Hypercalcemia is a condition characterized by too much calcium in the bloodstream. It can cause bone weakening, kidney stones, and interference with heart and brain functions. In some cases, the symptoms may be non-existent. Hypercalcemia may appear as a secondary ailment along with hyperthyroidism and cancer. However, it is treatable with several medications and surgical procedures after consultations with healthcare experts.
What is Hypercalcemia?
Hypercalcemia occurs when you have more calcium levels in the blood than the normal range of 8.5 to 10.5mg/dl. However, it is important to know that this level is for adults, and in newborns, the normal calcium range is 9 to 11mg/dl and stays like this until the age of 5. Calcium is an important mineral that is present most prominently in bones and blood. Higher levels can lead to fatal health complications like kidney failure. Calcium is required for normal body functions. The most prominent role of calcium involves:
- Blood clotting
- Heart Pumping
- Muscle movement through squeezing
- Nerve transmission
Calcium levels increase from normal levels when two hormones, calcitonin and thyroid hormones, are abnormally functioning. These glands are located near the thyroid gland in the neck. Additionally, taking extra vitamin D and calcium supplements may elevate calcium levels.
Causes of Hypercalcemia
Hypercalcemia may be caused by a variety of factors including:
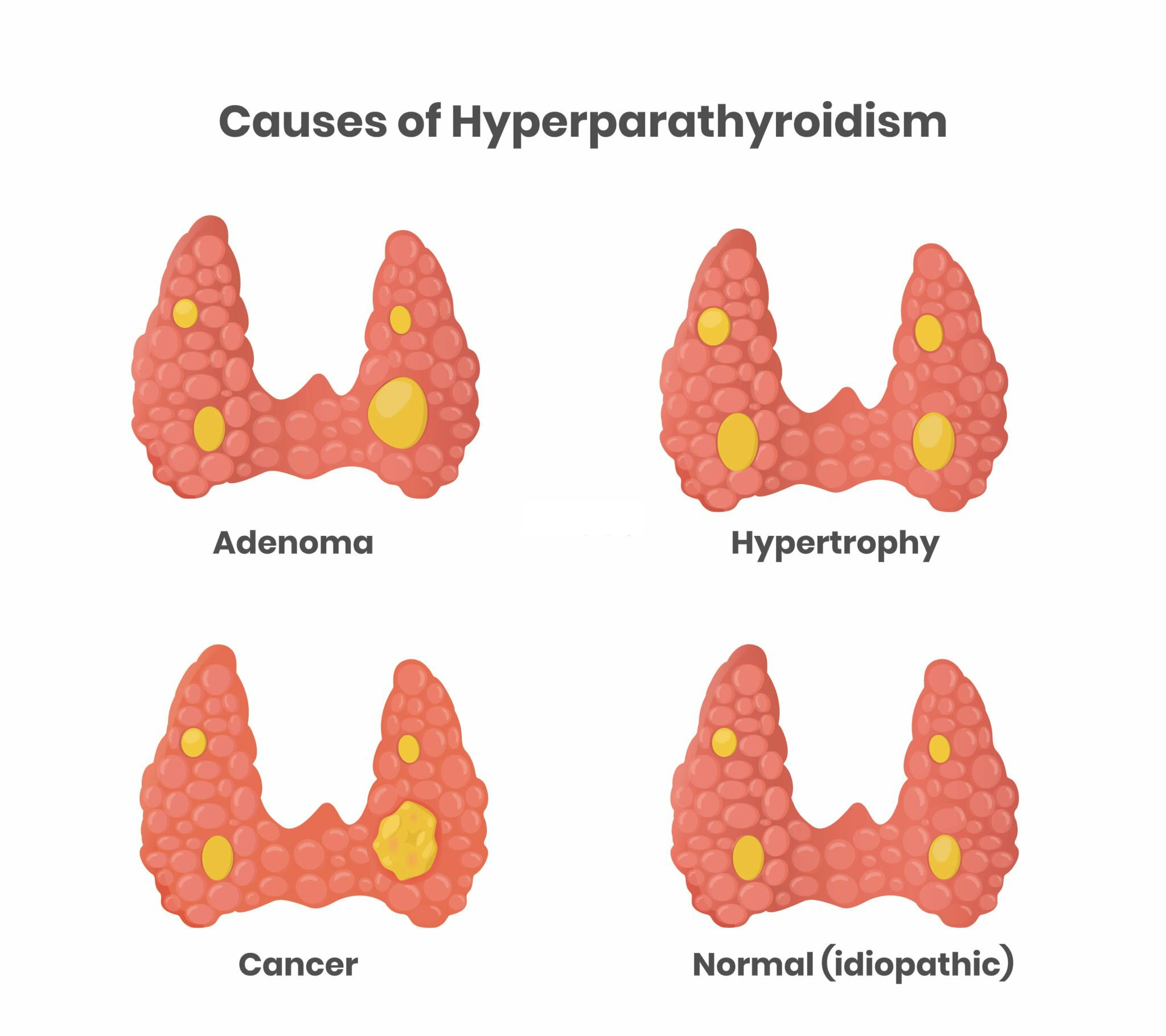
Hyperparathyroidism
Hyperactivity of parathyroid glands releases excessive PTH (parathyroid hormone), which draws calcium out of the bones by enhancing the activity of osteoclasts (bone-destroying cells). The most common condition leading to this parathyroid gland enlargement due to non-cancerous growths called adenomas.
