What is Prurigo Nodularis?
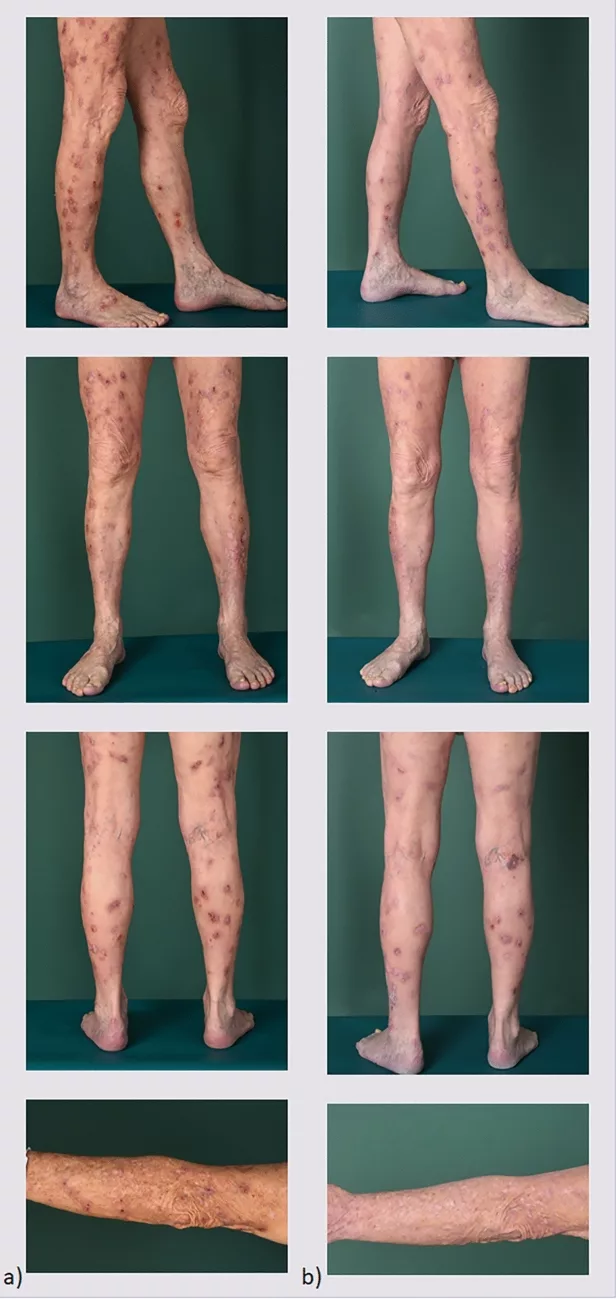
Prurigo nodularis (PN) is a rare, chronic skin condition primarily affecting older adults. It is characterized by multiple, firm, itchy nodules or rashes that are symmetrically distributed across the skin. The rash can develop on any body part but mainly occurs in the arms, legs, back, and stomach regions. The prevalence of prurigo nodularis in the United States is estimated to be 36.7 to 148.3 per 100,000 population.1Ständer, S., Augustin, M., Berger, T., Elmariah, S., Korman, N. J., Weisshaar, E., & Yosipovitch, G. (2021). Prevalence of prurigo nodularis in the United States of America: a retrospective database analysis. JAAD international, 2, 28. In several cases, the disease is associated with other skin disorders, such as dermatoses (especially atopic dermatitis) and chronic pruritis.
Prurigo Nodularis (PN) Symptoms
The symptoms of PN include the following:
Itchy Spots
The initial presentation of nodular prurigo is itchiness. Many people report itchy skin areas without any nodules. The episodes of itchiness may be episodic or can be long-lasting. The itchy dermal spots then transform into lumps or bumps. PN causes evident impairments in quality of life due to the severe “super itch” it causes.
Itchy Bumps
PN causes one of the worst itches (some say it has the worst itch intensity).2Hashimoto, T., Nattkemper, L. A., Kim, H. S., Kursewicz, C. D., Fowler, E., Shah, S. M., … & Yosipovitch, G. (2021). Itch intensity in prurigo nodularis is closely related to dermal interleukin‐31, oncostatin M, IL‐31 receptor alpha, and oncostatin M receptor beta. Experimental dermatology, 30(6), 804-810. Thus, patients scratch and pick repeatedly, which leads to transformation into nodules. It generally takes around six weeks for the itchy spots to become bumps.
