Nystagmus present since birth is known as congenital nystagmus, which is the involuntary to and fro movement of eyes in either horizontal or vertical direction. Congenital nystagmus commonly manifests in both eyes. Since it is a rare ocular disorder, congenital nystagmus affects 17 per 10000 individuals.1Hertle, Richard W., Cecily Kelleher, David Bruckman, Neil McNinch, Isabel Ricker, Rachida Bouhenni, and Kelly Wiseman. “Analysis of anomalous head posturing in patients with infantile nystagmus syndrome.” Journal of American Association for Pediatric Ophthalmology and Strabismus 25, no. 3 (June 2021): 145.e1–145.e5. http://dx.doi.org/10.1016/j.jaapos.2021.02.009.
What is Congenital Nystagmus?
Congenital nystagmus (also known as infantile nystagmus) comprises rapid “to and fro” rhythmic movements of eyes that begin shortly after birth, having variable ranges of frequency and amplitude of oscillations ranging from 2 to 15 Hertz. It often presents at around six weeks to 3 months of age. Congenital nystagmus, although painless, is a permanent condition.
However, prescribed medications and other therapeutic interventions can manage the associated symptoms. Moreover, while nystagmus itself is harmless, it can be associated with serious health conditions. Hence, a complete evaluation by ophthalmologists is mandatory to identify the possible causes and maximize visual development.
Congenital nystagmus is one of the three early-onset types of nystagmus during infancy. The retina, the visual cortex of the occipital lobe in the brain, optic nerve, optic chiasm, and lateral geniculate bodies are an integral part of the visual pathway. Hence, any dysfunction or abnormality in components of the visual pathway may lead to impaired vision and uncontrolled eye movements.2Kelly, John P., Kristina Tarczy-Hornoch, James O. Phillips, and Avery H. Weiss. “A reduced visual pathway response in infantile nystagmus syndrome.” Journal of American Association for Pediatric Ophthalmology and Strabismus 25, no. 1 (February 2021): 9.e1–9.e6. http://dx.doi.org/10.1016/j.jaapos.2020.09.005.
Additionally, it is important to rule out any structural abnormalities in the cornea or eye lens due to a developmental issue which can give rise to congenital nystagmus.
Nystagmus Causes
Failure of the brain, the vestibular (balance) system and the eyes to work together results in nystagmus. Therefore, congenital nystagmus could be associated with a neurological defect, a problem in the eyes or a problem in the inner ear. In some incidents, parents can pass nystagmus to their children, however often the exact cause is unknown.3Wang P, Ya P, Li D, Lv S, Yang D. Nystagmus with pendular low amplitude, high-frequency components (PLAHF) in association with retinal disease. Strabismus. 2020;28:3–6.
One type of nystagmus called idiopathic nystagmus has no apparent cause and is mostly rare. However, it is important to rule out any developmental abnormalities in the eye as well.
Moreover, the most common risk factors and causes associated with congenital nystagmus are as follows:
Albinism
Nystagmus is present with both types of albinism, occulocutenous albinism and ocular albinism.
Optic Nerve Hypoplasia
Underdevelopment of the optic nerves leads to hypoplasia of the nerves, resulting in unclear vision due to improper functioning. Since the optic nerve plays a significant role in the visual pathways it results in nystagmus due to misalignment of the visual pathway and reduced visual perception.
Aniridia
The absence of iris i.e. coloured part of the eye surrounding the pupil. It can be congenital and acquired as well. Aniridia is associated with congenital nystagmus and reduced visual acuity due to foveal hypoplasia (incomplete development of the foveal pit). Fovea is responsible for central sharp vision.
Retina Coloboma
The congenital absence of eye tissues may lead to vision loss and is associated with nystagmus.
