Retinoblastoma is an aggressive childhood tumour that arises from the retina, i.e., the light-sensitive area at the back of the eye. It makes up 3% of all childhood cancers and can be fatal if left untreated.1Rao, R., & Honavar, S. G. (2017). Retinoblastoma. Indian Journal of Pediatrics, 84(12), 937–944. https://doi.org/10.1007/s12098-017-2395-0 Though infants and children under the age of 5 are primarily affected by it, it can occur in any age group.
Normally, during development, nerve cells in the eye mature and differentiate to form the retina’s photoreceptors. These receptors, also called rods and cones, receive visual input from the environment and send it to the brain. The brain then translates them into images.
But sometimes, due to an abnormality, these cells do not mature properly and grow out of control to form a tumour.
Retinoblastoma Causes
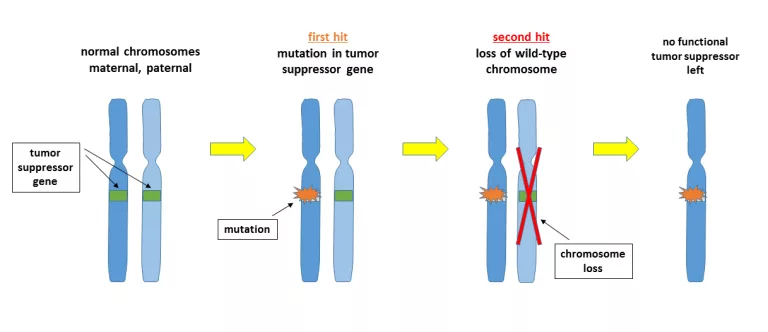
The primary cause of cancer is a mutation of the Retinoblastoma 1 (RB1) gene.2 Wiman, K. G. (1993). The retinoblastoma gene: Role in cell cycle control and cell differentiation. The FASEB Journal, 7(10), 841–845. https://doi.org/10.1096/fasebj.7.10.8393817 This gene is located on chromosome 13q14 and works as a tumour suppressor to stop cells from dividing uncontrollably. It has two copies (alleles), and either the loss or mutation of both is necessary for tumour formation.
This mechanism follows Knudson’s “Two-Hit Hypothesis”, which explains how the disease process occurs.
Hereditary or Germline Retinoblastoma:
In this type, the RB1 mutation is present in all cells of the body from birth. Generally, one mutated copy of the gene is passed down from a parent. Later, mutations occur in the second one as well, eventually leading to tumour formation. This is a more dangerous form of retinoblastoma as it affects both eyes and is also associated with other types of cancers in the body.
Non-Hereditary or Sporadic Retinoblastoma:
This is a less severe type of cancer that usually affects one eye and is not inherited from parents. In this case, both RB1 mutations happen in retinal cells only. Hence, other cells of the body are spared from cancer.
Retinoblastoma Symptoms
The most common sign of retinoblastoma is that the eyes of the child do not look normal. One or both eyes may appear hazy, abnormally protruding, or have a whitish colour. The main symptoms include:
- Leukocoria: When light enters a normal eye, the pupil looks red. However, in a patient with retinoblastoma, the pupil appears white when light shines into it.3Abramson, D. H., Frank, C. M., Susman, M., Whalen, M. P., Dunkel, I. J., & Boyd, N. W. III. (1998). Presenting signs of retinoblastoma. The Journal of Pediatrics, 132(3), 505–508. https://doi.org/10.1016/S0022-3476(98)70028-9 4Bukhari, S., Aziz-ur-Rehman, Bhutto, I. A., & Qidwai, U. (2011). Presentation pattern of retinoblastoma. Pakistan Journal of Ophthalmology, 27(3). https://doi.org/10.36351/pjo.v27i3.483
- Squint, or Strabismus, a condition in which there is an abnormally aligned axis of the eyes during movement.
- Proptosis, or a protruding eye, which appears to be coming out of the orbit.
- Nystagmus, or repetitive eye movements without control
- Eye pain, due to an increase in intraocular pressure.
- Redness, without any visible infection due to increased blood supply in the area.
- Poor vision, as the tumour obstructs normal vision.
Also, less common symptoms can include sensitivity to light (photophobia), enlarged pupils, and swelling around the eyes.
(Image by Swathi Kaliki, published in Community Eye Health Journal, licenced under CC BY-NC 2.0)
(Image courtesy: International Centre for Eye Health, licenced under CC BY-NC 2.0)
Retinoblastoma Diagnosis
If a doctor suspects cancer in your child, they will start with a detailed history and perform an eye exam. Following this, they will advise various imaging and genetic tests to confirm the diagnosis. These tests may include:
Eye Examination:
Eyes are examined for any abnormal appearance, redness, proptosis (bulging) and squint. The pupillary light reflex is checked to rule out other conditions. Less harmful conditions which mimic retinoblastoma and don’t raise further suspicion are ruled out at this stage.
