Placenta previa is an obstetrical complication where the placenta completely or partially covers the cervix, resulting in vaginal bleeding. Normally, the placenta is far away from the internal Os, but in this condition, it reaches or sometimes crosses the internal Os, resulting in bleeding and complications for the fetus and mother. Advanced imaging through ultrasound helps diagnose the location of the placenta and helps manage the condition. About 0.3% to 2% of females have this condition in the second half of pregnancy.1Anderson-Bagga, F.M. (2023) Placenta previa, StatPearls [Internet]. Retrieved 17 February 2024 https://www.ncbi.nlm.nih.gov/books/NBK539818/#article-27262.r6
What Is Placenta Previa?
Placenta previa is a condition where the placenta develops on the lower side of the uterus, partially or completely blocking the cervix, usually during the second half of pregnancy. The cervix, the lower end of the uterus, expands during delivery to allow the baby to pass out of the womb. However, when the cervix is obstructed by the placenta, vaginal delivery can result in excessive blood loss. Placenta previa commonly presents as painless vaginal bleeding, but it can lead to serious complications. The diagnosis is made using ultrasound. Patients who experience vaginal bleeding after 20 weeks of gestation should be evaluated for this condition.
The placenta is a sac-like organ that forms and expands during pregnancy to fulfill the nutrient and oxygen demands of the developing fetus. It usually forms on the lower side of the uterus but generally shifts to the top by the third trimester. This helps give the baby a passage to leave the womb during delivery.
Symptoms
Common clinical manifestations are:
- Bright red bleeding, with variable frequency, from the vagina in the last half of pregnancy. Bleeding is severe and might be fatal.
- Cramping in the abdomen
- Contractions in the back and lower belly
- Lightheadedness/Syncope

Causes & Risk Factors
Although the principal cause of this condition is unknown, it is found to have some association with scarring of the uterus and endometrial damage.2RM; S. (2015) Abnormal placentation: Placenta previa, vasa previa, and placenta accreta, Obstetrics, and Gynecology. Retrieved 13 February 2024 https://pubmed.ncbi.nlm.nih.gov/26244528/ However, some risk factors might contribute to the disease. Common risk factors are linked to age, lifestyle, and past medical history of the mother. Some risk factors associated with the development of this condition are:
- Using cocaine
- Smoking cigarettes
- Abnormally shaped uterus
- Maternal age of 35 years or more
- Twin pregnancy
- Any surgical procedure on the uterus, either caesarian section (C-section) or D&C
- Multiparity
- History of uterine fibroids (leiomyomas)
- Prior use of suction
- Assisted reproductive technology
- Prior placenta previa3CV, F.A. (2009) Etiology and risk factors for PLACENTA PREVIA: An overview and meta-analysis of observational studies, The journal of maternal-fetal & neonatal medicine : the official journal of the European Association of Perinatal Medicine, the Federation of Asia and Oceania Perinatal Societies, the International Society of Perinatal Obstetricians. Retrieved 17 February 2024 https://pubmed.ncbi.nlm.nih.gov/12820840/?dopt=Abstract
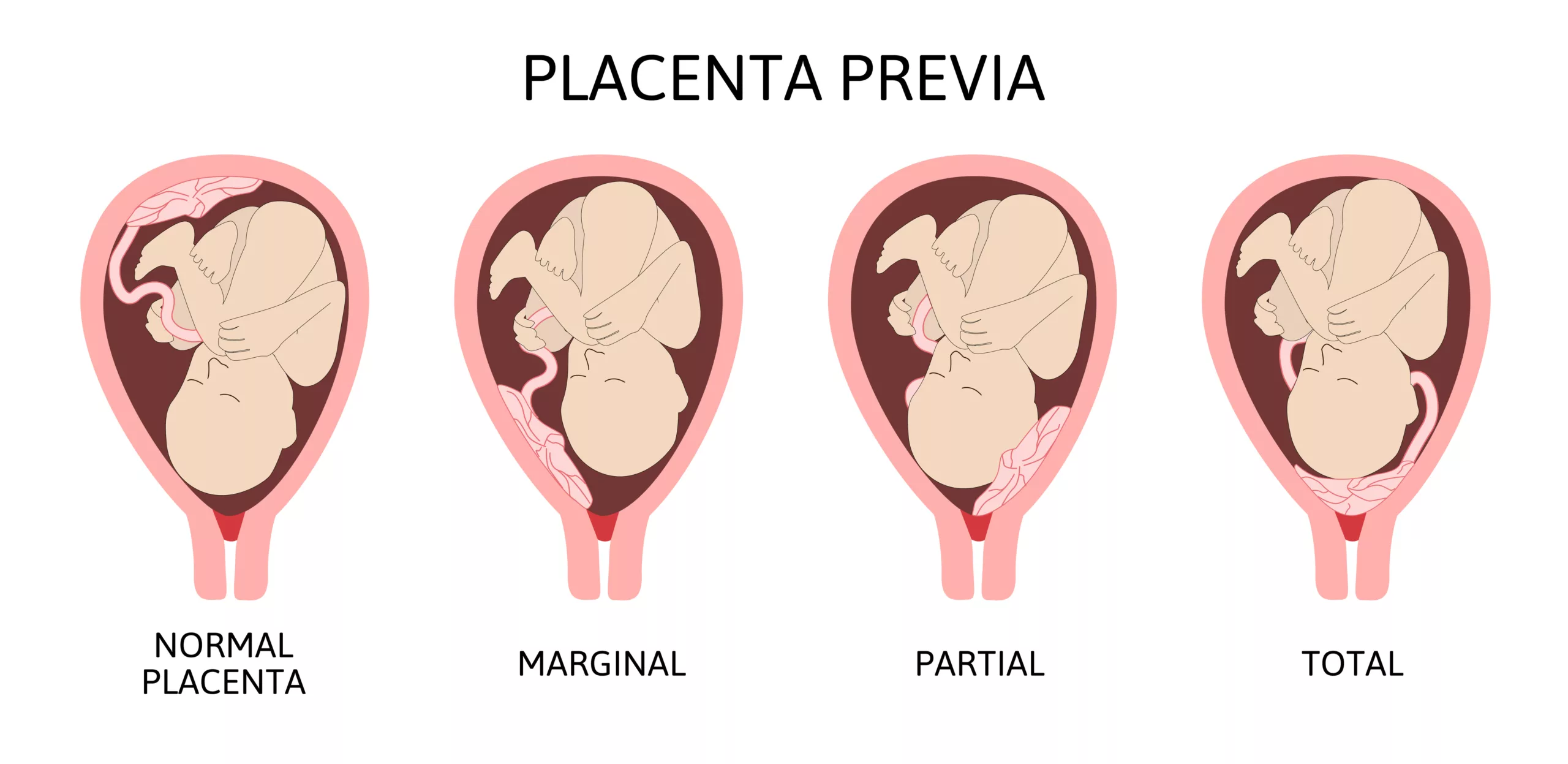
Types Of Placenta Previa
Depending on the location of the placenta in the uterus, it is classified into three types. The placenta touching or partially covering the cervix usually gets better till delivery, but complete previa is more severe and requires cesarean delivery. It is classified into these three types:
Marginal
In this condition, the placenta forms at the margin of the cervix. In marginal placenta previa, the placenta is positioned so that it touches the cervix but does not cover it. This type of condition usually corrects itself.
Partial
In this type, the placenta partially covers the cervix.
Complete/Total Placenta Previa
It is the most severe form of placenta previa, which is unlikely to resolve. In this condition, the placenta totally covers the cervix and blocks the vagina.4Oylese and MD, Y. (2006) Placenta previa, placenta accreta, and vasa previa : Obstetrics & gynecology, LWW. Retrieved 17 February 2024 https://journals.lww.com/greenjournal/Fulltext/2006/04000/Conservative_Versus_Extirpative_Management_in.00029.aspx?casa_token=sGmxVP2rMIkAAAAA%3AaAUoZisJeQ1UVaz4MBgQwnkaLIj0F7hMqhfOG0k-P4ObjahCYvmCONESsWlV6o5iacyeKxmLRhYp9rNcINcMV_MtTg
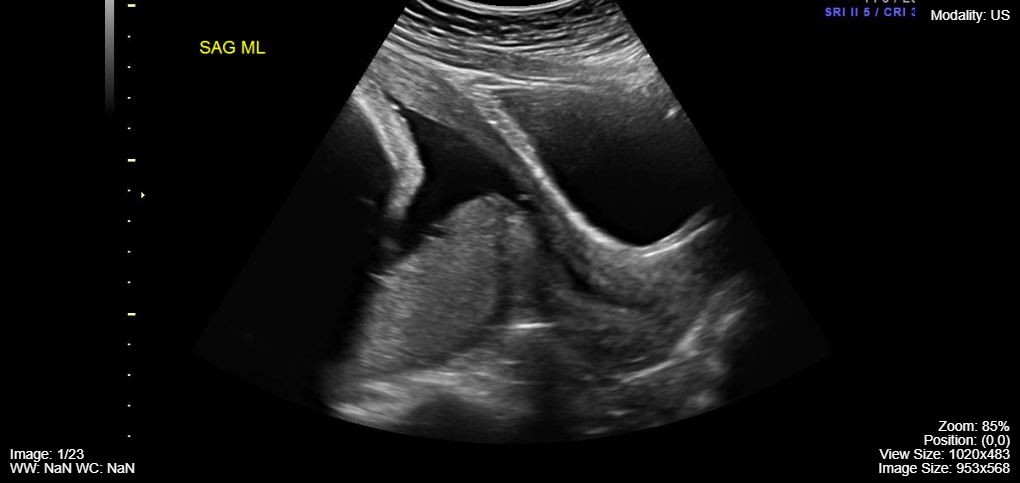
Diagnosis
Your healthcare provider can diagnose this condition during a routine ultrasound in the second half of pregnancy. A patient presenting with vaginal bleeding in the second or third trimester should undergo a transabdominal ultrasound before a digital examination. If placenta previa is suspected, a transvaginal ultrasound should be performed to confirm the exact location of the placenta. This method offers a clearer and more precise image of the placenta’s location relative to the cervix.
