Periodontal Surgery or Gum Surgery refers to surgical procedures of the gums (gingiva) and periodontium (structures that surround the tooth, including bone and soft tissues). Patients undergo periodontal surgery for a variety of reasons, ranging from gum disease treatment to esthetic improvements. Initial healing from the surgery generally takes 1-2 weeks. However, complete healing of the tissues can take up to several months. So, let’s find out what you can expect from a periodontal surgery.
Who is an Ideal Candidate for a Periodontal Surgery?
You are a good candidate for periodontal surgery if you have:
- Severe gum disease (gingival bleeding and recession)
- Periodontal disease (bone loss)
- Halitosis (bad breath)
- Tooth mobility due to bone loss
- Non-resolving gum disease symptoms (with non-surgical/minimally invasive strategies)
Your dentist will try to manage the condition with conservative methods and move towards intervention only if surgery is unavoidable. Health professionals prefer patients who do not have any health-deteriorating habits like drinking and smoking etc.
Contraindications:
Relative contraindications exist in cases where the treatment outcomes can become compromised. Doctors do not prefer carrying out periodontal surgery in the following patient scenarios:
- Diabetes mellitus: The Presence of underlying comorbidities like diabetes increases the risk of postoperative complications (wound dehiscence, delayed wound healing, etc.).1Nibali, L., Gkranias, N., Mainas, G., & Di Pino, A. (2022). Periodontitis and implant complications in diabetes. Periodontology 2000, 90(1), 88-105.
- Tobacco/cigarette smoking: Smokers are generally not preferred patients for periodontal surgery because tobacco smoking promotes gingival recession and periodontal disease, which negatively impacts the treatment outcomes.2Leite, F. R., Nascimento, G. G., Scheutz, F., & Lopez, R. (2018). Effect of smoking on periodontitis: a systematic review and meta-regression. American journal of preventive medicine, 54(6), 831-841.
- Immunosuppressant disease/drugs: People suffering from weak immunity (AIDS, hepatitis patients) and patients on immunosuppressant drug therapy have higher chances of post-operative complications (especially infection).
Periodontal Surgery Types
Based on the purpose of the intervention, we divide periodontal surgeries into different types:
Gum Disease Surgeries:
Periodontitis (gum disease) is a common oral malady characterized by gum recession and loss of alveolar bone. The loss of interdental bone leads to the formation of periodontal pockets. The exposed teeth (after bone loss) present with symptoms like hot/cold sensitivity, pain, and bad breath (halitosis).
It affects around 20-50% of the global population. However, despite the high prevalence, only a small number of patients seek surgical treatment for their problems.3Nazir, M. A. (2017). Prevalence of periodontal disease, its association with systemic diseases and prevention. International journal of health sciences, 11(2), 72. Doctors employ different types of procedures to alleviate symptoms arising from receding gums and resorbing bone.
Gingivectomy
Excision of gums, i.e., gingivectomy, is the second most common periodontal surgical procedure. Dentists remove the affected gums in periodontal disease cases where there is excessive thickening of the gingiva in conjunction with bone defects.
Gingivoplasty
The surgical reshaping (and recontouring) of the gums is referred to as gingivoplasty. Dental professionals consider the procedure in cases of defective gums due to periodontal disease and for esthetic considerations.4Evangelista, I. M., Candido, L. R., de Araújo, J. J. S., & Scriboni, A. B. (2024). Major considerations of gingivoplasty: a concise systematic review. MedNEXT Journal of Medical and Health Sciences, 5(S4).
Wedge Procedure
The wedge procedure is a type of gingivectomy surgery in which the surgeon removes a small portion of the gingival tissue via a wedge/square-shaped incision. This type of minimal surgery is selected when the pocket-associated gingival thickening is confined to one tooth surface only (mesial or distal).
