Sarcoidosis of the lungs or Pulmonary sarcoidosis is a type of sarcoidosis that specifically affects the lungs, where clusters of inflammatory cells known as granulomas form in lung tissue. These granulomas can interfere with normal lung function, leading to symptoms like persistent cough, shortness of breath, and chest pain. The disease is not only limited to the lungs but also affects lymph nodes. Rarely does the disease involve the eyes, heart, nervous system, and the skin.1American Lung Association. Learn about sarcoidosis. https://www.lung.org/lung-health-diseases/lung-disease-lookup/sarcoidosis/learn-about-sarcoidosis/
The exact cause of sarcoidosis is unknown, but it is thought to result from an abnormal immune response, potentially triggered by environmental or genetic factors. While some cases are mild and resolve on their own, others may lead to lung scarring (fibrosis) and chronic respiratory issues. Pulmonary sarcoidosis requires close monitoring, and in severe cases, treatment may include medications to reduce inflammation or, in advanced stages, lung transplantation.
Sarcoidosis is fairly uncommon, and its prevalence differs across different geographical locations. For instance, sarcoidosis occurs in 1-5 per 1,00,000 individuals in Southeast Asia, whereas the incidence sores to 140-150 per 1,00,000 in the Western parts of the world.2Arkema, E. V., & Cozier, Y. C. (2020). Sarcoidosis epidemiology: recent estimates of incidence, prevalence and risk factors. Current opinion in pulmonary medicine, 26(5), 527–534. https://doi.org/10.1097/MCP.0000000000000715
Symptoms of Sarcoidosis in Lungs
Sarcoidosis is a multi-systemic disease that results in non-caseating granulomas in different body parts. It has not been possible to know exactly why it happens, but we have hypothesized theories regarding some unknown triggers that set off T-cell-mediated reactions in the body, leading to the destruction of your body cells at the hands of macrophages.3Bokhari SRA, Zulfiqar H, Mansur A. Sarcoidosis. [Updated 2023 Jun 25]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430687/
Sarcoidosis of the lungs is mainly a disease in young adults and, more commonly, in females.
Lungs are the most common organ affected by this auto-immune disease (90%).
Sarcoidosis of the lungs presents with general respiratory symptoms4Polverino, F., Balestro, E., & Spagnolo, P. (2020). Clinical Presentations, Pathogenesis, and Therapy of Sarcoidosis: State of the Art. Journal of Clinical Medicine, 9(8), 2363. https://doi.org/10.3390/jcm9082363 such as:
- Dry cough
- Breathing difficulty
- Weight loss
- Non-specific chest pain
- Early fatigue
These symptoms may be experienced in other minor conditions, such as mild forms of pneumonia and common flu. However, sarcoidosis causes cough, fatigue, and shortness of breath to persist for a long time. It may resolve spontaneously without treatment or worsen over time.
Your health practitioner will advise you to take a chest X-ray as part of a routine workup and some baseline investigations.
Bilateral lymphadenopathy (enlarged lung lymph nodes on both sides) is quite a pathognomonic sign of sarcoidosis of the lungs. A small proportion of these patients (3-5%) can also have unilateral lymphadenopathy.
Stages of Sarcoidosis of Lungs- Scadding Criteria
Sarcoidosis of the lungs is classically diagnosed on the basis of chest X-rays. In fact, the first and foremost investigation your doctor will advise you will be an x-ray of your chest.
In a few cases, when the diagnosis is doubted or to gauge the severity of the disease, your doctor may also recommend a High-Resolution Computed Tomography (HRCT) test.
Sarcoidosis of lungs is staged5Maller V, Elfeky M, Knipe H, et al. Thoracic sarcoidosis (staging). Reference article, Radiopaedia.org (Accessed on 26 Sep 2024) https://doi.org/10.53347/rID-4997 based on chest radiograph image (Scadding criteria), which is described as follows:
- Stage 0: Normal
Patients who present during the early stage of the disease may have no changes in their chest X-ray. - Stage 1: Hilar Lymph Node Enlargement Only
This happens when lymphadenopathy is on both sides of your lung fields (near the mediastinum in the center). If detected at this stage, it may as well undergo spontaneous resolution.