Treatment
The main goal of therapy is to get you as close to your due date as possible. For a gestational age of 36 to 37 weeks, C-section is the best option, as vaginal delivery results in heavy bleeding. In case of vaginal bleeding, a cesarean is performed immediately. In short, management depends on the assessment of the risk of vaginal bleeding against the preterm delivery of the baby.
Your medical care provider decides the best treatment option for you based on the following factors:
- Gestational age of the baby
- Type of Placnta Previa (PP)
- Risk of vaginal bleeding
- The overall health of baby and mother7MD, V.J. (2020b) Guideline No. 402: Diagnosis and Management of Placenta Previa, ScienceDirect. Retrieved 17 February 2024 https://www.sciencedirect.com/science/article/abs/pii/S1701216319307261
If you have marginal or partial previa, you need to:
- Take adequate bed rest
- Reduce physical activity
- Avoid sexual activity
- Visit the clinic regularly for antenatal checkups
Other treatment options to avoid heavy bleeding in moderate to severe cases include:
- Medicines to stop early labor
- Blood transfusion
- Steroid shots to help mature the lungs of baby
- Bed rest
Complications
It can cause serious complications that can even lead to hysterectomy. Postpartum hemorrhage, septicemia, maternal intensive care admission, and maternal death are some of the complications. A few have been described below:
Preterm Birth
Excessive vaginal bleeding may compel your healthcare provider to go for an emergency C-section. This leads to the birth of a premature baby without fully developed organs.
Placental Abruption
If this condition gets complicated, it may result in detachment of the placenta from the uterus before birth. This condition is termed as placental abruption.
Bleeding
Severe life-threatening vaginal bleeding is a common complication. It may happen during pregnancy, delivery, or shortly after delivery. Postpartum hemorrhage, bleeding after giving birth, leads to the loss of 1000ml or more blood, giving rise to conditions like low blood pressure, anemia, and shortness of breath.
Placenta Accreta
Placenta accreta is a spectrum of closely related disorders, including placenta previa. In this condition, the placenta expands deep into the wall of the uterus, resulting in excess bleeding following delivery.
Outlook of Placenta Previa
The most significant risk to females with this condition is life-threatening bleeding. It requires immediate delivery before the baby is completely matured.
Neonates
This condition increases the chances of neonatal morbidity and mortality by three to four times, attributing to premature birth.8Silver RM. Abnormal Placentation: Placenta Previa, Vasa Previa, and Placenta Accreta. Obstet Gynecol. 2015 Sep;126(3):654-668. The vital organs of a preterm baby, particularly the lungs, are not developed completely and cannot function properly. For this reason, it is expected that preterm babies are at a higher risk of respiratory distress syndrome.
Mothers
The maternal prognosis for this condition is generally favorable, with delivery resolving about 90% of cases. However, females with complete placenta previa show poor prognosis. They are at high risk of heavy bleeding, damage to nearby organs, hysterectomy, and death. Women who seek regular antenatal examinations can avoid risk due to early diagnosis.9Crane, J.M.G. et al. (2000) Maternal complications with placenta previa, American Journal of Perinatology. Retrieved 17 February 2024 https://www.thieme-connect.com/products/ejournals/abstract/10.1055/s-2000-9269
Vasa Previa Vs. Placenta Previa
Vasa previa is a complication of pregnancy that occurs when the umbilical cord connects to the amniotic sac instead of the placenta. Many blood vessels that link the umbilical cord to the placenta are present near the opening of the vagina. During labor, the disruption of membranes around the baby can also rupture these blood vessels. This results in excessive loss of blood, and the baby is born with bradycardia.