The following features of the bumps are seen:
- Form on both sides of the body.
- Range in size from 0.5 to 2 cm in diameter (pinhead to larger size).
- The number of bumps varies from 2 to 200.
- The bumps may be raised from the rest of the skin.
- The crusty, scaly bumps resemble warts in appearance.
- The raised bumps vary in color from pink and red to brown-black.

Burning/Stinging Sensations
Burning sensation gravely impacts the quality of life. Studies show that severe prurigo patients report stinging and burning accompanied by pain in the nodular lesions and intralesional skin.3Aggarwal, P., Choi, J., Sutaria, N., Roh, Y. S., Wongvibulsin, S., Williams, K. A., … & Kwatra, S. G. (2021). Clinical characteristics and disease burden in prurigo nodularis. Clinical and Experimental Dermatology, 46(7), 1277-1284. A few patients also report strange feelings of bugs crawling on the skin.
Bleeding From The Bumps
Frequent, repetitive scratching of the bumps eventually leads to breaking and bleeding. Most patients explain an unpleasant scratching experience as it makes you itch more and may make the skin too painful to touch—there are many reports of black spots forming on the bump region after too much scratching. The bumps may also scar after healing.
The scaly-bumpy appearance of the skin, paired with the uncontrollable urge to itch, makes patients embarrassed and shameful. This leads to limiting social activities and anxiety. The itch-scratch cycle also disrupts sleep and interferes with daily routine, all of which ultimately leads to depression.
Prurigo Nodularis Causes and Risk Factors
The exact cause of prurigo nodularis is unknown. In a pathophysiological context, this dermal condition arises due to certain changes in the skin cells. Many have noted changes in the number of nerve cells within the skin layers (papillary dermis) accompanied by changes in the neuroimmune system (increased neuropeptides). PN lesions show increased dermal and Merkel cells in the epidermis. Additionally, there is an upregulation of mast cells and neutrophils in PN patients.
However, researchers are of the view that there is always a dermatological complication in PN patients. Skin conditions found in association with prurigo nodularis include:
- Dry skin
- Eczema (atopic dermatitis)
- Lichen planus
According to a study, all PN patients under observation suffered from a dermatological disease or a systemic disease. The most commonly associated skin disorder was endogenous eczema.4Tan, W. S., & Tey, H. L. (2014). Extensive prurigo nodularis: characterization and etiology. Dermatology, 228(3), 276-280.
Underlying systemic conditions that increase your chances of developing nodular prurigo include:
- Diabetes
- Thyroid dysfunction
- Neuropsychiatric disorders
- Lymphoma
- HIV infection
- Chronic kidney disease
- Hepatitis C
- Chronic obstructive pulmonary disease (COPD)
Chronic Diseases
The use of chemotherapeutic drugs, like pembrolizumab and carboplatin etc., may also increase your chances of PN. Research reveals a close association between diabetes (type 1 and 2) and PN.5Huang, A. H., Williams, K. A., & Kwatra, S. G. (2020). Prurigo nodularis: epidemiology and clinical features. Journal of the American Academy of Dermatology, 83(6), 1559-1565.
An underlying faulty thyroid gland (as in Hashimoto thyroiditis) may also be the culprit for PN development. Several patients with thyroiditis have displayed nodular prurigo. 6Rishi, R., Ringwala, S., Tracy, J., & Fatteh, S. (2014). Prurigo nodularis and Hashimoto thyroiditis. Annals of Allergy, Asthma & Immunology, 113(6), 673-674. In addition to thyroid abnormalities, auto-immune disorders can also be associated with nodular prurigo. Lupus patients may also suffer from PN. However, one study showed that almost 13% of PN patients had no comorbidity or predisposing disease, thus adding to the unique nature of the disorder.7Kowalski, E. H., Kneiber, D., Valdebran, M., Patel, U., & Amber, K. T. (2019). Treatment-resistant prurigo nodularis: challenges and solutions. Clinical, cosmetic and investigational dermatology, 163-172.
High-Risk Patients
Chronic inflammatory skin disease seems to have a propensity for middle-aged individuals (51-65 years of age), women, and people belonging to the Black community.
Is Prurigo Nodularis Contagious?
No, prurigo nodularis is not contagious. However, you may transmit or contract other diseases through the exchange of body fluids (blood oozing from an open bump). Therefore, you should be cautious when dealing with HIV-positive or hepatitis patients.
