Photokeratitis is an inflammation of the cornea caused by exposure to ultraviolet (UV) rays. It is similar to sunburn but affects the eyes. It can be acute, occurring immediately after high UV exposure, or chronic, developing after prolonged low-level exposure. Symptoms include eye pain, redness, blurred vision, and light sensitivity, typically lasting 24-48 hours. Severe cases may also cause temporary vision impairment. Major risk factors include outdoor activities at high altitudes or using UV-emitting devices.
What is Photokeratitis?
The term “photokeratitis” is derived from “photo” (light) and “keratitis” (inflammation of the cornea). The cornea is the transparent, dome-shaped structure covering the pupil and iris, playing a crucial role in focusing light onto the retina. In photokeratitis, UV rays damage the corneal epithelial cells, leading to inflammation. The condition often affects both eyes and is sometimes referred to as “snow blindness” (common in snowy environments where UV light reflects strongly) or “welder’s arc” (due to unprotected exposure to welding arcs).1Izadi, M., Jonaidi-Jafari, N., Pourazizi, M., Alemzadeh-Ansari, M. H., & Hoseinpourfard, M. J. (2018). Photokeratitis induced by ultraviolet radiation in travelers: A major health problem. Journal of Postgraduate Medicine, 64(1), 40–46. https://doi.org/10.4103/jpgm.JPGM_52_17
In addition to sunlight, other sources of UV rays include welding arcs, tanning lamps, and high-intensity UV radiation used for therapeutic purposes in conditions like psoriasis, as well as germicidal UV lamps.
Types of Photokeratitis
Photokeratitis can be acute or chronic.
Acute Photokeratitis
Acute Photokeratitis is a temporary condition that occurs immediately after exposure to high levels of UV radiation. Common examples include snow blindness from skiing without protective eyewear or welder’s flash due to unshielded welding.
Chronic Photokeratitis
Chronic photokeratitis is a condition that occurs after continuous exposure to low levels of UV radiation over time. It is less common than acute photokeratitis. It is more subtle in onset and may not present with immediate symptoms. However, it can contribute to long-term complications like cataracts and macular degeneration.
Symptoms of Photokeratitis
The important symptoms of photokeratitis are as follows:2Chan, J. Y. Y., Chow, V. W. S., Chan, C. K. M., Chan, E. Y. M., Lau, J. S. K., Lai, T. Y. Y., Young, A. L., & Tham, C. C. Y. (2024). Photokeratitis in Outdoor Event Participants Exposed to UV Radiation Display. JAMA Ophthalmology, 142(6), 568–571. https://doi.org/10.1001/jamaophthalmol.2024.1092
- Eye pain
- Eye redness
- Watery eye or eye tearing
- Blurred vision
- Sensitivity of exposure to light (photophobia)
- A gritty or foreign body sensation, especially on eye closure
- Rarely, halos, headaches, or temporary loss of vision
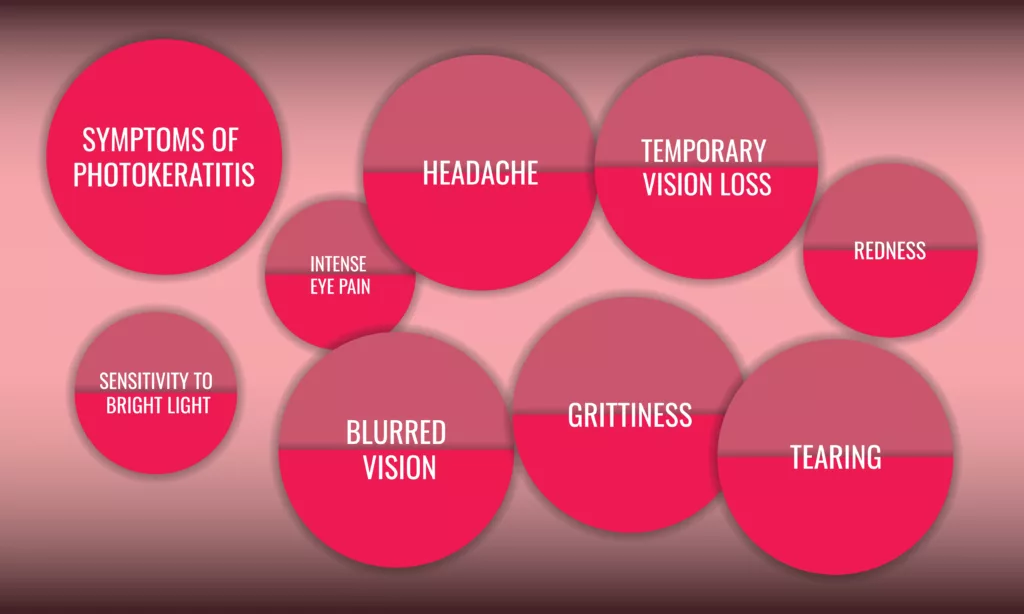
The symptoms appear within 6-8 hours and persist for 48 hours. The longer you are exposed to UV radiation, the worse the symptoms become.