Indirect Ophthalmoscopy:
In case of any uncertainty, it is mandatory to perform indirect ophthalmoscopy with pressure on the sclera.5Pandey, A. N. (2014). Retinoblastoma: An overview. Saudi Journal of Ophthalmology, 28(4), 310–315. https://doi.org/10.1016/j.sjopt.2013.11.001 An ophthalmoscope is a tool that doctors use to see the retina and other internal structures of the eye. It is a gold standard method which enables the successful detection of almost 95% of cancers.
Imaging Techniques:
For further evaluation, multiple imaging modalities are currently in use, such as:
- Ultrasonography: Also called a B-scan, it is one of the first investigations to be performed. An ultrasound machine uses high-frequency sound waves to get a look at the inner structures of the eye. On a B-scan, retinoblastoma appears as a round mass typically with calcification or retinal detachment.
- MRI: After spotting the tumour with an ultrasound, the next step is to locate the extent of the tumour and do the staging. Staging of the tumour is necessary to start treatment and is done using MRI, which stands for Magnetic Resonance Imaging. It shows the exact size of the tumour and any invasion in nearby areas, like the choroid plexus, orbital structures and optic nerve.
- CT-Scan: If MRI is unavailable, a CT scan is the method of choice to classify the tumour. Moreover, it also indicates the deposition and location of calcium crystals in the tumour. Since it uses high doses of radiation and can activate cancers in young children, its use is not much preferred in routine.6Jenkinson, H. (2015). Retinoblastoma: Diagnosis and management—the UK perspective. Archives of Disease in Childhood, 100(11), 1070–1075
Genetic Testing:
Though genetic testing is not necessary for every case, doctors may recommend it when they suspect a hereditary form of cancer. It includes using a blood or saliva sample to look for mutations in DNA and determine whether the disease is inherited or not. Furthermore, it helps in the screening of family members and genetic counselling.
Lumbar Puncture & Bone Marrow Biopsy:
These investigations are not part of the routine. But sometimes, there is a suspicion of the spread of cancer to the nervous system or bone marrow. This is an alarming situation requiring a thorough analysis of cerebrospinal fluid or bone marrow to check the possibility of cancer cells.7Bakhshi, S., Meel, R., Kashyap, S., & Sharma, S. (2011). Bone marrow aspirations and lumbar punctures in retinoblastoma at diagnosis: Correlation with IRSS staging. Journal of Pediatric Hematology/Oncology, 33(5), e182–e185. https://doi.org/10.1097/MPH.0b013e3182103f5c
Bone Scan:
In hereditary cases, there is a significant risk of cancer in other body areas. For this reason, a bone scan is an important additional investigation tool to effectively screen for the presence of Osteosarcomas, a type of bone cancer.
(image courtesy of ScienceDirect, licensed under CC BY-NC-ND 3.0)
(image courtesy of ScienceDirect, licensed under CC BY-NC-ND 3.0)
Retinoblastoma Stages
The stage of cancer describes its extent and invasion of surrounding structures. Thus, it is a common method for selecting appropriate treatment options and assessing prognosis.8Fabian, I. D., Reddy, A., & Sagoo, M. S. (2018). Classification and staging of retinoblastoma. Community Eye Health, 31(101), 11–13. PMCID: PMC5998397. Usually, doctors divide it into two main groups:
- Intraocular retinoblastoma: If the cancer is limited to the eye.
- Extraocular retinoblastoma: If the cancer has spread outside the eye.
Classification of Intraocular Retinoblastoma (ICRB Staging System):
It classifies intraocular tumour into 5 stages labelled A through E, based on the size and extent.
| Group | Description |
|---|---|
| A | A tumour with a size less than 3mm that is confined to the retina. |
| B | A tumour with a size of more than 3mm but still in the retina. |
| C | Well-defined but with a little seeding in the vitreous or subretinal space. |
| D | Poorly defined, with widespread seeding in the vitreous or subretinal space. It may cause retinal detachment as well. |
| E | A very large tumour that is blocking the front part of the eye almost completely. It also causes other symptoms, like glaucoma. |
Classification of Extraocular Retinoblastoma (IRSS Staging System):
This staging system is used when the tumour has spread beyond the eye. Specifically, if the tumour invades the optic nerve, choroid plexus, or orbit, or if there is distant metastasis, the extent of surgery will be determined based on this method.
| Stages | Classification |
| Stage 0 | Only conservative management, no enucleation |
| Stage 1 | Enucleation, complete resection of tumour with histopathological examination |
| Stage 2 | Enucleation with microscopic residual tumour |
| Stage 3 | Regional extension IIIa: Overt orbital disease. IIIb: Preauricular or cervical lymph node involvement. |
| Stage 4 | Metastatic Disease IVa: Hematogenous metastasis without CNS involvement. IVb: CNS involvement, including intracranial or spinal subarachnoid disease. |
Reese-Ellsworth Classification:
Researchers created this system in the 1960s. It helps predict if the eye can be saved with external beam radiotherapy. Although newer treatments have reduced their use, they still provide historical context for retinoblastoma management.