Prurigo Nodularis Diagnosis
Your healthcare provider will thoroughly examine your skin lesions to reach a diagnosis. The main points to look for in a suspected case of PN are the size, location, and color of the bumps. Your doctor will also ask for the intensity of itch (as PN is severely itchy) and any specific triggers that increase itchiness.
A complete drug history is also important as sometimes, drug allergy or an adverse drug reaction can lead to urticaria or itchiness. Tests that can aid prurigo diagnosis include:
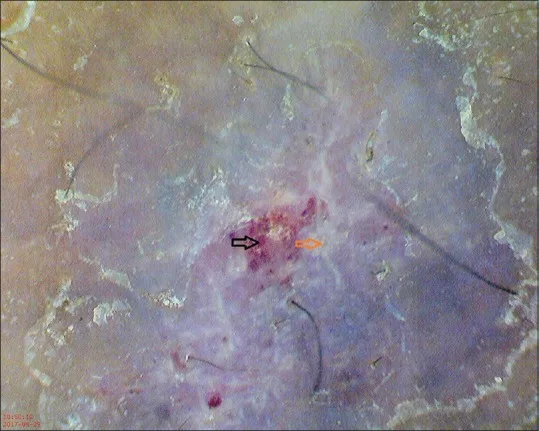
Dermoscopy:
In this test, the doctor observes your skin lesions under a light microscope. A magnified view of the skin makes diagnosis easier.
Skin biopsy:
A small portion of the skin (dermis and epidermis) is removed using a scalpel and sent to a pathology lab for microscopic analysis. Biopsies help differentiate PN from any cancerous conditions.
Your doctor may also order certain blood and urine tests to analyze the condition of your kidneys, thyroid, etc. This is done to rule out PN secondary to chronic ailments.
Prurigo Simplex Vs. Prurigo Nodularis
A skin condition, quiet similar to prurigo nodularis is prurigo simplex. In prurigo simplex, numerous tiny blisters form on the buttocks and limbs (mostly). The lesions are symmetrical in distribution. However, the blisters of nodular prurigo are thicker and larger in number than those of prurigo simplex.
Other conditions that fall into DD for prurigo nodularis include prurigo pigmentosa, pruritus (itch without lesion), pemphigoid nodularis, discoid eczema, and atopic eczema.
Prurigo Nodularis Treatment
The main aim of all treatment strategies is to relieve the itch and improve the quality of life. The following treatment modalities are effective for prurigo nodularis:
Topical Management:
Mild nodular prurigo can be managed well with topical creams and ointments. Antihistamines can alleviate itch and are branded as anti-itch medications. Calamine lotion application has minimal but positive results. Most patients rely on topical corticosteroids and calcineurin inhibitors (immune suppressants) for relief. Immunosuppressants are the first choice of most physicians. Therefore, topical calcineurin inhibitors are frequently used.
According to a study, the following topical medicines conveyed beneficial effects in PN patients:8Qureshi, A. A., Abate, L. E., Yosipovitch, G., & Friedman, A. J. (2019). A systematic review of evidence-based treatments for prurigo nodularis. Journal of the American Academy of Dermatology, 80(3), 756-764.
- Corticosteroids
- Calcineurin inhibitors
- Calcipotriol-vitamin D3 ointment (anti-psoriatic)
- Capsaicin (chili pepper extract)
Injections:
When topical application is insufficient, the doctor chooses to deliver the drugs directly into the lesions. Corticosteroid injections into the nodules reduce inflammation and redness. The evident decrease in the urge to itch relaxes the patient.
Medications:
Newer drugs like thalidomide can be beneficial in managing symptoms but have side effects. Different classes of drugs are continually being employed to get rid of PN symptoms. Some studies advocate the use of pregabalin (anti-convulsant), fluvoxamine (anti-depressant), amitriptyline (tricyclic antidepressant), and neurokinin-1 receptor antagonists (antidepressant/anti-emetic). However, there is little evidence that supports the use of medicines like naltrexone (opioid antagonist), aprepitant (anti-nausea/vomiting), and pregabalin for PN.9Frølunde, A. S., Wiis, M. A. K., Ben Abdallah, H., Elsgaard, S., Danielsen, A. K., Deleuran, M., & Vestergaard, C. (2022). Non-atopic chronic nodular prurigo (prurigo nodularis hyde): a systematic review of best-evidenced treatment options. Dermatology, 238(5), 950-960.