Severe Refractive Error
The disorders related to eye focusing capability such as nearsightedness. Since the eye tries to compensate for the visual disturbance by rapid eye movement. High refractive error or even astigmatism can result in nystagmus as a result of the body’s compensatory mechanism
Some additional causes and conditions associated with congenital nystagmus include:
- Vitamin deficiency (Vitamin B12)
- Fetal alcohol syndrome
- Brain tumour
- Central nervous system disorders such as multiple sclerosis
- Carotid artery stenosis leading to stroke
- Trauma
- Congenital rubella syndrome
Types of Congenital Nystagmus
Based on vision, congenital nystagmus has two main subtypes, children with abnormal vision (sensory nystagmus) versus children having normal vision (motor nystagmus)
- The eyes of children with abnormal vision cannot send feedback to the brain. They are unable to send back a clear message about what is visible to them. This visual impairment may range from moderate to severe levels. Hence, this condition is also known as ‘sensory nystagmus’ manifesting the inability of the eyes to sense ‘vision’. Manifesting at 2-3 months of child age, sensory nystagmus continues throughout the life of the affected individual.4Matsuda H, Tanzawa Y, Sekine T, Matsumura T, Saito S, Shindo S, et al. Congenital membranous stapes footplate producing episodic pressure-induced perilymphatic fistula symptoms. Front Neurol. 2020;11:585747.
- Congenital motor nystagmus involves impaired motor control in children having normal sight where the brain is weak at performing motor control over eye movements.
Furthermore, three additional types of congenital nystagmus include:
Congenital Nystagmus with Albinism:
Albinism has a strong association with congenital nystagmus and can be seen in both of the following conditions.
Ocular Albinism
Ocular albinism is a genetic condition with an X-linked inheritance pattern affecting the GPR-143 gene. Unlike other forms of albinism, ocular albinism affects the colouring within the eyes only, involving the iris (coloured part) and the retina (the light-sensitive part at the back of the eye). Owing to the reduction in pigment production, ocular albinism presents with reduced vision, congenital nystagmus, and photophobia (light sensitivity).5Thomas, M.G., Zippin, J. and Brooks, B.P., 2023. Oculocutaneous albinism and ocular albinism overview. It is more common in males and rarely manifests in females.
Occulocuteanous Albinism
It is the most common form of hypopigment disorder involving defective melanin synthesis. Occulocuteanous albinism is an autosomal recessive disorder and can present equally in both males and females. It affects the coloring of skin, hair, and eyes and presents as white skin, white hair, pale eyelashes, and eyebrows. Occulocutenous albinism also affects the eyes, resulting in nystagmus (horizontal), reduced vision, photophobia, and strabismus (crossed eyes).
Spasmus Nutans:
Spasmus nutans is a type of nystagmus that often occurs between six months and three years of age. It is a benign condition and is self-resolving. It improves by itself without requiring any medical intervention when a child crosses the 2-8 years of age limit.6Jin, Soohwa, Sung-Eun Park, Dongju Won, Seung-Tae Lee, Sueng-Han Han, and Jinu Han. “TUBB3 M323V Syndrome Presents with Infantile Nystagmus.” Genes 12, no. 4 (April 15, 2021): 575. http://dx.doi.org/10.3390/genes12040575. Sapsmus nutans presents with the triad of head nodding, ocular oscillations, and anomalous head position.7Raghuraman, T.S. and Shukla, K.M., 2001. Spasmus nutans. Medical Journal Armed Forces India, 57(3), pp.243-244.
Latent & Manifest Latent Nystagmus:
Latent nystagmus, as the name suggests, is hidden and is only observed in the alternative eye when the other eye is covered. The uncovered eye manifests as two phases: the slow phase of nystagmus, where the eyeball jerks in the direction of the nose, while the fast phase moves towards the uncovered eye. However, conjugate beating is observed in the covered eye. The main rationale behind latent nystagmus is the compensation response of eyes due to unequal visual input. This condition is benign and is rarely associated with neurological defects.8Liu, G.T., Volpe, N.J. and Galetta, S.L., 2018. Liu, Volpe, and Galetta’s neuro-ophthalmology E-book: diagnosis and management. Elsevier Health Sciences.
On the other hand, manifest latent nystagmus has continuous presentation and is characterized by worsening following occlusion of one eye.