Chest Radiograph showing Stage 2 Sarcoidosis of Lungs (Image Source: Wikimedia Commons) - Stage 2: Lymph Node Enlargement and Involvement of Lung Parenchyma (Granulomas)
Bilateral hilar lymphadenopathy with lung infiltrates. There is evidence of both lymph node enlargement and parenchymal involvement, indicating the spread of inflammation to lung tissue. Symptoms, such as cough and shortness of breath, are often more noticeable.

- Stage 3: Presence of Disease (Granulomas) in the Parenchyma of the Lung only.
Parenchymal infiltrates without hilar lymphadenopathy. The lymph nodes are no longer enlarged, but significant lung involvement indicates advanced inflammatory spread within the lungs. Respiratory symptoms, such as dyspnea, are common in this stage. At this stage, there is only a 10-20% chance of spontaneous resolution.

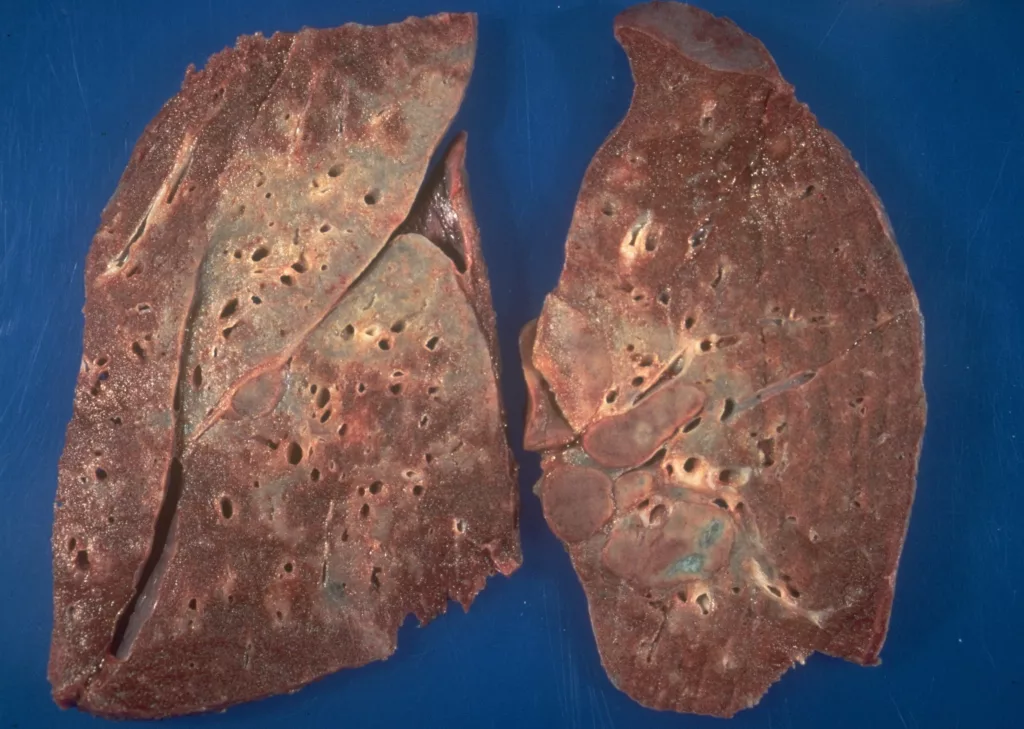
- Stage 4: End-Stage Lung Sarcoidosis (Pulmonary Fibrosis)
Near total or total destruction of lung parenchyma, making a patient oxygen-dependent and a candidate for lung replacement.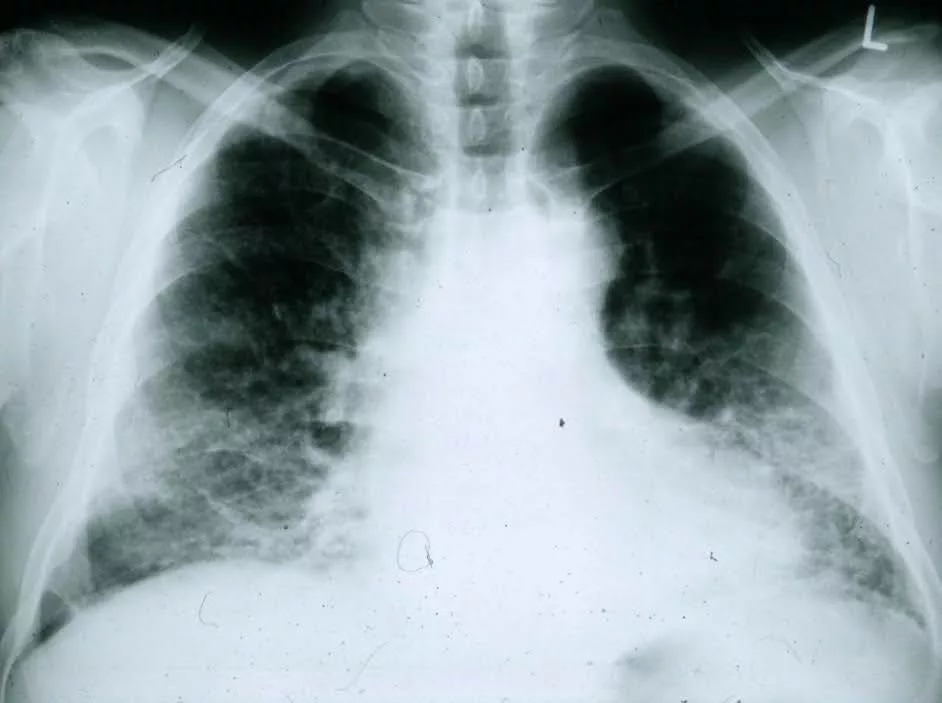
Chest Radiograph showing Stage 4 Sarcoidosis of Lungs (Image Source: Wikimedia Commons)
Sarcoidosis of Lungs Prognosis: How long is the Survival?
The fate of patients having sarcoidosis of the lungs is variable. It should be, however, relieving to know that about two-thirds6Sarcoidosis Prognosis – Foundation for Sarcoidosis Research. (2019, January 18). Foundation for Sarcoidosis Research. https://www.stopsarcoidosis.org/what-is-sarcoidosis/prognosis/ of these patients will be cured, either spontaneously or with the help of a limited period of medications.
Sarcoidosis patients can meet any of the following fates, given their stage at diagnosis, age at diagnosis, and involvement of other organs by the disease:
- The disease will regress spontaneously without any treatment
- The patients will undergo remission after a short course of prescribed treatment
- The patients will remain under treatment and surveillance for a considerable time