Long-Term Risks of Chronic UV Exposure
While photokeratitis itself usually resolves without long-term damage, prolonged or repeated UV exposure can increase the risk of:
- Cataracts: Cloudy areas in the lens of the eye that impairs vision3Roberts JE. Ultraviolet radiation as a risk factor for cataract and macular degeneration. Eye Contact Lens. 2011 Jul;37(4):246-9. doi: 10.1097/ICL.0b013e31821cbcc9. PMID: 21617534.
- Macular degeneration: Loss of central vision due to retinal damage
- Pterygium: A pinkish tissue growth extending from the conjunctiva onto the cornea4Mushtaq, Iqra; Maghdum, Renu; Bhavsar, Deepaswi; Iqbal, Banyameen1,. Correlation between Ocular Sun Exposure and Pterygium: A Hospital-Based Study. Journal of the Scientific Society 47(3):p 176-179, Sep–Dec 2020. | DOI: 10.4103/jss.JSS_34_20
Causes of Photokeratitis
The major cause of photokeratitis is UV radiation from the sun. UV-A and UV-B radiations are dangerous for the eyes, causing several conditions like photokeratitis, cataracts, macular degeneration, and pterygium.5Chawda, D., & Shinde, P. (2022). Effects of Solar Radiation on the Eyes. Cureus, 14(10), e30857. https://doi.org/10.7759/cureus.30857
Other sources of UV radiation that can cause photokeratitis include:
- Reflected sunlight from surfaces of snow, ice, water, or cement.
- Lamps in tanning beds and booths
- Laser light
- Halogen desk lamp
- Mercury vapor lamp
- Electric sparks or lightning
- Welding arcs
- Photography flood lamps
- Lights used for disinfection and medical treatments
Risk Factors
Certain factors increase the risk of developing photokeratitis, including:
- Spending prolonged time in the sun while engaging in activities like hiking, skiing, swimming, or outdoor labor
- Using tanning booths or working with UV-emitting equipment
- Living at higher altitudes, where UV exposure is greater due to thinner atmospheric protection
Proper protective measures, such as wearing UV-blocking eyewear and limiting direct UV exposure, can significantly reduce the risk of photokeratitis.6Jha K. N. (2012). High Altitude and the Eye. Asia-Pacific journal of ophthalmology (Philadelphia, Pa.), 1(3), 166–169. https://doi.org/10.1097/APO.0b013e318253004e
Diagnosis of Photokeratitis
Eye specialists usually diagnose photokeratitis on examination and history taking. The doctor will ask about environmental exposure, occupational risks, and symptoms such as eye pain, redness, and light sensitivity.
To confirm the diagnosis and assess corneal damage, the specialist may use fluorescein dye, which highlights irregularities on the corneal surface. This is followed by a slit lamp examination, a procedure that uses a focused, high-intensity light to examine the eyes in detail. These diagnostic steps help differentiate photokeratitis from other eye conditions and determine the extent of corneal injury.7Chen, K. K., Hsieh, S. M., Chang, H. H., & Lin, D. P. (2023). Diagnosis of Photokeratitis by Tear Ferning Using a Novel Set of SK Grading Criteria in a UVB-Induced Mouse Model. Translational vision science & technology, 12(6), 25. https://doi.org/10.1167/tvst.12.6.25
Home Care for Photokeratitis
If you suspect you have photokeratitis, the first step is to seek medical advice from a healthcare professional, ideally an eye specialist. In the meantime, you can take the following steps to help alleviate symptoms:
- Rest in a Dark Room: Minimizing light exposure by resting in a dark room can provide relief.
- Avoid Contact Lenses: If you wear contact lenses, remove them until cleared by your doctor.
- Cold Compress: Applying a cold washcloth or sponge to your eyes can reduce discomfort.
- Wear Sunglasses: If you must go outside, wearing sunglasses will help protect your eyes from light sensitivity.
- Artificial Tears: These can help relieve dryness and irritation, but they should be used under the guidance of a healthcare provider.