Tumors
Tumors, including lung cancer, especially non-small cell lung cancer and blood cancer, can elevate the risk of hypercalcemia. Regarding the pathophysiology, malignancy-related hypercalcemia is mediated by three pathways: excessive release of PTH, increased osteoclastic activity, or enhanced calcitriol (vitamin D) production.1Vakiti, A., Anastasopoulou, C. and Mewawalla, P., 2018. Malignancy-related hypercalcemia. The following are the most common tumors leading to hypercalcemia:
- Breast cancer
- Cancer of the lymphatic system
- Rhabdomyosarcoma
- Multiple myeloma
Dehydration
Lower levels of fluids in the blood cause elevated calcium levels. As this reduces the volume of body fluids, leading to hypovolemia, the kidney’s ability to excrete calcium properly becomes compromised. It is important to note that severe dehydration only causes transient hypercalcemia.2Ojbindra, K.C., Dahal, P.H., Koirala, M. and Al Zaghal, E., 2022. Unusual Case of Dehydration Leading to Severe Symptomatic Hypercalcemia. The American Journal of Case Reports, 23, pp.e936204-1.
Congenital Conditions
Familial hypocalciuric hypercalcemia is a genetic condition where calcium-sensing receptor genes (CASR) are affected, resulting in reduced activity of the receptors. The symptoms include hypercalcemia along with low urine calcium, hyper-magnesia, and hypophosphatemia.3Afzal, M. and Kathuria, P., 2021. Familial hypocalciuric hypercalcemia. Treasure Island, FL: StatPearls Publishing.
Medications
Some drugs also cause hypercalcemia as a side effect. The most common example is the administration of lithium for the management of bipolar disorder. Other medications include:
- Hydrochlorothiazide diuretics
- Calcium carbonate
- Antacids
Limited Physical Activity
The health conditions that bind the patients to less physical activity develop hypercalcemia. The conditions demand lying or sitting longer, like post-stroke, paralysis, or fractures. As a result, bones release calcium in the blood due to extra stress.
Nutritional Supplement
The administration of nutritional supplements containing calcium, vitamin A, or vitamin D can lead to excessive calcium levels in the bloodstream.
Associated Diseases
Several other diseases, including sarcoidosis and tuberculosis, can elevate vitamin D levels. Vitamin D facilitates calcium absorption, triggering increased absorption from the digestive tract.
In around 43% of patients with multi-nodular goiter over 60 years of age, high thyroid levels resulted in hypercalcemia.4Kravchenko, V.I., Andrusyshyna, I.M., Luzanchuk, I.A., Polumbryk, M.O. and Tarashchenko, Y.M., 2020. Association between thyroid hormone status and trace elements in serum of patients with nodular goiter. Biological trace element research, 196(2), pp.393-399.