- The patients will require lung transplantation and may become morbid and oxygen-dependent for the rest of their days on Earth.
The following are a few factors that alter the prognosis of sarcoidosis of lungs7Kobak S. (2020). Catch the rainbow: Prognostic factor of sarcoidosis. Lung India: official organ of Indian Chest Society, 37(5), 425–432. https://doi.org/10.4103/lungindia.lungindia_380_19
Gender:
Females generally have a poorer prognosis than males. In fact, females with sarcoidosis will have more functional impairment as compared to their male counterparts.
Age:
Sarcoidosis in relatively younger and middle-aged people tends to resolve spontaneously and is more treatment-responsive than that in elderly people (>40 years).
Ethnicity:
Like the other two, ethnicity is also a non-modifiable factor. It has been studied that sarcoidosis has a poorer prognosis in African-Americans than that in Caucasians.
Extra-Pulmonary Involvement:
Involvement of other systems such as the eyes, skin, heart, nervous system, and joints has a not-so-good impact on the prognosis of sarcoidosis of lungs.
Positive Family History:
Few genetic sequences are known to be associated with harsh fates in sarcoidosis patients (e.g., HLA-DQB1*1501 and the Annexin A11 gene).
Timeline:
A short-lived, acute phase of disease is more likely to meet complete resolution than an ever-lasting diseased state.
Stage:
Late-stage sarcoidosis (stages 3 and 4) usually has a poor outcome for the patient’s quality of life and life expectancy.
Laboratory Markers:
The presence of high levels of inflammatory markers (e.g., KL-6, TNF-alpha) is an indication of aggressive forms of the disease.
About 50% of these cases may also have raised angiotensin converting (ACE) enzymes8Belperio, J. A., Fishbein, M. C., Abtin, F., Channick, J., Balasubramanian, S. A., & Lynch, J. P., III. (2023). Pulmonary sarcoidosis: A comprehensive review: Past to present. Journal of Autoimmunity, 103107. https://doi.org/10.1016/j.jaut.2023.103107 in the blood, which is a rather nonspecific finding.
