Pickwickian syndrome, also known as Obesity hypoventilation syndrome (OHS), is a breathing disorder that develops in some obese people. The syndromic disorder is characterized by low oxygen (hypoxia) and high carbon dioxide (hypercapnia) levels in the body. The imbalance of blood gases is attributed to sub-optimal (slow) breathing rates in obese individuals, which lead to hypoventilation. The excess carbon dioxide and oxygen deficit cause breathing difficulties, fatigue, and impaired concentration, etc. It is an underdiagnosed disorder, with an estimated prevalence of 0.15-0.30% in the general population and 10-20% in obese individuals.1Chau, E. H., Lam, D., Wong, J., Mokhlesi, B., & Chung, F. (2012). Obesity hypoventilation syndrome: a review of epidemiology, pathophysiology, and perioperative considerations. Anesthesiology, 117(1), 188-205.
The majority of OHS patients also suffer from obstructive sleep apnea (OSA). The hypoventilation syndrome can lead to serious, life-threatening complications, therefore, treatment is necessary. Doctors manage it with breathing assistance (like CPAP) and weight-loss programs (lifestyle modifications, bariatric surgery, etc.).
Pickwickian Syndrome Symptoms
The most common symptoms of the syndromic disorder include:
Breathing Difficulties:
Patients experience sleep-disordered breathing, which consequently leads to other symptoms like daytime sleepiness. Obstructive sleep apnea (OSA) is a type of sleeping disorder frequently present in such patients. In the majority of OSA cases, partners of patients notice snoring and night awakenings with typical gasping for air.2Kaw, R., Wong, J., & Mokhlesi, B. (2021). Obesity and obesity hypoventilation, sleep hypoventilation, and postoperative respiratory failure. Anesthesia & Analgesia, 132(5), 1265-1273. However, in addition to OSA, OHS patients also experience awake diurnal hypercapnia (elevated levels of carbon dioxide during the day). The raised levels of carbon dioxide during the day compromise breathing and directly affect work performance.
If severe breathing compromises continue, you may notice the development of serious symptoms like chest pain, swelling of the foot/ankle region, cyanosis, etc. Immediately visit the ER if you experience any such symptoms!
Fatigue & Tiredness:
Several individuals with sleep-disordered breathing suffer from tiredness and constant fatigue. There have been reported cases of elderly men reporting fatigue and somnolence after progressively gaining weight.3Shah, N. M., Shrimanker, S., & Kaltsakas, G. (2021). Defining obesity hypoventilation syndrome. Breathe, 17(3). Sometimes, episodes of dizziness may also accompany daytime fatigue.
Lack Of Energy & Daytime Sluggishness:
Lack of proper sleep causes daytime drowsiness, seriously affecting your work performance. This, paired with a generalized lack of energy, significantly reduces productivity and may even cause a bad mood.
Headache:
A large number of patients with OHS report morning headaches. A 67-year-old male with a BMI above 37 kg/m presenting with progressive breathlessness and morning headaches was diagnosed with obesity hypoventilation syndrome.4Prabhudesai, P. (2019). Obesity Hypoventilation Syndrome. International Journal of Head and Neck Surgery, 10(2), 39-41. Even children with severe obesity and daytime hypoventilation suffer from morning headaches, cognitive deficits, and signs of cor pulmonale.5Wang, G., Guevarra, J., & Bronstein, J. (2020). 1217 Obesity hypoventilation syndrome in a 4-year-old child. Sleep, 43(Supplement_1), A465-A465.
Cognitive & Memory Impairments:
Pickwickian syndrome can have a direct impact on neurocognitive abilities and memory in patients. Persistent hypercapnia can impair cognitive abilities. In a study, OHS patients showed increased reaction times, poor cognitive function assessments, and deficits in logical memory. The slow processing speed of individuals was attributed to hypercapnia. Some patients may also fall prey to depression.6Kung, S. C., Shen, Y. C., Chang, E. T., Hong, Y. L., & Wang, L. Y. (2018). Hypercapnia impaired cognitive and memory functions in obese patients with obstructive sleep apnoea. Scientific reports, 8(1), 17551.
Pickwickian Syndrome Causes
The exact cause of Pickwickian is unknown. However, experts believe the main underlying cause of the disorder is a reduction in the capacity of the respiratory system. This ultimately leads to poor processing of carbon dioxide, causing its buildup in the body. Multiple factors that contribute to compromises in ventilation include:
- Adipose tissues: Deposition of extra fat around the neck and chest makes breathing harder and thus, a challenge for the respiratory system to exchange gases efficiently.