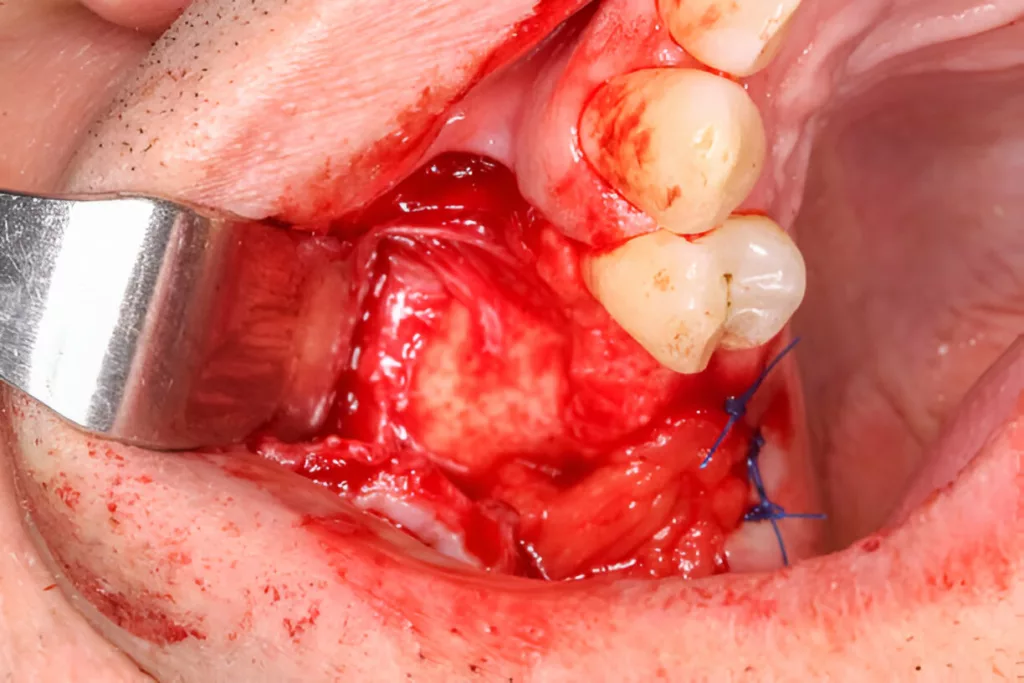
Gingival Flap Surgery
The most commonly employed surgical procedure in the management of periodontal loss/disease is the gingival flap surgery. It is also known as open flap debridement.5Akram, H. M., Zaidoon, R., & Alaa, R. (2025). Prevalence and characteristics of periodontal surgery procedures in postgraduate periodontic clinics: an epidemiological analysis. Folia Medica, 67(2), e143232. Doctors also refer to it as surgical scaling and root planning. In open flap debridement, a periodontist makes an incision in the gums and exposes the roots by lifting a section of the gums. After gaining access to the hard tissues, the surgeon/periodontist repairs the damaged bone and performs the debridement of the roots. The main aim of this surgery is to eliminate periodontal pockets that cause symptoms. A flap surgery is ideal for cases with suprabony pockets and horizontal bone loss.
Bone Surgery
If the bottom part of the periodontal pocket lies apical(towards the tooth root) to the alveolar bone level, it is called an infrabony pocket. Such pockets are mostly seen in cases of vertical bone loss. To correct infrabony pockets and residual pockets, doctors go deeper than flap surgery into the periodontium, remove the walls of the bone defect, and restore healthy bony architecture. As it involves restructuring the bone, the procedure is also called osseous surgery.
Regenerative/Replacement Gum Surgeries:
Next come the surgical procedures, which are done to regenerate the lost tissues. Doctors can adopt a variety of approaches to promote the regrowth of periodontal ligament, cementum (of roots), and lost bone. It is noteworthy here that the success of a regenerative periodontal surgery relies heavily on the expertise of the surgeon and the lifestyle habits of the patients. Therefore, it is important to get the procedure done from an expert periodontist or oral surgeon and abstain from negative activities like smoking, etc.