Sarcoidosis of the Lungs Diagnosis
The diagnosis of pulmonary sarcoidosis is a systemic approach, wherein your doctor will begin inspecting you step by step as follows:
History & Examination:
Typical symptoms of chest pain, chronic dry cough, and breathing difficulty will prompt a doctor to investigate your lungs for commonly occurring infectious and non-infectious ailments. Certain conditions such as the Löfgren syndrome9Brown F, Modi P, Tanner LS. Lofgren Syndrome. [Updated 2023 Jul 31]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482315/ (systemic sarcoidosis) straightaway gives the impression of sarcoidosis of lungs.
On physical examination, you may appear short of breath, have an increased respiratory rate and an increased heart rate due to additional breathing effort, and have your chest sound harsh or wheezy on auscultation. There may also be low-grade fever.
Advanced stages of pulmonary sarcoidosis may present with fatigue, air hunger, paleness, and emaciation.
Radiology:
A chest X-ray is the mainstay for diagnosing pulmonary sarcoidosis.10Nunes, H., Uzunhan, Y., Gille, T., Lamberto, C., Valeyre, D., & Brillet, P. (2012). Imaging of sarcoidosis of the airways and lung parenchyma and correlation with lung function. European Respiratory Journal, 40(3), 750–765. https://doi.org/10.1183/09031936.00025212
Usually, a plain PA view of your chest is enough to give your doctor insight into your diagnosis and management.
In a significant number of pulmonary sarcoidosis cases, HRCT11Sharma, R., Guleria, R., Mohan, A., & Das, C. (2004). Scadding criteria for diagnosis of sarcoidosis: Is there a need for change? CHEST Journal, 126(4), 754S. https://doi.org/10.1378/chest.126.4_meetingabstracts.754s is also required, especially when extensive disease is suspected, which may require more aggressive management strategies. Even for early forms of pulmonary sarcoidosis, relying merely on chest radiographs may underestimate the severity of the disease and, hence, can delay treatment. It is important to emphasize the need for cardiac function evaluation (echocardiography) in pulmonary fibrosis, as the disease commonly affects these thoracic viscera.
Pulmonary Function Tests:
Any chronic lung disease requires investigation of pulmonary parameters.12Yao, Q., Ji, Q., & Zhou, Y. (2023). Pulmonary Function in Pulmonary Sarcoidosis. Journal of Clinical Medicine, 12(21), 6701. https://doi.org/10.3390/jcm12216701 Lungs will function normally in milder forms of pulmonary sarcoidosis. However, 10 to 30% of patients may experience some form of pulmonary function restriction.
The carbon monoxide diffusion capacity (DLCO) determines the gas diffusion capacity offered by lung parenchyma. Forced vital capacity (FVC) reflects the amount of air that can be forcibly cleared from the lungs (it differentiates between restrictive and obstructive lung disease). In sarcoidosis of the lungs, a DLCO of <60% and FVC of <70% indicates significant involvement of the lung and warrants treatment.
Biopsy:
Histopathology13Ungprasert, P., Ryu, J. H., & Matteson, E. L. (2019). Clinical Manifestations, Diagnosis, and Treatment of Sarcoidosis. Mayo Clinic proceedings. Innovations, quality & outcomes, 3(3), 358–375. https://doi.org/10.1016/j.mayocpiqo.2019.04.006 is the definitive diagnosis of the disease. Transbronchial biopsy using a flexible bronchoscope is used to obtain a piece of hilar tissue. This is a safe procedure that requires mild sedation only. If adequate hilar lymph node tissue is unavailable or inaccessible, the next best specimen would be the lung parenchyma.
A triad of relatable history, radiographic findings, and histopathology results is required to declare one as having sarcoidosis of the lungs.
Histopathological findings14Belperio, J. A., Fishbein, M. C., Abtin, F., Channick, J., Balasubramanian, S. A., & Lynch, J. P., III. (2023b). Pulmonary sarcoidosis: A comprehensive review: Past to present. Journal of Autoimmunity, 103107. https://doi.org/10.1016/j.jaut.2023.103107 of pulmonary sarcoidosis are discrete, non-necrotizing granulomas composed of multinucleated giant cells and multinucleated giant cells surrounded by plasma cells, lymphocytes and fibroblasts at the periphery.
Sarcoidosis Lungs Life Expectancy
The life span of patients with pulmonary sarcoidosis is variable and depends on the stage of disease and involvement of extrapulmonary sites (such as the heart and nervous system).
