What are Uterine Polyps?
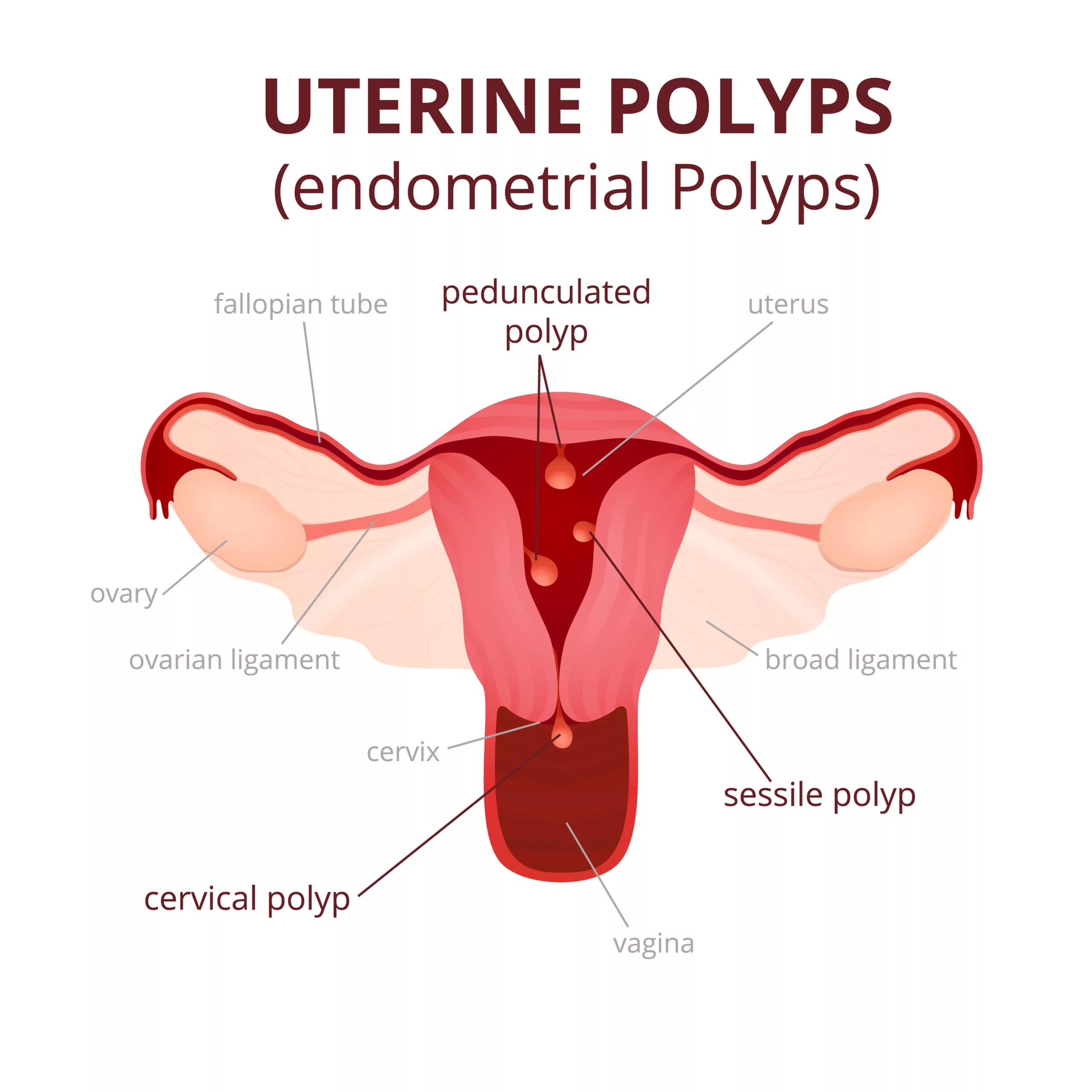
Uterine or endometrial polyps are abnormal growths protruding from the inner lining of the uterine cavity. This abnormal growth contains glands, vessels, and stroma. They come in various sizes, spanning from a few millimeters to several centimeters, sometimes reaching the size of a golf ball or larger, and can potentially fill the entire uterine cavity.1Nijkang, N. P., Anderson, L., Markham, R., & Manconi, F. (2019). Endometrial polyps: Pathogenesis, sequelae, and treatment. SAGE open medicine, 7, 2050312119848247. https://doi.org/10.1177/2050312119848247
Endometrial polyps can occur in all ages, but the peak incidence is between 40 and 45. Polyps have a high prevalence rate of 32% in females aged 29 or 30 years with infertility. These are usually noncancerous but can be malignant. Premenopausal females are less likely to have malignant polyps than postmenopausal females, who are at higher risk.2Hinckley, M. D., & Milki, A. A. (2004). 1000 office-based hysteroscopies prior to in vitro fertilization: feasibility and findings. JSLS: Journal of the Society of Laparoendoscopic Surgeons, 8(2), 103–107.