- Hormonal imbalance: The excess fat cells (especially abdominal fat cells) produce the leptin hormone. Elevated levels of this hormone can interfere with normal patterns of breathing, thereby contributing to hypoventilation.7Gauda, E. B., Conde, S., Bassi, M., Zoccal, D. B., Almeida Colombari, D. S., Colombari, E., & Despotovic, N. (2020). Leptin: master regulator of biological functions that affects breathing. Comprehensive Physiology, 10(3), 1047-1083.
- Brain defect: Sometimes, a defect causes the brain to lose control of your breathing. The exact defect causing this is not known, but it surely involves the region responsible for controlling breathing.
Risk Factors:
Males have a greater tendency to develop this obesity disorder than females. Additionally, researchers have also found a higher prevalence of Pickwickian syndrome in black people.
Pickwickian Syndrome Diagnosis
Though Pickwickian disease is a rare disorder, it is fairly common in obese people. Therefore, clinicians suspect the case if an obese patient presents with disordered breathing.
The first step in diagnosis is quantifying the patient’s obesity. Body mass index (BMI) is a scale to measure body fat and is calculated by measuring body weight and height. People having a BMI of 30 or higher are obese. Generally, individuals suffering from OHS are very obese and have a BMI of above 35.8Ghimire, P., Sankari, A., & Kaul, P. (2024). Pickwickian syndrome. In StatPearls [Internet]. StatPearls Publishing.
If your BMI is high, your doctor will perform a physical examination to check the cause of the ventilation issue. Another important test is the arterial blood gas test. In case of suspected OHS, the test checks the arterial carbon dioxide tension, i.e., a measurement of carbon dioxide in your blood.
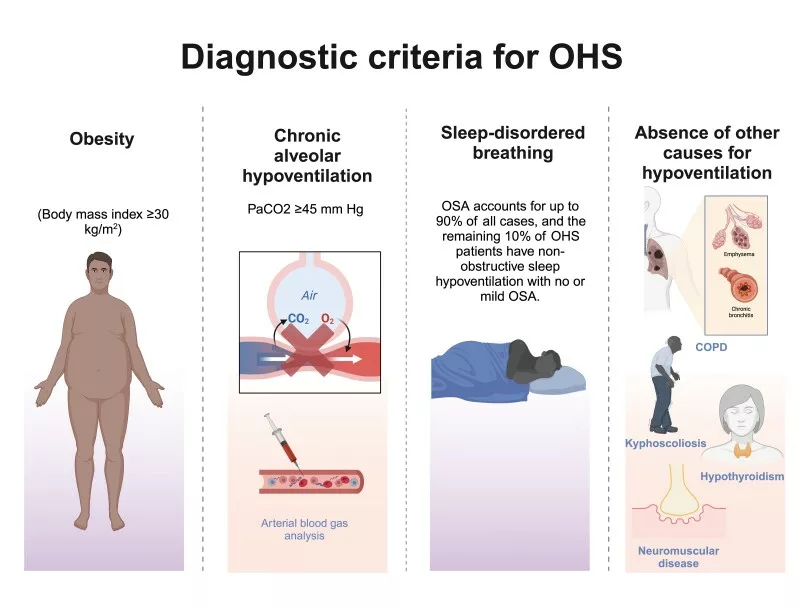
Diagnostic Criteria:
Doctors diagnose it as OHS if:
- Arterial carbon dioxide tension is greater than 45mm Hg while awake
- BMI is 30 or higher (obesity)
- Hypoventilation is present and is not linked to any other underlying cause
Other tests/imaging that your doctor may order include:
- Pulmonary function test: This tests the lungs’ performance to rule out any other causes of pulmonary distress.
- Electrocardiogram/Echocardiogram: ECG and echo tests reveal the performance of the heart. These tests aid in ruling out heart pathologies as the cause of hypoventilation.
- Oxygen saturation: Modern healthcare providers use a pulse oximeter to measure oxygen saturation to get an idea of hypoxemia.
- Chest X-rays: Lung function and chest X-rays are done in conjunction to rule out other possible causes of hypoventilation.
- Sleep study (polysomnography): This helps in understanding the severity of sleep apnea.
Differential Diagnosis:
Pickwickian Syndrome Vs Chronic Obstructive Pulmonary Disorder (COPD)
Obesity hypoventilation syndrome is often misdiagnosed as COPD due to the similarities. However, there are some evident differences too. OHS is characterized by hypoventilation in obese individuals with evident hypercapnia. On the other hand, COPD is a progressive respiratory disease that is usually linked to smoking. COPD patients suffer from shortness of breath accompanied by wheezing and coughing. No such symptoms are seen in OHS.
Pickwickian Syndrome Treatment
The main aim of the treatment is to enhance ventilation (and breathing) and improve your quality of life. The following treatment modalities are most commonly employed to manage Pickwickian syndrome.