TNM Staging:
The American Joint Committee on Cancer (AJCC) created this system to provide a clear anatomical description of tumour size, regional lymph node involvement, and distant metastasis.9TNM8: The updated TNM classification for retinoblastoma. (2018). Community Eye Health, 31(101), 34. PMID: 29915471; PMCID: PMC5998398. The components include:
- T (tumour): The size and extent of the primary tumour, both within and outside the eye.
- N (Node): Involvement of regional lymph nodes.
- M (Metastasis): The presence of distant metastasis.
- H (Heritability): Genetic predisposition, which indicates the presence of germline mutations.
Treatment of Retinoblastoma
Management of retinoblastoma is a long process requiring patience and adherence to the doctor’s instructions. Children with cancer undergo evaluation by a multi-disciplinary team consisting of an oncologist, an ophthalmologist, and a radiation oncologist to plan the treatment. The main goals of treatment are:
- Save the life of the patient.
- Preserve vision and the eye as much as possible.
- Decrease the risk of recurrence of cancer later in life.
Commonly used treatment methods include:
1. Cryotherapy:
Cryo or cold therapy involves applying a cryoprobe near the retina. It uses liquid nitrogen to lower the temperature of the tissue, hence freezing and killing the cancer cells. This helps treat small tumours only (less than 4 disc diameters), located in the front of the eye.10Ancona-Lezama, D., Dalvin, L. A., & Shields, C. L. (2020). Modern treatment of retinoblastoma: A 2020 review. Indian Journal of Ophthalmology, 68(11), 2356–2365. https://doi.org/10.4103/ijo.IJO_721_20
2. Thermotherapy:
Thermotherapy in cancer means the application of heat to raise the temperature of the tissue, hence killing the cancer cells. The focus of the traditionally used Argon laser was the destruction of blood vessels that supply nutrients to the tumour cells. Now, the diode laser has replaced this approach. This modern method uses infrared light to heat the tumour’s surface and destroy cancer cells directly.
3. Chemotherapy:
It involves using drugs to damage or kill the cancer cells by damaging their DNA. It enhances the outcomes of other methods like radio or cryotherapy when used as an adjuvant, i.e., additional treatment.
To achieve better results, most doctors follow a three-drug regimen that includes vincristine, etoposide, and carboplatin. They either use injections or oral pills to deliver the drug into the bloodstream, inject it locally into the vitreous humour (a gel-like substance filling the eyeball), or administer it through cannulation of the ophthalmic vein.
4. Radiation Therapy:
This cancer treatment employs high-energy radiation to eliminate cancer cells. Since radiation is harmful and has the potential to stimulate cancer formation in other areas of the body, its use is limited.
External Beam Radiation Therapy helps to destroy tumours by directing X-ray beams at the damaged area from an external source, such as a machine, whereas the latest methods involve the use of a device that is implanted behind the eye, near the tumour. The radiation emitted from it helps to kill the damaged cells.
5. High-dose Chemotherapy with Stem Cells:
Along with cancer cells, chemotherapy also destroys some healthy cells, specifically those which form blood. To counter this, doctors reinfuse a pool of stem cells into the patient after treatment, thus helping the bone marrow restore blood cell count.
6. Surgery:
The surgical treatment for retinoblastoma is enucleation, i.e., removal of the eyeball along with a portion of the optic nerve. Unfortunately, it is the only surgical option and doctors perform it only when the tumour is massive in size, unresponsive to other treatments, has little to no chance of preserving vision, and when leaving the eyeball can lead to lethal outcomes. Later, they replace the space with a prosthetic (artificial) eye.
(Image courtesy of Wikimedia, licenced under CC BY-SA 4.0)
Retinoblastoma Prognosis
The outcome of cancer depends on the time of detection and stage of disease. Moreover, skilled professionals who can choose the best treatment options also play a vital role. According to the National Institutes of Health, in most first-world countries with modern diagnostic facilities and treatment, the five-year survival rate is approximately 95% for small to medium-sized tumours.11Ishaq, H., & Patel, B. C. (2023, August 8). Retinoblastoma. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK545276/. However, without treatment, the disease often spreads locally and to distant areas, eventually leading to death within two years.