Polyps vary in morphology. If an endometrial polyp is connected to the surface of the uterus by a slender, elongated stem, it is referred to as pedunculated. Conversely, if it lacks a stem and has a wide, flat base, it is termed sessile. These polyps typically exhibit a smooth, rounded, or cylindrical appearance, and their color ranges from tan to yellow.3Nijkang NP, Anderson L, Markham R, Manconi F. Endometrial polyps: Pathogenesis, sequelae, and treatment. SAGE Open Med. 2019 May 2;7:2050312119848247. doi: 10.1177/2050312119848247. PMID: 31105939; PMCID: PMC6501471.
Signs & Symptoms of Uterine Polyps
Signs and symptoms of uterine polyps vary. They can be small and asymmetric or large enough to fill the whole uterus, leading to infertility and menstrual problems.
The following are the signs and symptoms of uterine polyps:
- Intermenstrual bleeding or IMB (bleeding between periods)
- HMB/heavy menstrual bleeding
- Postmenopausal bleeding in older females
- Irregular menstrual cycle with variable length and heaviness
- Bleeding during or after intercourse
- Pelvic pain during intercourse
- Infertility (inability to conceive)
Some polyps are asymptomatic and may seem to be hanging from the cervix. (Cervical polyps). Your doctor may accidentally find them during a physical examination of the genital tract.
What Causes Uterine Polyps?
The exact cause of uterine polyps is still unknown, but according to some research studies, it is believed to be related to estrogen stimulation, characterized by an increased concentration of estrogen receptors (ERs), particularly ER-alpha, in polyp glandular cells. This estrogen dominance, coupled with decreased expression of progesterone receptors (PRs), contributes to the development of these polyps in the inner lining of the uterus (endometrium). Additionally, abnormalities in cell survival and proliferation markers, chromosomal rearrangements, and the expression of specific genes like p63, aromatase P450, and SF-1 may also play a role in forming endometrial polyps.4Nijkang NP, Anderson L, Markham R, Manconi F. Endometrial polyps: Pathogenesis, sequelae, and treatment. SAGE Open Med. 2019 May 2;7:2050312119848247. Doi: 10.1177/2050312119848247. PMID: 31105939; PMCID: PMC6501471.
Uterine polyps can also develop due to genetic abnormalities, resulting in the monoclonal growth of altered endometrial cells. Monoclonal growth means that the polyps originate from a single abnormal cell or a small group of identical abnormal cells in the endometrium (inner lining of the uterus). This distinguishes polyps from other types of growths with different cellular origins.5Nijkang, N. P., Anderson, L., Markham, R., & Manconi, F. (2019). Endometrial polyps: Pathogenesis, sequelae and treatment. SAGE open medicine, 7, 2050312119848247. https://doi.org/10.1177/2050312119848247
Risk Factors For Uterine Polyps
Uterine polyps can occur due to metabolic disorders, medications, chronic inflammation, and hormonal replacement therapy. The following are risk factors for uterine polyps:
Obesity:
Excessive fats in obese people convert into estrogen by aromatization reaction. Unopposed stimulation of estrogen causes endometrial hyperplasia, resulting in the formation of uterine polyps.
Hypertension:
Hypertensive people tend to have a higher body mass index compared to others. High BMI is a risk factor for endometrial polyps.
Medications:
Some medicines that act as estrogen agonists can cause the formation of uterine polyps. Tamoxifen (estrogen agonist), which is normally used to treat breast cancer, is the major risk factor for polyp formation.