Hypercalcemia Symptoms
Higher calcium levels have different symptoms in all individuals. Sometimes, hypercalcemia may be asymptomatic, but the older population shows more aggressive symptoms as compared to young ones.5Sternlicht H, et al. (2015). Hypercalcemia of malignancy and new treatment options. https://doi.org/10.2147/TCRM.S83681 However, they may also vary depending on the underlying cause and duration of the ongoing condition. As hypercalcemia affects all body systems, the most common targets are the central nervous system, gastrointestinal functions, and cardiac system. So, hypercalcemia symptoms include:
- Central Nervous system: Confusion, fatigue, muscle weakness, and ultimately comma.
- Gastrointestinal effects: Pancreatitis, stomach aches, peptic ulcers, nausea, constipation, anorexia, and decreased appetite.
- Renal Effects: Renal stones, nocturia, chronic kidney disease, polyurea, dehydration, acute kidney injury, or nephrogenic diabetes insipidus.
- Cardiac effects: Bradycardia, arrhythmia, short QT intervals, and hypertension.
Moreover, hypercalcemia symptoms may also manifest as muscle weakness, cramps, and aching.

Diagnosis of Hypercalcemia
Since hypercalcemia often shows fewer symptoms, it is diagnosed through lab blood tests. These tests help to identify the calcium levels in the blood. The most commonly recommended tests are:
- Serum calcium
- Serum vitamin D levels
- Serum PTH
- Urine calcium
- Serum PTH-related proteins
The above-mentioned blood tests diagnose hypercalcemia on three levels of calcium crisis: mild (10.5-11.9 mg/dL), moderate (12.0-13.9 mg/dL), or severe (14.0-16.0 mg/dL). However, among these conditions, the hypercalcemic crisis (severe hypercalcemia) is considered an emergency to be treated and managed immediately.6Gill, G., Agrawal, V. and Kerr, P., 2023. Primary hyperparathyroidism presenting as acute hypercalcemic crisis: a case report. Journal of Otolaryngology-Head & Neck Surgery, 52(1), pp.1-8.
Although blood tests are the first line, if hypercalcemia is associated with other diseases like sarcoidosis, healthcare providers can ask for imaging tests to visualize tumors and lesions. The following tests are usually ordered:
- Mammogram: These are X-ray images of breasts and can be used in breast cancer-induced hypercalcemia.
- Chest X-rays: These are used to visualize lung cancer, usually as coin lesions.
- Computed Tomography Scans: They are advanced scans typically performed on suspected cases of sarcoidosis, showing hilar and mediastinal lymphadenopathy (lymph node enlargement).
Additionally, other possible causes can be diagnosed by complete physical evaluation and past medical history. Those who have excessive parathyroid hormone production are then recommended to visit an endocrinologist for an accurate diagnosis. Moreover, evaluation of serum chloride, phosphate levels, alkaline phosphatase, and alkaline phosphatase can also be helpful.
Hypercalcemia vs Hypocalcemia
Hypercalcemia and hypocalcemia are both related to the calcium levels in the body, and the main difference lies in the quantity of calcium. While hypercalcemia means high calcium, the prefix ‘’hypo’’ defines ‘’low’’ levels. This means hypocalcemia is the lower levels of calcium in the body. Hypocalcemia presents with the following symptoms:7Pepe, J., Colangelo, L., Biamonte, F., Sonato, C., Danese, V.C., Cecchetti, V., Occhiuto, M., Piazzolla, V., De Martino, V., Ferrone, F. and Minisola, S., 2020. Diagnosis and management of hypocalcemia. Endocrine, 69, pp.485-495.
- Muscle cramps
- Paresthesias
- Myoclonic jerks
- Severe hypocalcemia symptoms include
- Laryngospasm
- Tetany
- Apnea
- Hypotension
- Seizures
- Osteoporosis
- Changes in brain functions
Additionally, if the hypocalcemic condition lasts longer, it may manifest several skin indications, including dry and coarse skin, brittle nails, eczematous dermatitis, and dental hypoplasia.
The two most prominent signs of hypocalcemia are diagnosed during physical examination, including Chvostek symptoms and Trousseau signs. These findings identify the facial muscle contractions and carpopedal compressions.
Treatments revolve around the use of high-calcium diets and supplements to restore calcium.
How is Hypercalcemia Treated?