The condition usually resolves in 24-48 hours. If it persists after this or the symptoms get worse, immediately see your healthcare professional. It is best to see an eye specialist.
Treatment of Photokeratitis
If medical therapy is necessary, your eye specialist or healthcare provider will give you the following medications:8Ting, M. A., Saha, K., & Robbie, S. (2016). Mass photokeratitis following ultraviolet light exposure at a nightclub. Contact lens & anterior eye: the journal of the British Contact Lens Association, 39(4), 316–317. https://doi.org/10.1016/j.clae.2016.01.009
- Local anesthesia for examination purposes to confirm the diagnosis
- Artificial tears for relief of symptoms
- Eye ointment to relieve the discomfort and soothe the eye
- Oral analgesics for pain relief like ibuprofen
- Sometimes, an infection supersedes photokeratitis. In this case, antibiotics like chloramphenicol are necessary.
- If a ciliary muscle spasm occurs, a cycloplegic drug is given, like cyclopentolate.
- In severe cases, the doctor might prescribe steroid eye drops as well.
Prevention of Photokeratitis
To reduce the risk of photokeratitis, consider the following preventive measures:
-
- Use goggles or sunglasses: Choose protective eyewear with 100% UV protection, especially in high-altitude or snowy regions where UV reflection is significant.
- Wear a hat with a wide brim: This can provide extra shade and limit direct UV exposure to your eyes.
- Use protective eye gear: Always wear appropriate protective equipment if your job involves UV exposure, such as welding or working with UV lamps.
- Minimize UV exposure: Avoid prolonged exposure to direct sunlight, especially during peak UV radiation hours (10 a.m. to 4 p.m.).
In conclusion, photokeratitis is a preventable condition primarily caused by UV radiation exposure. Awareness of the risks and taking protective measures, such as wearing appropriate eyewear, can significantly reduce the likelihood of developing this condition. Early recognition and prompt treatment are essential to avoid complications and ensure a quick recovery. By understanding the symptoms and practicing preventive care, individuals can protect their eyes from the harmful effects of UV radiation and maintain healthy vision.
Refrences
- 1Izadi, M., Jonaidi-Jafari, N., Pourazizi, M., Alemzadeh-Ansari, M. H., & Hoseinpourfard, M. J. (2018). Photokeratitis induced by ultraviolet radiation in travelers: A major health problem. Journal of Postgraduate Medicine, 64(1), 40–46. https://doi.org/10.4103/jpgm.JPGM_52_17
- 2Chan, J. Y. Y., Chow, V. W. S., Chan, C. K. M., Chan, E. Y. M., Lau, J. S. K., Lai, T. Y. Y., Young, A. L., & Tham, C. C. Y. (2024). Photokeratitis in Outdoor Event Participants Exposed to UV Radiation Display. JAMA Ophthalmology, 142(6), 568–571. https://doi.org/10.1001/jamaophthalmol.2024.1092
- 3Roberts JE. Ultraviolet radiation as a risk factor for cataract and macular degeneration. Eye Contact Lens. 2011 Jul;37(4):246-9. doi: 10.1097/ICL.0b013e31821cbcc9. PMID: 21617534.
- 4Mushtaq, Iqra; Maghdum, Renu; Bhavsar, Deepaswi; Iqbal, Banyameen1,. Correlation between Ocular Sun Exposure and Pterygium: A Hospital-Based Study. Journal of the Scientific Society 47(3):p 176-179, Sep–Dec 2020. | DOI: 10.4103/jss.JSS_34_20
- 5Chawda, D., & Shinde, P. (2022). Effects of Solar Radiation on the Eyes. Cureus, 14(10), e30857. https://doi.org/10.7759/cureus.30857
- 6Jha K. N. (2012). High Altitude and the Eye. Asia-Pacific journal of ophthalmology (Philadelphia, Pa.), 1(3), 166–169. https://doi.org/10.1097/APO.0b013e318253004e
- 7Chen, K. K., Hsieh, S. M., Chang, H. H., & Lin, D. P. (2023). Diagnosis of Photokeratitis by Tear Ferning Using a Novel Set of SK Grading Criteria in a UVB-Induced Mouse Model. Translational vision science & technology, 12(6), 25. https://doi.org/10.1167/tvst.12.6.25
- 8Ting, M. A., Saha, K., & Robbie, S. (2016). Mass photokeratitis following ultraviolet light exposure at a nightclub. Contact lens & anterior eye: the journal of the British Contact Lens Association, 39(4), 316–317. https://doi.org/10.1016/j.clae.2016.01.009