Medications like tamoxifen increase the incidence of uterine polyps by 20-35 %.6Mansour T, Chowdhury YS. Endometrial Polyp. [Updated 2023 Apr 25]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK557824/
Hormonal Replacement Therapy:
Women who get hormonal replacement therapy are at a higher risk than others. This occurs due to overstimulation of the endometrium by estrogen.
Age:
Women with ages greater than 60 years are at higher risk of getting polyps formation. This occurs due to an imbalance in estrogen levels before and after menopause.
Diagnosis of Uterine Polyps
Diagnosis of uterine polyps starts with taking a detailed history followed by a physical examination. Some other tests that are used to confirm the diagnosis and rule out other diseases are :
- Pap smear test
- Ultrasound (transvaginal and transabdominal)
- Hysteroscopy
- Histological examination by taking an endometrial biopsy
History & Physical Examination:
Your healthcare provider will gather a detailed medical history to diagnose uterine polyps. This process includes discussing your menstrual history, any abnormal bleeding patterns, pelvic pain, and other relevant symptoms. Information about your reproductive history, hormone use, and relevant medical conditions will also be considered. This comprehensive evaluation forms the foundation for accurate diagnosis and appropriate management.
After a detailed history, your doctor will perform a gynecological examination (examination of private parts) to check the location, size, and shape of these polyps. Further tests for polyps are the following:
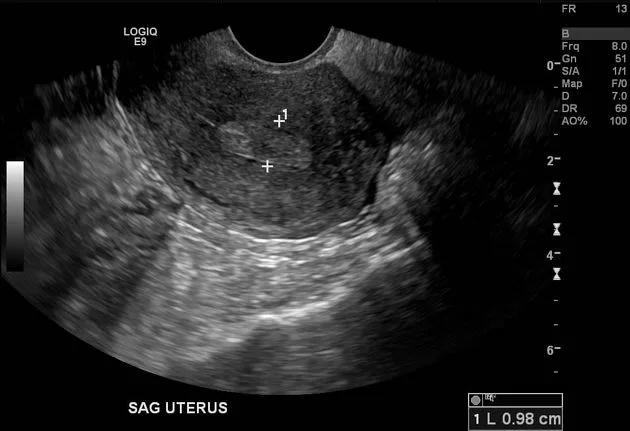
Transvaginal Ultrasound:
Transvaginal ultrasound is the investigation of choice to diagnose uterine polyps. In this procedure, a small ultrasound transducer is inserted into the vagina by your doctor for vaginal examination. Your doctor may use saline infusion sonohysterography (SIS) to enhance the diagnostic accuracy of transvaginal ultrasound. He will infuse a contrast with saline into your uterus to expand it and provide a clear view of endometrial polyps.7Fadl, S. A., Sabry, A. S., Hippe, D. S., Al-Obaidli, A., Yousef, R. R., & Dubinsky, T. J. (2018). Diagnosing Polyps on Transvaginal Sonography: Is Sonohysterography Always Necessary? Ultrasound Quarterly, 34(4), 272–277. https://doi.org/10.1097/RUQ.0000000000000384
Hysteroscopy:
Hysteroscopy is a procedure to examine the inner part of the uterus and cervix. This procedure uses a hand-held flexible tube called a hysteroscope. This is a diagnostic as well as a therapeutic procedure. A detailed genital tract examination is done by this procedure to rule out any other disease. In suspected cases, a biopsy is taken for further workup.
Biopsy:
In most cases, uterine polyps are noncancerous, but they can be precancerous. A biopsy is taken when your doctor suspects some malignancy. In such a case, diagnostic hysteroscopy can be advised to take a uterine sample.
Curettage:
Curette is a long metallic instrument with a loop at the end. Your doctor will scrap and collect endometrial tissue with the help of a curette. This is a traditional method to examine and remove uterine polyps. Nowadays, hysteroscopy is preferred.
Treatment of Uterine Polyps:
There are several treatment options for managing uterine polyps, depending on the size, shape, and location of the polyps. The following are treatment approaches for endometrial polyps:
Watchful Waiting:
Small and asymptomatic (that do not show any symptoms) polyps do not need surgical resection. They might resolve on their own. In case of bleeding, severe pain during intercourse with your partner, or worsening symptoms, you must consult your gynecologist.
