What is Pica Disorder?
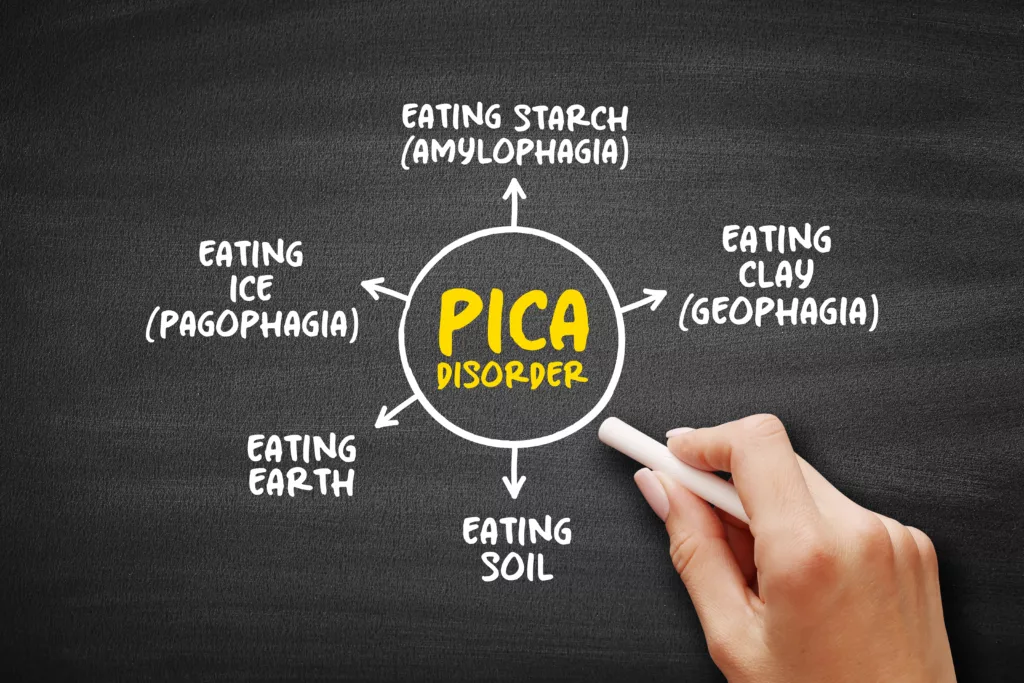
Pica Eating Disorder is a condition that involves an irreversible urge to ingest inedible or non-food substances devoid of nutritional value. According to the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), Pica is defined as eating a wide variety of non-food and non-nutritive substances for at least one month in children older than two years of age that has harmful consequences for your body. The types of items ingested in Pica disorder can vary widely. They may include substances such as earth (geophagy), raw starches (amylophagy), ice (pagophagia), charcoal, ash, paper, chalk, cloth, baby powder, coffee grounds, and eggshells.1Young SL. Pica in pregnancy: new ideas about an old condition. Annu Rev Nutr. 2010 Aug 21;30:403-22.
Pica is reported worldwide; geophagia is the most common form. It is most commonly reported in children but can also occur in young patients having a psychological impairment. This eating disorder also affects women during pregnancy. It usually occurs as an isolated disorder but can coexist with other mental illnesses like obsessive-compulsive disorder (OCD), schizophrenia, and autism.
Research shows that 25-33% of young children have this eating disorder. In pregnant women, it usually occurs during their first pregnancy. The prevalence of pica in pregnant women is about 27.8%. It is also reported in patients with sickle cell disease. About 34% of the patients with Sickle cell disease have this disorder.2Burke, M., MD. (n.d.). Pica: Practice Essentials, Background, Etiology. https://emedicine.medscape.com/article/914765-overview#a5
Causes of Pica Disorder:
The exact cause of pica eating disorder is still unknown, but some factors like psychological, nutritional, and biochemical factors contribute to pica disorder.
Psychological
Pica is usually associated with mental health problems or stress. Poor parental care is a leading cause of pica disorder. Psychological factors that contribute to causing pica eating disorder are:3Singhi S, Singhi P, Adwani GB. Role of psychosocial stress in the cause of pica. Clin Pediatr (Phila). 1981 Dec;20(12):783-5.