Multiple regenerative procedures that help cover your gingival and bony defects include:
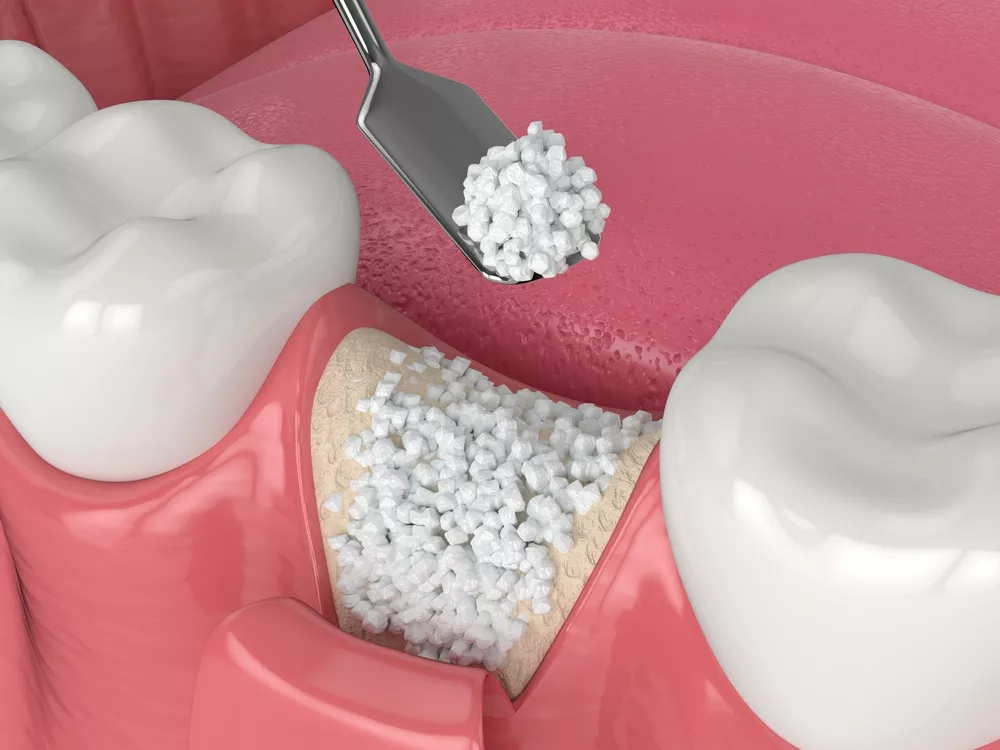
Bone Grafting
In cases with significant bone loss, doctors opt for bone grafts to cover the defects caused by periodontal disease. There are different types of bone grafts, including autogenous grafts (from the patient), allografts (from another human donor), xenografts (from animals), and alloplasts (man-made materials). It helps promote bone regrowth, which consequently prevents tooth loss and mobility. There is sufficient data that suggests that bone grafting procedures lead to appreciable bone filling in periodontitis.6Balaji, V. R., Manikandan, D., & Ramsundar, A. (2020). Bone grafts in periodontics. Matrix Science Medica, 4(3), 57-63.
Guided Tissue Regeneration (GTR)
In the present era, guided tissue regeneration is one of the most commonly adopted procedures because it shows superb results. In this procedure, the periodontist uses a barrier membrane (between the bone and soft tissue) to guide appropriate regrowth of the tooth-supporting structures. The scaffolding technologies and guided tissue regeneration have shown great results and hold immense potential in periodontal disease management. 7Alqahtani, A. M., Moorehead, R., & Asencio, I. O. (2023). Guided tissue and bone regeneration membranes: a review of biomaterials and techniques for periodontal treatments. Polymers, 15(16), 3355. Doctors use different types of biocompatible resorbable and non-resorbable materials that act as temporary scaffolds until tissues grow completely.8Deng, Y., Liang, Y., & Liu, X. (2022). Biomaterials for periodontal regeneration. Dental Clinics of North America, 66(4), 659-672.
Biologics
Sometimes, doctors use biologics for periodontal tissue regeneration. Most commonly used biologics include growth factors and platelet-concentrates like platelet-rich plasma (PRP), platelet-rich fibrin variants (PRF, A-PRF, etc.), and sticky bone for the purpose. Studies show that the combination of biologics and bone grafting plays a positive role in the management of infrabony periodontal defects.9Tavelli, L., Chen, C. Y., Barootchi, S., & Kim, D. M. (2022). Efficacy of biologics for the treatment of periodontal infrabony defects: an American Academy of Periodontology best evidence systematic review and network meta‐analysis. Journal of Periodontology, 93(12), 1803-1826.
Mucogingival Surgeries:
Defects of the mucosa-gingiva require mucogingival surgeries. In most cases, doctors perform gingival grafts to cover areas of thin epithelium or lost soft tissue.
Connective Tissue Graft
In this, the surgeon takes the whole of connective tissue from the donor site (usually the palate) while sparing the top layer and harvests it in the affected site. Sometimes, doctors go for acellular dermal matrix (instead of the connective tissue graft), which is a structurally intact collagen matrix derived from human/animal skin. Both these techniques show good results in the correction of localized recession.
Soft Tissue Grafting
In cases of gum thinning or gingival loss, periodontists go for a gum graft. Doctors mostly use autogenous grafts (gingival grafts from the patient) and place them in position. There are different types of gingival grafts that the surgeon can adopt, including:
- Free gingival graft: In this type, a small graft is taken from the palate and stitched at the recipient site with some interdental tissue to richer vascular supply to the graft.