Breathing Assistance: Positive Airway Pressure (PAP) Therapy
The first-line treatment for OHS is PAP. Doctors generally advise patients to use a Continuous positive airway pressure (CPAP) machine while sleeping. It is a specialized machine that continuously provides pressurized air from a motor to your mouth via a nose/mouth mask. Another machine called the Bilevel positive airway pressure (BiPAP) delivers pressurized air only when you inhale. Most patients use CPAP and BiPAP machines during sleep to improve apnea. Medical study reviews find CPAP to be an effective and affordable solution for OHS patients.9Soghier, I., Brożek, J. L., Afshar, M., Kakazu, M. T., Wilson, K. C., Masa, J. F., & Mokhlesi, B. (2019). Noninvasive ventilation versus CPAP as initial treatment of obesity hypoventilation syndrome. Annals of the American Thoracic Society, 16(10), 1295-1303.

This therapy greatly helps patients with nighttime sleep and consequently alleviates symptoms of daytime drowsiness and fatigue. Another study pointed out that 3 months of PAP therapy leads to better sleep quality, improved cognitive function, and enhanced quality of life. 10Zheng, Y., Yee, B. J., Wong, K., Grunstein, R. R., & Piper, A. J. (2024). A comparison of two obesity-related hypoventilation disorders: Impact on sleep, quality of life and neurocognitive outcomes and the effects of positive airway pressure therapy. Sleep Advances, 5(1), zpae016. Many experts believe switching to non-invasive ventilation (CPAP or BiPAP) for OHS to be a feasible step. 11Arellano‐Maric, M. P., Hamm, C., Duiverman, M. L., Schwarz, S., Callegari, J., Storre, J. H., … & Windisch, W. (2020). Obesity hypoventilation syndrome treated with non‐invasive ventilation: Is a switch to CPAP therapy feasible?. Respirology, 25(4), 435-442.
In rare circumstances, when PAP doesn’t work, doctors may use a ventilator machine (which works like human lungs in exchanging gases) or opt for surgical procedures like tracheostomy to ensure optimal breathing. Tracheostomy is a procedure in which the surgeon creates a hole in your neck and exposes the windpipe (trachea) so you can breathe. Afterwards, a tube is placed to ensure that it keeps the created hole open and safe.
Weight & Fat Loss:
In the long-term management of the condition, your doctor will advise you to lose weight. You can cut away your body fat by making simple tweaks to your lifestyle. Avoiding refined sugars, shifting to a Mediterranean diet, and exercising regularly can help shed excess weight.
Bariatric Surgery
In cases of severe obesity, doctors go for bariatric surgery to reduce weight. There are different types of procedures that a surgeon can opt for. However, the most commonly performed procedures include gastric bypass and laparoscopic gastric banding.
In Roux-en-Y gastric bypass, the surgeon creates a small pouch in the stomach that connects to the small intestine. This bypasses the main gastrointestinal system and reduces the size of your working stomach to the equivalent of a walnut. In laparoscopic gastric banding (LABG), the surgeon places an adjustable band around the upper part of the stomach, which leads to the creation of a small pouch. Both these procedures reduce the capacity of your stomach and aid in losing weight.
Pickwickian Syndrome Life Expectancy
Treatment alleviates symptoms and significantly improves your quality of life. On the other hand, untreated OHS is reported to have high mortality and morbidity rates. In one study, the average mortality rate at the end of 18 months without treatment was 23%.12Nowbar, S., Burkart, K. M., Gonzales, R., Fedorowicz, A., Gozansky, W. S., Gaudio, J. C., … & Zwillich, C. W. (2004). Obesity-associated hypoventilation in hospitalized patients: prevalence, effects, and outcome. The American journal of medicine, 116(1), 1-7. Pickwickian syndrome life expectancy can improve, and the mortality rate drops to 3% (after 18 months) with timely non-invasive ventilation (NIV).
Pickwickian Syndrome Complications
Obese people with breathing difficulties are prone to falling prey to multiple complications. Pickwickian syndrome is frequently associated with complications like:
- Pulmonary hypertension: High blood pressure in arteries of the lungs (and ride side of the heart) is pretty common in OHS patients and has a prevalence of around 70%.13Almeneessier, A. S., Nashwan, S. Z., Al-Shamiri, M. Q., Pandi-Perumal, S. R., & BaHammam, A. S. (2017). The prevalence of pulmonary hypertension in patients with obesity hypoventilation syndrome: a prospective observational study. Journal of Thoracic Disease, 9(3), 779.
- Cor pulmonale: There is enlargement (and consequent failure) of the right ventricle. This mostly occurs due to OHS-induced pulmonary hypertension.
- Respiratory failure: Severe, long-standing hypoventilation eventually leads to respiratory failure.
- Secondary polycythemia: Pickwickian syndrome is linked to the development of abnormally high red blood cell count in the blood, which increases the risk of blood clots.14Wang, Y. Y., & Han, F. (2015). Polycythemia, ablepsia, and obesity hypoventilation syndrome: a case report. Chinese Medical Journal, 128(20), 2815-2817.