Unlike placenta previa, which can be diagnosed earlier during pregnancy, vasa previa symptoms appear during labor. Dark red blood is the predominant symptom of vasa previa due to oxygen insufficiency. Moreover, partial and complete placenta previa increase the chances of vasa previa.
Placenta Previa Vs. Abruption
Placental abruption is a complication of placenta previa. It happens when the placenta detaches, entirely or partially, from the uterus too early. The placenta contains numerous blood capillaries that transfer oxygen and nutrients to the fetus. Early separation of the placenta causes vaginal bleeding. Placental abruption, or abruptio placenta, occurs due to direct trauma to the uterus or any other unknown cause.10Calleja-Agius, J. et al. (2006) Placental abruption and placenta praevia – European clinics in obstetrics and gynecology, SpringerLink. Retrieved 17 February 2024 https://link.springer.com/article/10.1007/s11296-006-0046-5
However, in placenta previa, the placenta remains intact till the delivery of the baby. Furthermore, women with this condition face painless vaginal bleeding. Conversely, females with placental abruption suffer from painful vaginal bleeding with painful cramps and contractions.
Prevention of Placenta Previa
You cannot prevent it; no medical procedure exists to prevent this condition. However, you can avoid some risk factors like smoking and use of cocaine that increase the risk of having PP. After diagnosis is established, there are some strategies to reduce vaginal bleeding and ensure the safety of mother and child.
Final Words
It is a curable condition if diagnosed and managed appropriately. Routine ultrasound examinations and antenatal checkups are essential for timely diagnosis of this condition. Do not hesitate to contact your healthcare provider if you find signs of vaginal bleeding or abdominal cramping. Your doctor would recommend regular ultrasound and some other medications to avoid complications or might order a cesarean immediately in severe conditions.
Refrences
- 1Anderson-Bagga, F.M. (2023) Placenta previa, StatPearls [Internet]. Retrieved 17 February 2024 https://www.ncbi.nlm.nih.gov/books/NBK539818/#article-27262.r6
- 2RM; S. (2015) Abnormal placentation: Placenta previa, vasa previa, and placenta accreta, Obstetrics, and Gynecology. Retrieved 13 February 2024 https://pubmed.ncbi.nlm.nih.gov/26244528/
- 3CV, F.A. (2009) Etiology and risk factors for PLACENTA PREVIA: An overview and meta-analysis of observational studies, The journal of maternal-fetal & neonatal medicine : the official journal of the European Association of Perinatal Medicine, the Federation of Asia and Oceania Perinatal Societies, the International Society of Perinatal Obstetricians. Retrieved 17 February 2024 https://pubmed.ncbi.nlm.nih.gov/12820840/?dopt=Abstract
- 4Oylese and MD, Y. (2006) Placenta previa, placenta accreta, and vasa previa : Obstetrics & gynecology, LWW. Retrieved 17 February 2024 https://journals.lww.com/greenjournal/Fulltext/2006/04000/Conservative_Versus_Extirpative_Management_in.00029.aspx?casa_token=sGmxVP2rMIkAAAAA%3AaAUoZisJeQ1UVaz4MBgQwnkaLIj0F7hMqhfOG0k-P4ObjahCYvmCONESsWlV6o5iacyeKxmLRhYp9rNcINcMV_MtTg
- 5Ahn KH, Lee EH, Cho GJ, Hong SC, Oh MJ, Kim HJ. Anterior placenta previa in the mid-trimester of pregnancy as a risk factor for neonatal respiratory distress syndrome. PLoS One. 2018;13(11):e0207061.
- 6Feng Y, Li XY, Xiao J, Li W, Liu J, Zeng X, Chen X, Chen KY, Fan L, Kang QL, Chen SH. Risk Factors and Pregnancy Outcomes: Complete versus Incomplete Placenta Previa in Mid-pregnancy. Curr Med Sci. 2018 Aug;38(4):597-601.
- 7MD, V.J. (2020b) Guideline No. 402: Diagnosis and Management of Placenta Previa, ScienceDirect. Retrieved 17 February 2024 https://www.sciencedirect.com/science/article/abs/pii/S1701216319307261
- 8Silver RM. Abnormal Placentation: Placenta Previa, Vasa Previa, and Placenta Accreta. Obstet Gynecol. 2015 Sep;126(3):654-668.
- 9Crane, J.M.G. et al. (2000) Maternal complications with placenta previa, American Journal of Perinatology. Retrieved 17 February 2024 https://www.thieme-connect.com/products/ejournals/abstract/10.1055/s-2000-9269
- 10Calleja-Agius, J. et al. (2006) Placental abruption and placenta praevia – European clinics in obstetrics and gynecology, SpringerLink. Retrieved 17 February 2024 https://link.springer.com/article/10.1007/s11296-006-0046-5