Nystagmus Symptoms
One of the major symptoms of nystagmus include uncontrolled rapid eye movement. These movements may be horizontal, vertical, upward, or circular. Frequency can vary between high and low ranges and often involves both eyes.9Duraiswamy, Ashwath, and Babilu C.O. “Senior-Loken syndrome: A case report.” Karnataka Pediatric Journal 35 (September 9, 2020): 57–60. http://dx.doi.org/10.25259/kpj_12_2020.
Additionally, other symptoms associated with congenital nystagmus include the following:
- Blurry vision (most common)
- Motion sickness
- Fatigue
- Dizziness after performing any visual tasks
- Ocillopsia (shaky vision)
- Head tilting
- Improper postural adaptations
- Head bobbing
- Clumsiness
- Asthenopia (eye fatigue/ strain)
- Poor coordination
- Inaccurate spatial judgment (improper visualization pattern)
- Light sensitivity
Vertigo with Nystagmus
Vertigo with nystagmus is a rare symptom associated with congenital nystagmus. However, the individuals who get affected by nystagmus in the latter phase of life feel spinning during vertigo spells.
A temporary vertigo condition (benign paroxysmal positional vertigo) involves damage to the inner ear, causing repetitive sessions of positional vertigo.
The inner ear senses the movement and position of the head. Meanwhile, in the case of BPPV (benign paroxysmal positional vertigo), small crystals in semicircular ducts of fluid-filled chambers can irritate nerve endings. This incidence can become a reason for positional vertigo.10Dai, Bing, Kwang Meng Cham, and Larry Allen Abel. “Velocity Discrimination in Infantile Nystagmus Syndrome.” Investigative Opthalmology & Visual Science 62, no. 10 (August 30, 2021): 35. http://dx.doi.org/10.1167/iovs.62.10.35.
How is Congenital Nystagmus Diagnosed?
As a complex ocular oscillatory condition, it becomes very challenging to evaluate congenital nystagmus. Generally, it is not diagnosed at birth, but between the age limit of 6 weeks-6 months.11Cohen, Adam B., and Brain V. Nahed. “The Digital Neurologic Examination.” Digital Biomarkers 5, no. 1 (April 26, 2021): 114–26. http://dx.doi.org/10.1159/000515577. It may be an isolated disorder or present with a broad range of visual, systematic, or sensory abnormalities.
Therefore, different healthcare professionals may collaborate and perform additional tests related to eye diseases, brain conditions, and inner ear conditions. For this purpose, a multidisciplinary team involving expert neurologists, ophthalmologists, and audiologists is needed.
Clinical Examination:
- A detailed examination will be conducted, considering the frequency, amplitude, directions of movement, onset age, and eye movement recordings.
- Disease history, including progression and improvement.
- Childbirth records like prematurity or prenatal course exposures (infections and medications).
- Growth and developmental history, including growth charts and other milestones.
- General physical examination including skin color, head circumference, circumference for age, kidney problems, and abnormal head posture.
- Comprehensive family history.
Clinical Tests:
To establish a diagnosis of congenital nystagmus, a range of testing takes place, including:
CT Scan & MRI
These tests exclude organic and neurological reasons for congenital nystagmus.
Slit-Lamp Exam
A slit-lamp exam evaluates sensory defect nystagmus, differentiating optic nerve hypoplasia, ocular albinism, and congenital cataracts.

Visual Acuity
This test is performed to evaluate two parameters-vision clarity and sharpness of sight. The infant’s normal visual acuity ranges from 20/200 to 20/400. The commonly employed ways to assess visual acuity in infants include:
- Light response: The infant will blink when exposed to a bright light source.
- Pupillary reaction: The changing diameter of the pupil is measured in response to bright light.
- Ability to follow an object
- Visually evoked response (VER) testing: An electric monitor is attached to the infant’s head while a bright light is shown to the eyes to stimulate a response. The monitor then records the electrical activity of the brain.
Color Vision
The test evaluates the presence of achromatopsia by birth or eye squinting in bright light, manifesting light sensitivity.