- Lateral (pedicle) graft: There is a pedicular extension of the adjacent tissue over the exposed roots (that have undergone recession).
- Connective tissue graft: In this, the surgeon takes the whole of connective tissue from the donor site (usually the palate) while sparing the top layer and harvests it in the affected site. Sometimes, doctors go for acellular dermal matrix (instead of the connective tissue graft), which is a structurally intact collagen matrix derived from human/animal skin. Both these techniques show good results in the correction of localized recession.
Esthetic & Restorative Surgeries:
Crown Lengthening
Prosthodontists (restorative dentists) often collaborate with periodontists to achieve the ideal requirements for tooth prosthesis. Sometimes, the available tooth structure is insufficient for endodontic treatment or ferrule preparation. In such cases, periodontists perform crown lengthening, which is characterized by removing gum and part of the surrounding bone to expose the crown of the tooth. Another similar procedure is biologic shaping, in which the surgeon removes bone with specific burs and attaches the gingival flap to clean dentin surfaces. Studies reveal that long-term retention of restorations can be achieved with crown lengthening procedures.10Mugri, M. H., Sayed, M. E., Nedumgottil, B. M., Bhandi, S., Raj, A. T., Testarelli, L., … & Patil, S. (2021). Treatment prognosis of restored teeth with crown lengthening vs. deep margin elevation: a systematic review. Materials, 14(21), 6733.
Crown Exposure & Gingivectomy

In addition to prosthodontists, orthodontists also seek help from periodontists to obtain the best treatment results. Gummy smile patients have excessive gum display, which is attributed to different reasons, including tooth malposition and gum overgrowth. Periodontal specialists remove the overgrown gums and expose the anatomic crown fully, greatly improving the esthetics. The removal of a segment of gum falls under the category of gingivectomy.
Periodontal Surgery Procedures
Preparation:
You should stop anticoagulants like aspirin and blood thinner medicines like clopidogrel 24-48 hours before the surgery. However, some clinicians believe that dental surgical procedures like extraction can be performed without stopping aspirin therapy because aspirin stoppage predisposes the patient to adverse thromboembolic complications.11Verma, G. (2014). Dental extraction can be performed safely in patients on aspirin therapy: a timely reminder. International Scholarly Research Notices, 2014(1), 463684. You must consult your cardiologist/physician regarding the drug stoppage.
You should have someone to drive you back home because the effects of anesthesia (especially after conscious sedation) can temporarily impact your abilities. Patients are also advised to stop smoking and drinking alcohol a couple of days before surgery to enhance healing.
Procedure:
Generally, gum specialists perform periodontal surgery under local anesthesia. Conscious oral sedation (nitrous oxide inhalation) is reserved for patients with high dental anxiety. General anesthesia is rarely used for gum surgeries.
After giving anesthesia, the surgeon makes an incision in the gums. Nowadays, most modern clinics prefer specialized medical lasers to cut through the skin and mucosa. Laser periodontal surgery is common and pretty effective nowadays. According to clinical studies, laser gingivectomy shows favorable results in improving periodontal health parameters and orthodontic treatment outcomes.12Zeballos, B. K. C., Rubina, Y. N. A., Meza-Mauricio, J., Cafferata, E. A., & Vergara-Buenaventura, A. (2024). Laser gingivectomy for maintaining periodontal health in fixed orthodontic patients: a systematic review. Lasers in Dental Science, 8(1), 1-15. Moreover, patients now prefer diode laser gingivectomies over conventional scalpel surgeries because there is less bleeding and lower levels of pain.
Most periodontal procedures take 1-2 hours to complete. Anesthesia and incision-making are similar for the majority of periodontal surgeries. However, there are some differences between the various types of procedures:
Gingivectomy
After identifying the pathological region, the surgeon cuts through the gums using a scalpel or laser. After cutting out the swollen/overgrown part, the doctor reshapes the remaining gums to give them a good contour and stitches them back. He then places a soft (putty-like) dressing over the area exposed after gingivectomy to speed up healing.
Gingival Flap Surgery
Dentists across the globe prefer the Modified Widman flap surgery technique to treat suprabony pockets. In this very technique, the surgeon makes multiple connecting incisions (close to the root surface) in your gingiva instead of one. The surgeon keeps the gingival reflection limited to the root portion of the teeth. This has the advantage of minimal tissue removal, which ultimately minimizes gingival recession. After the procedure, there is expected formation of junctional epithelium, which improves gum attachment and minimizes pockets.