- Stress
- Child abuse
- Child neglect
- Maternal deprivation
- Mental disorders (autism, OCD, and schizophrenia)
- Parental separation
Nutritional
Pica disorder is most common in malnourished children living in unhygienic environments. Nutritional deficiency compels the patient to eat whatever he sees. Poor socioeconomic status, unhealthy diet, and malnutrition are associated with pica eating disorders. Biochemical factors that may lead to pica disorder include mineral and nutrient deficiencies, including iron, zinc, calcium, and vitamin deficiency. Geophagia is specifically linked ti iron deficiency.4Nchito M, Geissler PW, Mubila L, Friis H, Olsen A. Effects of iron and multimicronutrient supplementation on geophagy: a two-by-two factorial study among Zambian schoolchildren in Lusaka. Trans R Soc Trop Med Hyg. 2004 Apr;98(4):218-27.
Risk Factors of Pica Disorder
Although there are many risk factors for pica eating disorder, the most common factors are:5Ezzeddin N, Zavoshy R, Noroozi M, Jahanihashemi H, Riseh SH. Prevalence and risk factors for pica during pregnancy in Tehran, Iran. Eat Weight Disord. 2015 Dec;20(4):457-63.
- Mental stress
- Positive family history
- Low socioeconomic status
- Cultural factors
- Pregnancy6Konlan KD, Abdulai JA, Konlan KD, Amoah RM, Doat AR. Practices of pica among pregnant women in a tertiary healthcare facility in Ghana. Nurs Open. 2020 Jan 28;7(3):783-792. doi: 10.1002/nop2.451. PMID: 32257266; PMCID: PMC7113508.
- Epilepsy
- Malnutrition
What are the Signs & Symptoms of Pica Eating Disorder?
Clinical presentation of pica eating disorder is variable and depends upon the type of food ingested and the duration of this activity. The signs and symptoms of pica are:
- Nausea
- Constipation
- Diarrhea
- Abdominal cramps
- Intestinal obstruction due to bizarre eating patterns
- Weight loss
- Behavior problems
- Lead poisoning: people with pica usually ingest hard metallic substances that contain lead and other metals. Signs of lead poisoning are lethargy, headache, seizures, and cranial nerve palsy.
- Ingestion of infectious agents leads to infections. It can lead to ascariasis (infestation with eggs of worms in the intestines). Other symptoms of infections include fever, enlargement of the liver and spleen, infection in the brain, and vision problems. 7Nasser, Y. A. (2022, November 17). Pica. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK532242/
Pica vs. Rumination Disorder
As discussed above, pica is an eating disorder in which an individual eats non-food material for at least more than one month.
Rumination disorder is an eating or feeding disorder in which undigested food regurgitates back into the mouth and causes nausea, heartburn, difficulty swallowing, odynophagia or painful swallowing, and pain in the upper abdomen. People with rumination disorder continuously vomit, spit, re-chew, or re-swallow undigested food.
How to Diagnose Pica?
Doctors diagnose pica disorder by taking a detailed history and examination. They may ask you about your family history, socioeconomic status, personal history, environmental history, exposure history, duration of exposure, types of ingested substances, and signs of toxicology.
Most patients with pica present with signs of toxin ingestion. Sometimes, they may fall unconscious due to the toxicity of different chemicals. DSM-5 criterion is used to diagnose pica.
Diagnostic Criteria :
According to the DSM-5, the diagnostic criteria that support pica is :
- Eating non-food substances for more than one month of duration.
- Ingestion of these non-nutritive substances is inappropriate for the development of the patient.
- Ingestion of these non-foody materials is not a part of cultural tradition.
- If ingestion of these non-food substances occurs in a patient having another disorder, it requires urgent medical attention.
Physical Examination:
After taking a detailed history, your doctor will do a thorough physical examination to support his diagnosis. He will do a general physical examination and proceed toward each system of the body.8McNaughten B, Bourke T, Thompson A. Fifteen-minute consultation: the child with pica. Arch Dis Child Educ Pract Ed. 2017 Oct;102(5):226-229. Physical examination includes:
- Look for signs of toxic ingestion, such as a change in the color of fingers and lips, erosion on fingers and lips, discoloration of tongue and teeth, and mouth ulcers after chewing hard substances.
- Gastrointestinal manifestations to look out for intestinal obstruction. Hard and indigestible substances can obstruct or perforate the patient’s intestines, causing vomiting and abdominal pain.
- Dental manifestations like tooth abrasion, discoloration, and tooth loss.