Full-Field Electroretinography (ERG)
ERG involves testing on infants by utilizing skin-type electrodes or DTL (Dawson, Trick, and Litzkow). Exhibiting light and dark adaptations of ERG indicate the early onset of retinal damage in childhood. Other findings of this test include the following:
- Reduced amplitude of ERG- for retinitis pigmentosa (group of disorders affecting retina)
- Electronegative- ERG- for X-linked retinoschisis (area of a retina splits into two layers)
Macula Optical coherence tomography (OCT)
OCT is a device that uses low-frequency light into the eyes and uses its reflections to take images of the retina. In infants, portable OCT devices can be used, which can aid in diagnosing retinoschisis, aniridia, and other retinal dystrophies, sometimes associated with congenital nystagmus.
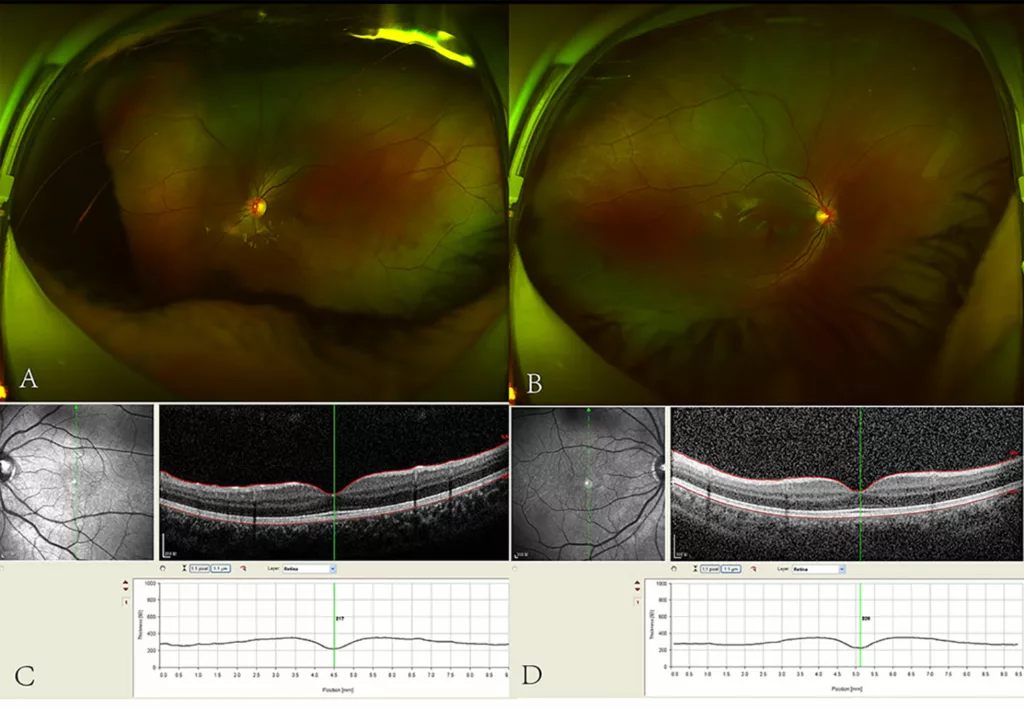
Source: Liu, F., Wang, M., Liao, M., Liu, L. and Jiang, X., 2023. X-linked FRMD7 gene mutation in idiopathic congenital nystagmus and its role in eye movement: A case report and literature review. Frontiers in Ophthalmology, 2, p.1080869. https://www.frontiersin.org/files/Articles/1080869/fopht-02-1080869-HTML-r2/image_m/fopht-02-1080869-g001.jpg
Intraocular Pressure (IOP) Measurements
This test measures the pressure inside the eye, which can be relevant to diagnosing and managing various eye conditions. The interpretation of IOP measurements takes into account factors like the patient’s age, axial length of the eye, and corneal thickness.
Eye Movement Recordings
This procedure involves recording eye movements using techniques like video-nystagmography and electronystagmography for observations and interpretations. These methods provide detailed information about the characteristics and patterns of nystagmus, helping diagnose and assess the condition.