The treatment approach aims to reduce calcium levels and eliminate symptoms. However, calcium levels in the blood decide the severity of the condition, whether it is mild or severe.
If your symptoms are mild, healthcare experts might try to monitor the health of bones and kidneys. Whereas, in severe hypercalcemia, the doctors undergo surgical procedures or certain medications as follows:
Medications:
Your doctor might prescribe the following:
Steroids
You might be administered steroids to decrease calcium levels. These steroids are inserted through an intravenous route or orally in tablet forms. They remove excessive calcium by increasing the excretion via the kidneys and reducing the absorption in the gut. 8Cohen, M., Sanchez, J., Toft, D.J., Eisenberg, Y. and Kukreja, S.C., 2021.Prednisone-Responsive Hypercalcemia in a Patient With IgG4 Disease and Elevated Serum PTHrP Levels. Journal of the Endocrine Society, 5(Supplement_1), pp.A212-A213.
Prednisolone
Prednisolone is a steroid hormone that helps regulate excess vitamin D levels. These pills have helped the short-term management of hypercalcemia due to vitamin D levels.
Calcitonin (Miacalcin)
Calcitonin, a hormone, regulates calcium levels in the body. It is obtained synthetically from salmon. Another benefit associated with calcitonin is the prevention of bones from breakage. However, it is administered intravenously, and the dose ranges from 3 to 4 times daily. The dosage selection depends on the calcium levels present in the blood and its efficacy.9Malick, Alyyah, Ananya Kondapalli, and Salila Kurra. “Non-parathyroid Hormone–Mediated Endocrine Causes of Hypercalcemia.” In Hypercalcemia, 223–36. Cham: Springer International Publishing, 2022. http://dx.doi.org/10.1007/978-3-030-93182-7_15.
Denosumab
Denosumab is a monoclonal antibody categorized among the targeted therapeutic approaches. This drug is administered to individuals who have cancer associated with hypercalcemia. The main function of denosumab is to prevent bone structure from fractures and breakage. Healthcare providers recommend denosumab to patients who are unresponsive to bisphosphonates.10Eremkina, A., Krupinova, J., Dobreva, E., Gorbacheva, A., Bibik, E., Samsonova, M., Ajnetdinova, A. and Mokrysheva, N., 2020. Denosumab for management of severe hypercalcemia in primary hyperparathyroidism. Endocrine Connections, 9(10), pp.1019-1027.
Calcimimetics
Calcimimetics have proven to be effective in managing parathyroid-related hypercalcemia. They reduce the overactivation of parathyroid hormones, which facilitates the management of hypercalcemia.
Bisphosphonates
Hypercalcemia due to cancer is treated by intravenous administration of bisphosphonates. Often used for osteoporotic bones, bisphosphonates help lower calcium levels quickly.11Wu JX, Yeh MW. Asymptomatic primary hyperparathyroidism. Diagnostic pitfalls and surgical intervention. Surg Oncol Clin North Am. 2016; 25: 77-90. This medication reduces pain and protects bones from deteriorating.
Loop Diuretics
Doctors may use loop diuretics in the emergency management of hypercalcemia. Only loop diuretics, e.g., furosemide, are used as they block the sodium-potassium-chloride transporter and cause extra calcium excretion in the urine.
Other Medications
Besides the above-mentioned medications, some individuals may remain unresponsive. For the treatment of resistant hypercalcemia, doctors might consider the following:
- Lithium
- Medication for acid reflux
Therefore, the treatment approaches vary among individuals. In some individuals, treatment eliminates symptoms of hypercalcemia quickly compared to others.
Fluid Replacement
Regarding hypercalcemic emergencies, starting patients on a bolus infusion of isotonic saline is advisable.