Laboratory Investigation:
Pica disorder not only has physical manifestations but also disrupts electrolyte balance and levels of essential nutrients. High levels of toxins cause toxicity. The following laboratory investigations help with the diagnosis of pica syndrome:
- Complete blood profile
- Lead level
- Stool examination
- Zinc level
- Serum iron level
- Vitamins and mineral screening
Radiological Investigations:
Some radiological modalities are used to confirm your diagnosis. These include:
-
X-rays Abdomen
The X-ray abdomen is preferred when a patient has ingested hard or bony substances like pins, coins, small rods, and other miscellaneous things. The X-ray shows the structure and location of the ingested materials.
-
Abdominal Ultrasound
Abdominal ultrasound is necessary to detect obstruction and intestine perforation due to ingesting indigestible substances.
-
Upper Gastrointestinal Tract Endoscopy
Upper GI endoscopy is a diagnostic and therapeutic procedure. Doctors use it to extract foreign bodies, such as sharp objects, from the esophagus or stomach.
-
Barium Examination (Upper & Lower GI)
Barium meals help doctors see the exact location, shape, and size of ingested substances on X-ray. This procedure shows changes and abnormalities in the gastrointestinal tract. Doctors ask the patient to swallow a barium meal for an upper GI examination, and a barium enema helps with a lower GI examination.
-
CT-Abdomen
Abdominal and pelvic CT scans help locate foreign bodies. They also detect intestinal dilatation and obstruction caused by the ingestion of indigestible materials.
Treatment of Pica Disorder:
A multidisciplinary approach is the best treatment approach for pica disorder, and it involves a psychologist, a physician, and a social worker. Behavioral modification is the most effective method to treat pica disorder. It involves;
- Training the patient so they can discriminate between edible and non-edible things.
- Sensory reinforcement
- Reversal of the habit
- Use of self-protection devices
- Environmental modifications
There is no specific medical treatment for pica disorder; however, evidence suggests that dopaminergic agonists like olanzapine can effectively manage the condition.
Surgery is the treatment of choice in cases of intestinal obstruction or perforation. Surgeons remove foreign bodies and repair the damaged intestine using various techniques.
Additionally, other interventions are available to address the complications associated with pica disorder. Some of these interventions include:
- Treating nutritional deficiency
- Treating mineral and vitamin deficiency
- Iron and zinc supplements
- A healthy diet
- A good relationship with parents and family
- Good mental health
- Stress reduction techniques
Prevention of Pica Disorder
Although there is no way to prevent pica disorder, some preventive measures can help treat it. These are:
- Providing adequate nutrition
- Family education
- Avoiding stress
- Good parents-child relation
- Using Self-protection devices that prohibit children or adults with pica from placing non-edible substances in the mouth.
Conclusion
To conclude, pica is an eating disorder that compels a person to eat non-food and non-nutritive substances. It is a treatable medical problem that involves a multidisciplinary approach. Adequate nutrition, counseling, family education, stress reduction techniques, and healthy parenting help alleviate this problem. If your child or a loved one suffers from pica syndrome, consult your doctor immediately and provide good care to improve his mental health.
Refrences
- 1Young SL. Pica in pregnancy: new ideas about an old condition. Annu Rev Nutr. 2010 Aug 21;30:403-22.
- 2Burke, M., MD. (n.d.). Pica: Practice Essentials, Background, Etiology. https://emedicine.medscape.com/article/914765-overview#a5
- 3Singhi S, Singhi P, Adwani GB. Role of psychosocial stress in the cause of pica. Clin Pediatr (Phila). 1981 Dec;20(12):783-5.
- 4Nchito M, Geissler PW, Mubila L, Friis H, Olsen A. Effects of iron and multimicronutrient supplementation on geophagy: a two-by-two factorial study among Zambian schoolchildren in Lusaka. Trans R Soc Trop Med Hyg. 2004 Apr;98(4):218-27.
- 5Ezzeddin N, Zavoshy R, Noroozi M, Jahanihashemi H, Riseh SH. Prevalence and risk factors for pica during pregnancy in Tehran, Iran. Eat Weight Disord. 2015 Dec;20(4):457-63.
- 6Konlan KD, Abdulai JA, Konlan KD, Amoah RM, Doat AR. Practices of pica among pregnant women in a tertiary healthcare facility in Ghana. Nurs Open. 2020 Jan 28;7(3):783-792. doi: 10.1002/nop2.451. PMID: 32257266; PMCID: PMC7113508.
- 7Nasser, Y. A. (2022, November 17). Pica. StatPearls – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK532242/
- 8McNaughten B, Bourke T, Thompson A. Fifteen-minute consultation: the child with pica. Arch Dis Child Educ Pract Ed. 2017 Oct;102(5):226-229.