Medications:
Hormonal medications, such as hormonal contraceptives (birth control pills), may help regulate menstrual cycles and reduce abnormal bleeding associated with uterine polyps.
Surgical Resection or Uterine Polypectomy:
In the case of large and symptomatic polyps, uterine polypectomy is the treatment of choice. Your doctor will use a flexible, tube-like instrument called a hysteroscope to remove uterine polyps from the base. This is an accurate and precise method to treat uterine polyps. Uterine polypectomy has a low recurrence rate.
Hysterectomy:
Hysterectomy is a surgical procedure in which your uterus is removed. It is done when the polyps are painful, cancerous, and not responding to any therapy.
How do Uterine Polyps affect Pregnancy?
Small polyps do not usually affect the pregnancy. However, large polyps cover the area of the uterus, resulting in interfering with sperm penetration and the embryo implantation process. Thus, large polyps increase the risk of subfertility.
Can they recur after Removal?
Postoperative recurrence of the endometrial polyps depends upon the nature, size, and follow-up duration after polypectomy. According to some studies, the postoperative recurrence rate was about 2.5 to 43.6%.8Yang JH, Chen CD, Chen SU, Yang YS, Chen MJ. Factors Influencing the Recurrence Potential of Benign Endometrial Polyps after Hysteroscopic Polypectomy. PLoS One. 2015 Dec 11;10(12):e0144857. doi: 10.1371/journal.pone.0144857. PMID: 26660149; PMCID: PMC4676604.
Conclusion
Uterine or endometrial polyps vary in size, shape, and location. They can lead to heavy menstrual bleeding, infertility, painful intercourse, and irregular periods. Smaller and asymptomatic polyps need watchful waiting. Uterine polypectomy is the treatment of choice for symptomatic and large polyps.
Refrences
- 1Nijkang, N. P., Anderson, L., Markham, R., & Manconi, F. (2019). Endometrial polyps: Pathogenesis, sequelae, and treatment. SAGE open medicine, 7, 2050312119848247. https://doi.org/10.1177/2050312119848247
- 2Hinckley, M. D., & Milki, A. A. (2004). 1000 office-based hysteroscopies prior to in vitro fertilization: feasibility and findings. JSLS: Journal of the Society of Laparoendoscopic Surgeons, 8(2), 103–107.
- 3Nijkang NP, Anderson L, Markham R, Manconi F. Endometrial polyps: Pathogenesis, sequelae, and treatment. SAGE Open Med. 2019 May 2;7:2050312119848247. doi: 10.1177/2050312119848247. PMID: 31105939; PMCID: PMC6501471.
- 4Nijkang NP, Anderson L, Markham R, Manconi F. Endometrial polyps: Pathogenesis, sequelae, and treatment. SAGE Open Med. 2019 May 2;7:2050312119848247. Doi: 10.1177/2050312119848247. PMID: 31105939; PMCID: PMC6501471.
- 5Nijkang, N. P., Anderson, L., Markham, R., & Manconi, F. (2019). Endometrial polyps: Pathogenesis, sequelae and treatment. SAGE open medicine, 7, 2050312119848247. https://doi.org/10.1177/2050312119848247
- 6Mansour T, Chowdhury YS. Endometrial Polyp. [Updated 2023 Apr 25]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK557824/
- 7Fadl, S. A., Sabry, A. S., Hippe, D. S., Al-Obaidli, A., Yousef, R. R., & Dubinsky, T. J. (2018). Diagnosing Polyps on Transvaginal Sonography: Is Sonohysterography Always Necessary? Ultrasound Quarterly, 34(4), 272–277. https://doi.org/10.1097/RUQ.0000000000000384
- 8Yang JH, Chen CD, Chen SU, Yang YS, Chen MJ. Factors Influencing the Recurrence Potential of Benign Endometrial Polyps after Hysteroscopic Polypectomy. PLoS One. 2015 Dec 11;10(12):e0144857. doi: 10.1371/journal.pone.0144857. PMID: 26660149; PMCID: PMC4676604.