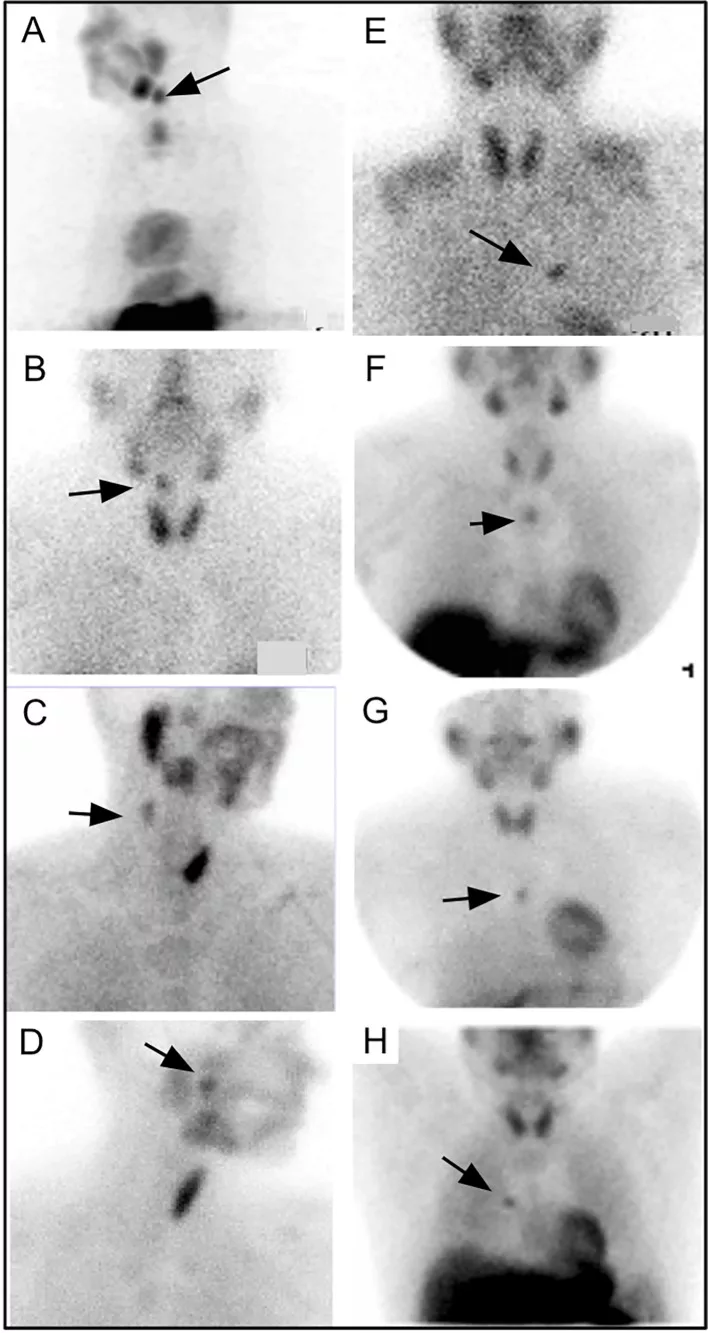
Surgical Management
Surgical procedures are mandatory for individuals who have abnormal functioning of parathyroid hormones or the growth of tumors. Firstly, a customized screening test called parathyroid scintigraphy involves radioactive material injection.12Carrelli, Angela L. “Rare and Other Causes of Hypercalcemia.” In Hypercalcemia, 237–45. Cham: Springer International Publishing, 2022. http://dx.doi.org/10.1007/978-3-030-93182-7_16.
This helps to localize the tumor in the parathyroid gland. Secondly, parathyroidectomy, a minimally invasive procedure, helps remove the tumor.
Complications associated with Hypercalcemia
If you are someone experiencing hypercalcemia for a longer period, there are rare chances of any associated complications, and these are mainly in resistant cases.13Omotosho, Y.B. and Zahra, F., 2021. Resistant hypercalcemia. Despite this, the most common complications that one may observe due to higher calcium levels are:
- Depression
- Osteoporosis
- Kidney failure
- Nephrocalcinosis leading to poor kidney functions
- Hypertension
- Bone cysts
- Bone fractures
Is Hypercalcemia Preventable?
Yes, it is preventable through lifestyle modifications. These may include decreased intake of calcium components in diet and medications like antacids and other supplements.14Feingold KR, et al, eds. Approach to hypercalcemia. In: Anatomy and Ultrastructure of bone – Histogenesis, growth, and remodeling. MDText.com. 2019. https://www.ncbi.nlm.nih.gov/books/NBK279129/. Moreover, you should always consult your doctor before starting any self-medication. Following are additional preventive measures that reduce the chances of hypercalcemia:
- Drinking adequate water
- Avoiding alcohol and smoking
- Resistant and strength training exercises
When should I go to the Healthcare Expert?
