digoxin. Digoxin is used when beta-blockers or calcium channel blockers are ineffective in controlling your heart rate. Amiodarone is for when other medications fail. In cases where medical treatment doesn’t work, your doctor may suggest AV node ablation with a permanent pacemaker placement. For asymptomatic or persistent cases, rate control is prioritized to manage symptoms without restoring rhythm. Medications include:
- Beta-blockers (e.g., metoprolol)
- Calcium channel blockers (e.g., diltiazem)
- Digoxin (for refractory cases)
- Amiodarone (for severe cases unresponsive to other treatments)
When medications fail, AV node ablation with pacemaker implantation may be considered.
Lifestyle changes for Paroxysmal Atrial Fibrillation Patients
Your Physician may recommend healthy eating and exercise. This means less salty or fatty foods with more whole grains, fruits, and vegetables. Other changes that might be recommended include:
- Quitting smoking
- Managing alcohol drinking
- Monitoring your cholesterol
- Lowering your blood pressure
Difference Between Atrial fibrillation & Flutter
In atrial fibrillation, the atria beat erratically. In atrial flutter, the atrial beat is regular but faster. Moreover, they often beat more than your ventricles. For every one ventricular beat, you may have multiple atrial beats.
In conclusion, paroxysmal atrial fibrillation is a sudden and intermittent irregular heart rhythm that typically lasts for a short duration. It’s important to seek appropriate medical care to effectively manage paroxysmal atrial fibrillation and reduce the risk of complications. By working closely with healthcare professionals and adopting a personalized treatment plan, individuals with paroxysmal atrial fibrillation can optimize their heart health and improve their overall well-being.
Refrences
- 1National Heart, Lung, and Blood Institute. (n.d.). *Types of Atrial Fibrillation*. Retrieved from [https://www.nhlbi.nih.gov/health/atrial-fibrillation/types]
- 2Brieger D, Amerena J, Attia J, et al., NHFA CSANZ Atrial Fibrillation Guideline Working Group. National Heart Foundation of Australia and the Cardiac Society of Australia and New Zealand: Australian clinical guidelines for the diagnosis and management of atrial fibrillation 2018. Heart Lung Circ2018;27:1209-66. doi:10.1016/j.hlc.2018.06.1043 pmid:30077228
- 3Ludhwani D, Wieters JS. Paroxysmal Atrial Fibrillation [Internet]. PubMed. Treasure Island (FL): StatPearls Publishing; 2020. Available from: https://www.ncbi.nlm.nih.gov/books/NBK535439/
- 4van der Velden RMJ, Hermans ANL, Pluymaekers NAHA, Gawalko M, Elliott A, Hendriks JM, Franssen FME, Slats AM, van Empel VPM, Van Gelder IC, Thijssen DHJ, Eijsvogels TMH, Leue C, Crijns HJGM, Linz D, Simons SO. Dyspnea in patients with atrial fibrillation: Mechanisms, assessment and an interdisciplinary and integrated care approach. Int J Cardiol Heart Vasc. 2022 Jul 19;42:101086. doi: 10.1016/j.ijcha.2022.101086. PMID: 35873859; PMCID: PMC9304702.
- 5De Mattia, L., Brieda, M., Dametto, E., Del Bianco, F., & Nicolosi, G. L. (2012). Paroxysmal atrial fibrillation triggered by a monomorphic ventricular couplet in a patient with acute coronary syndrome. Indian pacing and electrophysiology journal, 12(1), 19–23. https://doi.org/10.1016/s0972-6292(16)30460-0
- 6Centers for Medicare & Medicaid Services. (2024). 2024 ICD-10-CM Diagnosis Code I48.0: Paroxysmal atrial fibrillation. Retrieved from https://www.cms.gov/medicare/icd-10/2024-icd-10-cm
- 7Gerfer, S., Djordjevic, I., Eghbalzadeh, K., Mader, N., Wahlers, T., & Kuhn, E. (2022). Direct oral anticoagulation in atrial fibrillation and heart valve surgery-a meta-analysis and systematic review. Therapeutic advances in cardiovascular disease, 16, 17539447221093963. https://doi.org/10.1177/17539447221093963
- 8Mujović, N., Marinković, M., Lenarczyk, R., Tilz, R., & Potpara, T. S. (2017). Catheter Ablation of Atrial Fibrillation: An Overview for Clinicians. Advances in therapy, 34(8), 1897–1917. https://doi.org/10.1007/s12325-017-0590-z