Genetic Tests
These tests involve the segregation of parental genes for confirmation. It consists of comprehensive genetic testing like:
- Whole exome sequencing (WES): Analyzes all the protein-coding regions of genes to detect mutations.
- Whole genome sequencing (WGS): Provides a complete overview of the genetic makeup, including non-coding regions, to identify genetic variations.
Metabolic Testing
Metabolic testing considers the following clinical disorders:
- Carbohydrate-deficient glycoprotein syndromes
- Peroxisomal biogenesis disorders (PBDs)
- Hypomyelination leukodystrophy
Nystagmus Treatment
The treatment for congenital nystagmus differs according to associated medical complications. Some types of congenital nystagmus disappear on their own with time. However most forms are permanent, and the use of prescription glasses, surgery and medicines can minimise it.
Moreover, such approaches do not resolve nystagmus, they facilitate the procedure of having a clear vision with a reduction in the frequency of eye movements.
Medication for Nystagmus
Congenital nystagmus symptoms require various medications. These medications have reported a reduction in the intensity of congenital nystagmus. Among these, the clinically tested medications are as follows:
- Memantine (NMDA receptor antagonist): It protects nerve cells by blocking glutamate. It usually improves vision by 0.15 points.
- Gabapentin (anti-seizure): Gabapentin helps in calming excited neurons, mimicking GABA (gamma-aminobutyric acid). It improves vision by 0.09 points.
Cannabis and baclofen have also been observed to show some effects on eye movements but have not been suggested for clinical prescriptions due to a lack of clinical trial evidence.
In addition to this, other treatment options include the application of:
- Vision therapy or occupational therapy
- Syntonic phototherapy (causes retinal stimulation leading to improved visual)
- Visual tools, including telescopes or magnifying glasses (reduce eye strain)
Surgical Treatment:
The basic purpose of surgeries is to readjust eye muscles involved in eye movements. However, surgical treatments do not cure the condition. They only make an individual capable of keeping their head in a comfortable position while limiting eye movements. 12Gómez-Mariscal, Marta, P. Hernández-Martínez, J. M. Rodríguez-del Valle, M. Ruiz-Guerrero, C. Márquez-González, and J. M. Rodríguez-Sánchez. “Consecutive strabismus after infantile nystagmus syndrome surgery and potential risk factors.” Graefe’s Archive for Clinical and Experimental Ophthalmology 258, no. 7 (April 20, 2020): 1549–54. http://dx.doi.org/10.1007/s00417-020-04686-9.
Eye Muscle Surgeries
- Strabismus Surgery: An example is Strabismus surgery, which involves the operation of eye-controlling muscles. Consequently, this surgery results in an improvement in head position.
- Kestenbaum Surgery: Kestenbaum surgery is among the earliest surgical procedures involving recession and extraocular muscle resection.
- Artificial Divergence Surgery: It involves the recession of both medial rectus muscles. Combining both surgeries (Kestenbaum and artificial divergence) results in better effects on vision versus performing each one separately.
- Vision Correction Surgery: Nearsightedness, one of the prominent symptoms of congenital nystagmus, can be improved by laser vision correction surgery like LASIK.
Prognosis
The majority of children having congenital nystagmus make their lives easy with the help of occupational therapies, mobility experts, orientations and mobility experts in the early periods of life.
However, other adaptations these individuals follow to improve vision involve accommodations like visual problems, magnifying devices, increased lighting, and large print books. Getting help from low vision specialists facilitates children to live an active and normal life.
Prevention
Currently, congenital nystagmus is hard to predict or prevent before birth. However, in regards to preventing the condition from worsening and improving your quality of life, the following tips can be helpful.13Jung I, Shin JH, Kim J. Gaze-evoked nystagmus associated with valproic acid-induced lamotrigine toxicity. Clin Neurol Neurosurg. 2020;196:106013.
- Take regular breaks while using digital gadgets for longer periods.
- Practice good body posture.
- Join sports groups or individuals with congenital nystagmus to share experiences and find emotional support.