Phototherapy:
Light therapy has exceptional benefits for multiple skin conditions, like dermatitis. Specialized devices direct special light (mostly Ultraviolet) to the affected skin.
UV light is used to reduce the size of the nodules in nodular prurigo. In a study, 44 patients received phototherapy (UV-A and UV-B). The treatment was well tolerated, and the clearance rate of the lesions was greater than 75%. The outcome was satisfactory, and the study concluded that phototherapy can be combined with monotherapy for superior results.10Arrieta, A., Jaka, A., Del Alcázar, E., Blanco, M., & Carrascosa, J. M. (2021). Phototherapy for prurigo nodularis: our experience and a review of the literature. Actas Dermo-Sifiliográficas (English Edition), 112(4), 339-344. Sometimes, an antipsoriatic drug, i.e., psoralen, is paired with UVA for better results. The therapy is thus known as PUVA.
Cryotherapy:
This technique removes blisters and tumorous growths by freezing them. The doctor directly applies liquid nitrogen to the bumps, which freeze under the extreme cold. Your healthcare provider might also use a cryoprobe (special device) to freeze the blister. When given in cycles, cryotherapy leads to significant nodule clearance.11Mayala, E. V., Mavura, D. R., Robert, M., & Masenga, E. J. (2021). Prurigo nodularis comparative treatment outcome in patients attending a tertiary hospital in northern Tanzania. Dermatologic Therapy, 34(2), e14855.
Immunosuppressant Therapy:
Many dermatologists believe PN to have an auto-immune component. If you are suffering from an auto-immune disorder (Lupus, RA, psoriasis, etc.), your doctor will prescribe you immune-suppressing drugs like cyclosporine or methotrexate (MTX). However, immune suppressants are advised even with no underlying auto-immune disease. Studies show that MTX offers astonishing clearance of nodules and works well in prurigo cases that require prurigo treatment.12Klejtman, T., Beylot‐Barry, M., Joly, P., Richard, M. A., Debarbieux, S., Misery, L., … & Ingen‐Housz‐Oro, S. (2018). Treatment of prurigo with methotrexate: a multicentre retrospective study of 39 cases. Journal of the European Academy of Dermatology and Venereology, 32(3), 437-440.
It was concluded in a 2024 study that methotrexate, cyclosporine, and phototherapy (NB-UVB) are the most effective treatment modalities for prurigo nodularis. However, doctors should be cautious about the adverse effects.13Taghaddos, D., Savinova, I., & Abu-Hilal, M. (2024). Clinical Characteristics and Treatment Outcomes of Prurigo Nodularis: A Retrospective Study. Journal of Cutaneous Medicine and Surgery, 12034754241227808.
Clinical trials are ongoing for some drugs. Nemolizumab is a monoclonal antibody (a biological drug used in auto-immune disorders) that has shown promising results in PN treatment. In a phase 3 trial of nemolizumab monotherapy, it was observed that the drug significantly alleviated signs and symptoms of prurigo nodularis.14Kwatra, S. G., Yosipovitch, G., Legat, F. J., Reich, A., Paul, C., Simon, D., … & Ständer, S. (2023). Phase 3 trial of nemolizumab in patients with prurigo nodularis. New England Journal of Medicine, 389(17), 1579-1589. Another monoclonal antibody under trial for prurigo nodularis is dupilumab.
Other modes to eliminate bumps include excimer laser and pulsed dye laser.
Personal Care Strategies for Prurigo Nodularis
You can adopt the following simple strategies to manage prurigo and improve your quality of life:
Apply Cold:
Use cold compresses or ice packs to cool down the itchy areas.
Avoid the Sun:
Limit outdoor movement and use sunscreen when going out.
Moisturize the Skin:
Frequently apply petroleum jelly (Vaseline) to prevent dry skin.
Take Short Baths:
Lukewarm water baths for short periods can keep your skin healthy.
Avoid Hectic Activities:
Sweating can make things worse. Thus, you should avoid activities that make you sweat.
How Can I Prevent Nodular Prurigo?
The exact cause of prurigo nodularis is unknown; therefore, you can’t certainly avoid it by abstaining from specific activities. However, autoimmune patients suffering from Lupus or psoriasis must be cautious about their skin health. You must intervene and consult your doctor before the itch-scratch cycle starts.