Osseous Surgery
In bone surgery, your dentist will raise a full-thickness gingival flap (with the help of a scalpel or laser) and perform root debridement using surgical instruments (surgical burs). Professionals selectively remove bone pieces to contour the bony architecture. After bone removal is complete, the doctor sutures the gums together. In some cases, doctors perform a modified form of osseous surgery, i.e., fiber retention osseous resective surgery, in which there is a split-thickness gum flap.
Guided Tissue Regeneration (GTR) & Bone Grafting
GTR is done in conjunction with grafting procedures. The surgeon raises a gingival flap, accesses the area, and reshapes the bone to remove the defects. Next comes the graft material (autogenous, xenograft, allograft, etc.), which is carefully put in place. After debridement and graft placement are complete, the surgeon places a regenerative membrane over the bone, which separates it from the outer gum epithelia. Different types of GTR membrane materials are available. Your dentist will choose the ideal material according to your needs.
Mucogingival Surgery
In a free gingival graft, the surgeon creates an envelope flap at the mucogingival junction (of the recipient site). The flap is not full but rather split-thickness, which allows a thick layer of perisoteum to stay. Then, your surgeon will take a gingival graft from the palate (donor site) by making a split-thickness incision. The attained flap is then harvested at the soft tissue pouch created at the recipient site and fixed in place with the help of sutures.
In lateral sliding, the doctor mobilizes the tissue adjacent to the defective (minor) gums by making a split-thickness incision. The incised (but still attached) part of the neighboring gum is extended over the denuded/thin gingiva and fixed in position with sutures.
In connective tissue grafting, a split-thickness flap is created at the recession area. A piece of connective tissue graft is harvested from the palate and inserted into the recession area after cleaning the recipient site. The donor flap joins the receded area, fixed with stitches.
You can learn more about gum grafting by clicking here!
Crown Lengthening
In clinical crown lengthening, the doctor cuts the gingiva surrounding the intended tooth and reattaches it to a more apical level. In some cases, there is a need to remove (excise) the excess gum tissue.
Periodontal Surgery Recovery
Your recovery from the surgery depends on multiple factors, including the extent of periodontal disease (or surgery), your general health (presence of comorbidities like diabetes or hepatitis, etc.), and habits like smoking and drinking, etc.
On the day of Surgery:
You might feel slight discomfort and bleeding on the day of the procedure, which settles down by the next day. Eating ice cream (with preferred application on the surgical site) can help lower post-op inflammation. You can resume your work the next day without any significant trouble. Mild bleeding is normal, but you should report to your dentist if there is excessive bleeding.
1-2 weeks after Surgery:
Initial healing of the surgical site occurs during this period, and patients are advised to take a soft diet like scrambled eggs, yogurt, and cheese, etc. However, complete healing may take several months, depending on the type of procedure you underwent. You can get your stitches removed 7-10 days after the surgery.
Periodontal Surgery Aftercare:
In healthy cases, there is uneventful post-operative healing. However, you need to strictly follow the doctor’s instructions.
- You should avoid smoking/drinking, spicy foods, vigorous spitting/gargling, and hectic exercises during the first couple of weeks after surgery.
- To address bleeding, you can apply light pressure on the surgical site using a tea bag or gauze.
- Apply ice on the outside of your face (for 20 minutes) during the first 24 hours.
- Your doctor may also advise you to use an antibiotic mouthwash to minimize the chances of infection.
- Due to the wound, your doctor might also advise you to abstain from brushing or flossing until the site has healed.
Are there any Post-Operative Complications associated with Periodontal Surgery?
You may experience general postoperative complications like bleeding, bruising, swelling, pain, and tissue discoloration. Grafting patients report relatively more pain and swelling on the donor site (mostly palate) than the recipient site. As per a clinical study, the most common post-operative complications noted after periodontal surgery were:13Askar, H., Di Gianfilippo, R., Ravida, A., Tattan, M., Majzoub, J., & Wang, H. L. (2019). Incidence and severity of postoperative complications following oral, periodontal, and implant surgeries: a retrospective study. Journal of periodontology, 90(11), 1270-1278.