- Use bright lighting at home or in the office.
Conclusion
Congenital nystagmus can affect an individual’s vision, sense of equilibrium, and visual acuity. It is not possible to cure and eliminate the condition. However, therapeutic interventions can manage the associated symptoms and improve visual functions to an extent. Therefore, an effective management plan can help you control congenital nystagmus and enjoy good visual performance.
Refrences
- 1Hertle, Richard W., Cecily Kelleher, David Bruckman, Neil McNinch, Isabel Ricker, Rachida Bouhenni, and Kelly Wiseman. “Analysis of anomalous head posturing in patients with infantile nystagmus syndrome.” Journal of American Association for Pediatric Ophthalmology and Strabismus 25, no. 3 (June 2021): 145.e1–145.e5. http://dx.doi.org/10.1016/j.jaapos.2021.02.009.
- 2Kelly, John P., Kristina Tarczy-Hornoch, James O. Phillips, and Avery H. Weiss. “A reduced visual pathway response in infantile nystagmus syndrome.” Journal of American Association for Pediatric Ophthalmology and Strabismus 25, no. 1 (February 2021): 9.e1–9.e6. http://dx.doi.org/10.1016/j.jaapos.2020.09.005.
- 3Wang P, Ya P, Li D, Lv S, Yang D. Nystagmus with pendular low amplitude, high-frequency components (PLAHF) in association with retinal disease. Strabismus. 2020;28:3–6.
- 4Matsuda H, Tanzawa Y, Sekine T, Matsumura T, Saito S, Shindo S, et al. Congenital membranous stapes footplate producing episodic pressure-induced perilymphatic fistula symptoms. Front Neurol. 2020;11:585747.
- 5Thomas, M.G., Zippin, J. and Brooks, B.P., 2023. Oculocutaneous albinism and ocular albinism overview.
- 6Jin, Soohwa, Sung-Eun Park, Dongju Won, Seung-Tae Lee, Sueng-Han Han, and Jinu Han. “TUBB3 M323V Syndrome Presents with Infantile Nystagmus.” Genes 12, no. 4 (April 15, 2021): 575. http://dx.doi.org/10.3390/genes12040575.
- 7Raghuraman, T.S. and Shukla, K.M., 2001. Spasmus nutans. Medical Journal Armed Forces India, 57(3), pp.243-244.
- 8Liu, G.T., Volpe, N.J. and Galetta, S.L., 2018. Liu, Volpe, and Galetta’s neuro-ophthalmology E-book: diagnosis and management. Elsevier Health Sciences.
- 9Duraiswamy, Ashwath, and Babilu C.O. “Senior-Loken syndrome: A case report.” Karnataka Pediatric Journal 35 (September 9, 2020): 57–60. http://dx.doi.org/10.25259/kpj_12_2020.
- 10Dai, Bing, Kwang Meng Cham, and Larry Allen Abel. “Velocity Discrimination in Infantile Nystagmus Syndrome.” Investigative Opthalmology & Visual Science 62, no. 10 (August 30, 2021): 35. http://dx.doi.org/10.1167/iovs.62.10.35.
- 11Cohen, Adam B., and Brain V. Nahed. “The Digital Neurologic Examination.” Digital Biomarkers 5, no. 1 (April 26, 2021): 114–26. http://dx.doi.org/10.1159/000515577.
- 12Gómez-Mariscal, Marta, P. Hernández-Martínez, J. M. Rodríguez-del Valle, M. Ruiz-Guerrero, C. Márquez-González, and J. M. Rodríguez-Sánchez. “Consecutive strabismus after infantile nystagmus syndrome surgery and potential risk factors.” Graefe’s Archive for Clinical and Experimental Ophthalmology 258, no. 7 (April 20, 2020): 1549–54. http://dx.doi.org/10.1007/s00417-020-04686-9.
- 13Jung I, Shin JH, Kim J. Gaze-evoked nystagmus associated with valproic acid-induced lamotrigine toxicity. Clin Neurol Neurosurg. 2020;196:106013.