How Can I Prevent Pickwickian Syndrome?
You can reduce the risk of Pickwickian syndrome by maintaining a healthy weight. You should immediately report to the doctor about your breathing issues if you are obese. Timely treatment helps prevent aggravation of the disease and keeps you safe from complications.
Final Word
Pickwickian syndrome, or Obesity hypoventilation syndrome (OHS), is a respiratory disorder in which patients suffer from poor ventilation due to excess fat deposition. Obese individuals have sleep-disordered breathing, which is characterized by daytime hypercapnia (high carbon dioxide) and hypoxia (low oxygen levels). This gaseous imbalance leads to sleep apnea, morning headaches, and daytime sluggishness etc. Clinicians diagnose it using BMI, an arterial blood gas test, and sleep studies. The first line of treatment is breathing assistance with CPAP, BiPAP. Doctors advise weight loss and opt for surgeries like gastric bypass in cases where weight loss by lifestyle changes isn’t possible. Untreated OHS is linked to serious complications like pulmonary hypertension, cor pulmonale, and has a high mortality rate. Therefore, timely diagnosis and treatment are crucial.
Refrences
- 1Chau, E. H., Lam, D., Wong, J., Mokhlesi, B., & Chung, F. (2012). Obesity hypoventilation syndrome: a review of epidemiology, pathophysiology, and perioperative considerations. Anesthesiology, 117(1), 188-205.
- 2Kaw, R., Wong, J., & Mokhlesi, B. (2021). Obesity and obesity hypoventilation, sleep hypoventilation, and postoperative respiratory failure. Anesthesia & Analgesia, 132(5), 1265-1273.
- 3Shah, N. M., Shrimanker, S., & Kaltsakas, G. (2021). Defining obesity hypoventilation syndrome. Breathe, 17(3).
- 4Prabhudesai, P. (2019). Obesity Hypoventilation Syndrome. International Journal of Head and Neck Surgery, 10(2), 39-41.
- 5Wang, G., Guevarra, J., & Bronstein, J. (2020). 1217 Obesity hypoventilation syndrome in a 4-year-old child. Sleep, 43(Supplement_1), A465-A465.
- 6Kung, S. C., Shen, Y. C., Chang, E. T., Hong, Y. L., & Wang, L. Y. (2018). Hypercapnia impaired cognitive and memory functions in obese patients with obstructive sleep apnoea. Scientific reports, 8(1), 17551.
- 7Gauda, E. B., Conde, S., Bassi, M., Zoccal, D. B., Almeida Colombari, D. S., Colombari, E., & Despotovic, N. (2020). Leptin: master regulator of biological functions that affects breathing. Comprehensive Physiology, 10(3), 1047-1083.
- 8Ghimire, P., Sankari, A., & Kaul, P. (2024). Pickwickian syndrome. In StatPearls [Internet]. StatPearls Publishing.
- 9Soghier, I., Brożek, J. L., Afshar, M., Kakazu, M. T., Wilson, K. C., Masa, J. F., & Mokhlesi, B. (2019). Noninvasive ventilation versus CPAP as initial treatment of obesity hypoventilation syndrome. Annals of the American Thoracic Society, 16(10), 1295-1303.
- 10Zheng, Y., Yee, B. J., Wong, K., Grunstein, R. R., & Piper, A. J. (2024). A comparison of two obesity-related hypoventilation disorders: Impact on sleep, quality of life and neurocognitive outcomes and the effects of positive airway pressure therapy. Sleep Advances, 5(1), zpae016.
- 11Arellano‐Maric, M. P., Hamm, C., Duiverman, M. L., Schwarz, S., Callegari, J., Storre, J. H., … & Windisch, W. (2020). Obesity hypoventilation syndrome treated with non‐invasive ventilation: Is a switch to CPAP therapy feasible?. Respirology, 25(4), 435-442.
- 12Nowbar, S., Burkart, K. M., Gonzales, R., Fedorowicz, A., Gozansky, W. S., Gaudio, J. C., … & Zwillich, C. W. (2004). Obesity-associated hypoventilation in hospitalized patients: prevalence, effects, and outcome. The American journal of medicine, 116(1), 1-7.
- 13Almeneessier, A. S., Nashwan, S. Z., Al-Shamiri, M. Q., Pandi-Perumal, S. R., & BaHammam, A. S. (2017). The prevalence of pulmonary hypertension in patients with obesity hypoventilation syndrome: a prospective observational study. Journal of Thoracic Disease, 9(3), 779.
- 14Wang, Y. Y., & Han, F. (2015). Polycythemia, ablepsia, and obesity hypoventilation syndrome: a case report. Chinese Medical Journal, 128(20), 2815-2817.