Final Word
Prurigo nodularis is an inflammatory skin condition in which multiple small bumps form on the limb, buttocks, and abdomen. The causes of this super-itchy are unknown. However, autoimmune patients (Lupus, psoriasis) and dry skin patients commonly suffer from nodular prurigo. Mild prurigo nodularis can be managed with topical medications such as calcineurin inhibitors, corticosteroids, and vitamin D3 preparations. Moderate cases require systemic medications, including corticosteroids, thalidomide, pregabalin, etc. Other effective therapies include phototherapy and cryotherapy. Advanced biologic drugs like nemolizumab and dupilumab (monoclonal antibodies) are being tested as these drugs provide promising results in managing PN.
Refrences
- 1Ständer, S., Augustin, M., Berger, T., Elmariah, S., Korman, N. J., Weisshaar, E., & Yosipovitch, G. (2021). Prevalence of prurigo nodularis in the United States of America: a retrospective database analysis. JAAD international, 2, 28.
- 2Hashimoto, T., Nattkemper, L. A., Kim, H. S., Kursewicz, C. D., Fowler, E., Shah, S. M., … & Yosipovitch, G. (2021). Itch intensity in prurigo nodularis is closely related to dermal interleukin‐31, oncostatin M, IL‐31 receptor alpha, and oncostatin M receptor beta. Experimental dermatology, 30(6), 804-810.
- 3Aggarwal, P., Choi, J., Sutaria, N., Roh, Y. S., Wongvibulsin, S., Williams, K. A., … & Kwatra, S. G. (2021). Clinical characteristics and disease burden in prurigo nodularis. Clinical and Experimental Dermatology, 46(7), 1277-1284.
- 4Tan, W. S., & Tey, H. L. (2014). Extensive prurigo nodularis: characterization and etiology. Dermatology, 228(3), 276-280.
- 5Huang, A. H., Williams, K. A., & Kwatra, S. G. (2020). Prurigo nodularis: epidemiology and clinical features. Journal of the American Academy of Dermatology, 83(6), 1559-1565.
- 6Rishi, R., Ringwala, S., Tracy, J., & Fatteh, S. (2014). Prurigo nodularis and Hashimoto thyroiditis. Annals of Allergy, Asthma & Immunology, 113(6), 673-674.
- 7Kowalski, E. H., Kneiber, D., Valdebran, M., Patel, U., & Amber, K. T. (2019). Treatment-resistant prurigo nodularis: challenges and solutions. Clinical, cosmetic and investigational dermatology, 163-172.
- 8Qureshi, A. A., Abate, L. E., Yosipovitch, G., & Friedman, A. J. (2019). A systematic review of evidence-based treatments for prurigo nodularis. Journal of the American Academy of Dermatology, 80(3), 756-764.
- 9Frølunde, A. S., Wiis, M. A. K., Ben Abdallah, H., Elsgaard, S., Danielsen, A. K., Deleuran, M., & Vestergaard, C. (2022). Non-atopic chronic nodular prurigo (prurigo nodularis hyde): a systematic review of best-evidenced treatment options. Dermatology, 238(5), 950-960.
- 10Arrieta, A., Jaka, A., Del Alcázar, E., Blanco, M., & Carrascosa, J. M. (2021). Phototherapy for prurigo nodularis: our experience and a review of the literature. Actas Dermo-Sifiliográficas (English Edition), 112(4), 339-344.
- 11Mayala, E. V., Mavura, D. R., Robert, M., & Masenga, E. J. (2021). Prurigo nodularis comparative treatment outcome in patients attending a tertiary hospital in northern Tanzania. Dermatologic Therapy, 34(2), e14855.
- 12Klejtman, T., Beylot‐Barry, M., Joly, P., Richard, M. A., Debarbieux, S., Misery, L., … & Ingen‐Housz‐Oro, S. (2018). Treatment of prurigo with methotrexate: a multicentre retrospective study of 39 cases. Journal of the European Academy of Dermatology and Venereology, 32(3), 437-440.
- 13Taghaddos, D., Savinova, I., & Abu-Hilal, M. (2024). Clinical Characteristics and Treatment Outcomes of Prurigo Nodularis: A Retrospective Study. Journal of Cutaneous Medicine and Surgery, 12034754241227808.
- 14Kwatra, S. G., Yosipovitch, G., Legat, F. J., Reich, A., Paul, C., Simon, D., … & Ständer, S. (2023). Phase 3 trial of nemolizumab in patients with prurigo nodularis. New England Journal of Medicine, 389(17), 1579-1589.