You should visit your nearest healthcare provider if you notice any new symptoms, particularly muscle weakness, cramps, or mainly urine-associated symptoms, especially after starting any medication or supplement.
It is important to note that if you notice any mass or enlargements around the neck, you should immediately consult the nearest health center. However, patients with a diagnosis of hypercalcemia need regular follow-up sessions.
Conclusion
Hypercalcemia, as the name suggests, is more calcium. Although hypercalcemia has many causes, including supplements, cancers, medications, and much more, parathyroid enlargement remains the most common one. While most cases are silent, severe hypercalcemia is a medical emergency and needs prompt treatment.
Refrences
- 1Vakiti, A., Anastasopoulou, C. and Mewawalla, P., 2018. Malignancy-related hypercalcemia.
- 2Ojbindra, K.C., Dahal, P.H., Koirala, M. and Al Zaghal, E., 2022. Unusual Case of Dehydration Leading to Severe Symptomatic Hypercalcemia. The American Journal of Case Reports, 23, pp.e936204-1.
- 3Afzal, M. and Kathuria, P., 2021. Familial hypocalciuric hypercalcemia. Treasure Island, FL: StatPearls Publishing.
- 4Kravchenko, V.I., Andrusyshyna, I.M., Luzanchuk, I.A., Polumbryk, M.O. and Tarashchenko, Y.M., 2020. Association between thyroid hormone status and trace elements in serum of patients with nodular goiter. Biological trace element research, 196(2), pp.393-399.
- 5Sternlicht H, et al. (2015). Hypercalcemia of malignancy and new treatment options. https://doi.org/10.2147/TCRM.S83681
- 6Gill, G., Agrawal, V. and Kerr, P., 2023. Primary hyperparathyroidism presenting as acute hypercalcemic crisis: a case report. Journal of Otolaryngology-Head & Neck Surgery, 52(1), pp.1-8.
- 7Pepe, J., Colangelo, L., Biamonte, F., Sonato, C., Danese, V.C., Cecchetti, V., Occhiuto, M., Piazzolla, V., De Martino, V., Ferrone, F. and Minisola, S., 2020. Diagnosis and management of hypocalcemia. Endocrine, 69, pp.485-495.
- 8Cohen, M., Sanchez, J., Toft, D.J., Eisenberg, Y. and Kukreja, S.C., 2021.Prednisone-Responsive Hypercalcemia in a Patient With IgG4 Disease and Elevated Serum PTHrP Levels. Journal of the Endocrine Society, 5(Supplement_1), pp.A212-A213.
- 9Malick, Alyyah, Ananya Kondapalli, and Salila Kurra. “Non-parathyroid Hormone–Mediated Endocrine Causes of Hypercalcemia.” In Hypercalcemia, 223–36. Cham: Springer International Publishing, 2022. http://dx.doi.org/10.1007/978-3-030-93182-7_15.
- 10Eremkina, A., Krupinova, J., Dobreva, E., Gorbacheva, A., Bibik, E., Samsonova, M., Ajnetdinova, A. and Mokrysheva, N., 2020. Denosumab for management of severe hypercalcemia in primary hyperparathyroidism. Endocrine Connections, 9(10), pp.1019-1027.
- 11Wu JX, Yeh MW. Asymptomatic primary hyperparathyroidism. Diagnostic pitfalls and surgical intervention. Surg Oncol Clin North Am. 2016; 25: 77-90.
- 12Carrelli, Angela L. “Rare and Other Causes of Hypercalcemia.” In Hypercalcemia, 237–45. Cham: Springer International Publishing, 2022. http://dx.doi.org/10.1007/978-3-030-93182-7_16.
- 13Omotosho, Y.B. and Zahra, F., 2021. Resistant hypercalcemia.
- 14Feingold KR, et al, eds. Approach to hypercalcemia. In: Anatomy and Ultrastructure of bone – Histogenesis, growth, and remodeling. MDText.com. 2019. https://www.ncbi.nlm.nih.gov/books/NBK279129/.