Poor prognostic factors include:
- A large tumour occupying most of the eye
- Involvement of the optic nerve, the choroid plexus, or the orbital structures
- Extraocular spread, particularly distant metastasis to the brain, bones and lungs.12Gündüz, K., Müftüoglu, O., Günalp, İ., Ünal, E., & Taçyıldız, N. (2006). Metastatic retinoblastoma: Clinical features, treatment, and prognosis. Ophthalmology, 113(9), 1558–1566. https://doi.org/10.1016/j.ophtha.2006.03.039
- Older age at diagnosis
Keynote: Even after treatment, most patients require lifelong surveillance. This is because the genetic mutations in the RB1 gene, which are responsible for retinoblastoma, significantly increase the risk of relapse or tumour formation in other parts of the body.
Retinoblastoma Differential Diagnosis
Some eye conditions that mimic retinoblastoma due to the appearance of white reflex and can be a cause of worry on initial eye exam include:
- Cataracts
- Coats’ Disease
- Retinopathy of prematurity (ROP)
- Toxocariasis
- Persistent fetal vasculature
- Toxoplasmosis of the eye
Retinoblastoma vs. Cataract
A cataract is the presence of opacity in the lens. Children can have it either from birth or develop later in the early years of life. While retinoblastoma is a lethal cancer, a cataract is a far less dangerous local condition.
Leukocoria or white reflex appears in both conditions but cataracts mainly present with blurry or dim vision in contrast to retinoblastoma. Moreover, treatment for cataracts includes removing the lens only, followed by artificial lens placement, whereas retinoblastoma needs the removal of the whole eyeball with a part of the optic nerve.
Conclusion
A tumour of immature cells of the retina is a serious childhood cancer that can lead to loss of vision and death if left untreated. It occurs due to a defective RB1 gene and can be present at birth or develop in the initial years of life. Apart from children, people of any age group can also be affected, though it is uncommon.
A patient with retinoblastoma is usually a child whose parents notice an unusual appearance in one or both eyes. An eye exam, indirect ophthalmoscopy, and B-scan help in the initial diagnosis, while MRI helps stage the disease. Fortunately, it is rare, and treatment options are available, which help preserve vision and save lives. Early detection and proper management significantly improve outcomes and enhance the quality of life.
Refrences
- 1Rao, R., & Honavar, S. G. (2017). Retinoblastoma. Indian Journal of Pediatrics, 84(12), 937–944. https://doi.org/10.1007/s12098-017-2395-0
- 2Wiman, K. G. (1993). The retinoblastoma gene: Role in cell cycle control and cell differentiation. The FASEB Journal, 7(10), 841–845. https://doi.org/10.1096/fasebj.7.10.8393817
- 3Abramson, D. H., Frank, C. M., Susman, M., Whalen, M. P., Dunkel, I. J., & Boyd, N. W. III. (1998). Presenting signs of retinoblastoma. The Journal of Pediatrics, 132(3), 505–508. https://doi.org/10.1016/S0022-3476(98)70028-9
- 4Bukhari, S., Aziz-ur-Rehman, Bhutto, I. A., & Qidwai, U. (2011). Presentation pattern of retinoblastoma. Pakistan Journal of Ophthalmology, 27(3). https://doi.org/10.36351/pjo.v27i3.483
- 5Pandey, A. N. (2014). Retinoblastoma: An overview. Saudi Journal of Ophthalmology, 28(4), 310–315. https://doi.org/10.1016/j.sjopt.2013.11.001
- 6Jenkinson, H. (2015). Retinoblastoma: Diagnosis and management—the UK perspective. Archives of Disease in Childhood, 100(11), 1070–1075
- 7Bakhshi, S., Meel, R., Kashyap, S., & Sharma, S. (2011). Bone marrow aspirations and lumbar punctures in retinoblastoma at diagnosis: Correlation with IRSS staging. Journal of Pediatric Hematology/Oncology, 33(5), e182–e185. https://doi.org/10.1097/MPH.0b013e3182103f5c
- 8Fabian, I. D., Reddy, A., & Sagoo, M. S. (2018). Classification and staging of retinoblastoma. Community Eye Health, 31(101), 11–13. PMCID: PMC5998397.
- 9TNM8: The updated TNM classification for retinoblastoma. (2018). Community Eye Health, 31(101), 34. PMID: 29915471; PMCID: PMC5998398.
- 10Ancona-Lezama, D., Dalvin, L. A., & Shields, C. L. (2020). Modern treatment of retinoblastoma: A 2020 review. Indian Journal of Ophthalmology, 68(11), 2356–2365. https://doi.org/10.4103/ijo.IJO_721_20
- 11Ishaq, H., & Patel, B. C. (2023, August 8). Retinoblastoma. In StatPearls. StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK545276/.
- 12Gündüz, K., Müftüoglu, O., Günalp, İ., Ünal, E., & Taçyıldız, N. (2006). Metastatic retinoblastoma: Clinical features, treatment, and prognosis. Ophthalmology, 113(9), 1558–1566. https://doi.org/10.1016/j.ophtha.2006.03.039