- Dentinal hypersensitivity
- Excessive pain
- Moderate bleeding
Post-operative infection is rare and can be easily managed with oral antibiotic therapy. Over-the-counter pain killers like ibuprofen and cold application help with pain and swelling.
Pocket depth reduction can lead to gum recession and root exposure in some cases, which ultimately leads to dentin hypersensitivity. In some cases, the free gingival graft can undergo negative changes, such as sloughing off and undergoing drastic color changes. However, these complications are rare.
Final Word
Periodontal surgery is an umbrella term that covers various types of gum surgeries. Excess gingival tissue (due to chronic disease, orthodontic treatment, or medicines) is removed via scalpel or lasers (in laser gingivectomy). Gingival flap surgeries and osseous surgeries access the root surfaces of the teeth and debride them while recontouring the gingiva and bone of the periodontal pockets. Regeneration of lost tissues is done with guided tissue regeneration membranes. Doctors use GTR membranes in conjunction with ridge augmentation to ensure rapid healing of the structures. Gingival grafts (from animals, man-made sources, and the patient himself) are successfully harvested to cover the mucogingival defects.
Crown lengthening is done to improve the length of the clinical crown for restorations. Crown exposure is adopted in orthodontic patients to improve the appearance of gummy smiles. Generally performed under local anesthesia, most periodontal surgeries finish within a couple of hours, and initial healing completes within 1-2 weeks. Complications are rare. However, smoking, alcohol consumption, and diabetes negatively impact treatment outcomes by altering the healing potential of the body.
Refrences
- 1Nibali, L., Gkranias, N., Mainas, G., & Di Pino, A. (2022). Periodontitis and implant complications in diabetes. Periodontology 2000, 90(1), 88-105.
- 2Leite, F. R., Nascimento, G. G., Scheutz, F., & Lopez, R. (2018). Effect of smoking on periodontitis: a systematic review and meta-regression. American journal of preventive medicine, 54(6), 831-841.
- 3Nazir, M. A. (2017). Prevalence of periodontal disease, its association with systemic diseases and prevention. International journal of health sciences, 11(2), 72.
- 4Evangelista, I. M., Candido, L. R., de Araújo, J. J. S., & Scriboni, A. B. (2024). Major considerations of gingivoplasty: a concise systematic review. MedNEXT Journal of Medical and Health Sciences, 5(S4).
- 5Akram, H. M., Zaidoon, R., & Alaa, R. (2025). Prevalence and characteristics of periodontal surgery procedures in postgraduate periodontic clinics: an epidemiological analysis. Folia Medica, 67(2), e143232.
- 6Balaji, V. R., Manikandan, D., & Ramsundar, A. (2020). Bone grafts in periodontics. Matrix Science Medica, 4(3), 57-63.
- 7Alqahtani, A. M., Moorehead, R., & Asencio, I. O. (2023). Guided tissue and bone regeneration membranes: a review of biomaterials and techniques for periodontal treatments. Polymers, 15(16), 3355.
- 8Deng, Y., Liang, Y., & Liu, X. (2022). Biomaterials for periodontal regeneration. Dental Clinics of North America, 66(4), 659-672.
- 9Tavelli, L., Chen, C. Y., Barootchi, S., & Kim, D. M. (2022). Efficacy of biologics for the treatment of periodontal infrabony defects: an American Academy of Periodontology best evidence systematic review and network meta‐analysis. Journal of Periodontology, 93(12), 1803-1826.
- 10Mugri, M. H., Sayed, M. E., Nedumgottil, B. M., Bhandi, S., Raj, A. T., Testarelli, L., … & Patil, S. (2021). Treatment prognosis of restored teeth with crown lengthening vs. deep margin elevation: a systematic review. Materials, 14(21), 6733.
- 11Verma, G. (2014). Dental extraction can be performed safely in patients on aspirin therapy: a timely reminder. International Scholarly Research Notices, 2014(1), 463684.
- 12Zeballos, B. K. C., Rubina, Y. N. A., Meza-Mauricio, J., Cafferata, E. A., & Vergara-Buenaventura, A. (2024). Laser gingivectomy for maintaining periodontal health in fixed orthodontic patients: a systematic review. Lasers in Dental Science, 8(1), 1-15.
- 13Askar, H., Di Gianfilippo, R., Ravida, A., Tattan, M., Majzoub, J., & Wang, H. L. (2019). Incidence and severity of postoperative complications following oral, periodontal, and implant surgeries: a retrospective study. Journal of periodontology, 90(11), 1270-1278.