A single-centered study15Huitema, M., Mathijssen, H., Bakker, A., Mager, J., Van Houten, L., Grutters, J., & Post, M. (2022). Four-year survival rate in pulmonary sarcoidosis with extensive pulmonary hypertension screening. Respiratory Medicine, 195, 106762. https://doi.org/10.1016/j.rmed.2022.106762 determined that the four-year survival of newly diagnosed patients referred to a tertiary care setup was 96.4%. Those with more severe forms of the disease had a five-year survival rate of 91.5%.
Mainly, the patients who died of sarcoidosis were the ones who had end-stage heart disease, neurosarcoidosis, and those who were significantly older with respect to age.
Generally, the mortality rate16Belperio, J. A., Fishbein, M. C., Abtin, F., Channick, J., Balasubramanian, S. A., & Lynch, J. P., III. (2023c). Pulmonary sarcoidosis: A comprehensive review: Past to present. Journal of Autoimmunity, 103107. https://doi.org/10.1016/j.jaut.2023.103107 for sarcoidosis of lungs over five years is 7%.
Though the rates of spontaneous resolution are high in patients presenting with stage 1 and 2 sarcoidosis, up to 10-40% of these patients end up developing progressive pulmonary disease. Of these, 60% of patients die due to cardiopulmonary complications.
Treatment of Sarcoidosis of Lungs
The decision to treat sarcoidosis of the lungs depends upon the following factors:
- Stage of the disease
- Severity of the disease
- Propensity for spontaneous remission
- Risk of progression
- Risk of impaired quality of disease
There is a large proportion of sarcoidosis patients out in the world who don’t require any medical attention, as they are asymptomatic and have non-progressive forms of pulmonary sarcoidosis.17Thillai, M., Atkins, C. P., Crawshaw, A., Hart, S. P., Ho, L.-P., Kouranos, V., Patterson, K. C., Screaton, N. J., Whight, J., & Wells, A. U. (2021). *BTS Clinical Statement on Pulmonary Sarcoidosis*. Thorax. https://doi.org/10.1136/thoraxjnl-2019-214348
On the other hand, a significant number of patients progress to severe forms of sarcoidosis of the lungs and require life-long treatment.
Steroids:
Since the disease is auto-immune in nature, you would naturally think of something that can overcome the triggered immune system. Oral glucocorticoids are the mainstay of pulmonary sarcoidosis. Studies18Paramothayan, N. S., Lasserson, T. J., & Jones, P. (2005). Corticosteroids for pulmonary sarcoidosis. Cochrane Library, 2010(5). https://doi.org/10.1002/14651858.cd001114.pub2 have shown an improvement in radiographic findings of patients taking prednisone for pulmonary sarcoidosis compared to placebo.
The timeline for administration of steroid therapy varies with each patient. Your doctor will start you on high-dose steroids initially and will taper it over months, depending upon the disease response to treatment.
There are, however, associated side effects (osteoporosis, diabetes, weight gain, hypertension, impaired immunity) of using prednisolone >10 mg/day19Melani, A. S., Bigliazzi, C., Cimmino, F. A., Bergantini, L., & Bargagli, E. (2021). A Comprehensive Review of Sarcoidosis Treatment for Pulmonologists. Pulmonary Therapy, 7(2), 325–344. https://doi.org/10.1007/s41030-021-00160-x, which may resolve gradually as the steroid therapy is gradually discontinued.
Immunosuppressants:
In case you have severe forms of sarcoidosis of the lungs or are at risk of developing impaired quality of life, immunosuppressive therapy will be added as an adjunct to oral steroids.
Methotrexate has been shown to be 80% clinically effective and tolerable in a small cohort20Fang, C., Zhang, Q., Wang, N., Jing, X., & Xu, Z. (2019). Effectiveness and tolerability of methotrexate in pulmonary sarcoidosis: A single center real-world study. Sarcoidosis Vasculitis and Diffuse Lung Diseases, 36(3), 217–227. https://doi.org/10.36141/svdld.v36i3.8449 of 49 patients in the setting of pulmonary sarcoidosis. A randomized controlled trial also shows comparatively less glucocorticoid requirement when used in conjunction with methotrexate.
Anti-inflammatory Therapy:
As discussed above, tumor-necrosis factor is significantly raised in patients with sarcoidosis of the lungs. Likewise, anti-TNF-ALPHA therapy in the form of infliximab and adalimumab is initiated in selected sarcoidosis patients.21Rezaee, M., Zangiabadian, M., Soheili, A., Calcagno, T. M., Rahmannia, M., Dinparastisaleh, R., Nasiri, M. J., & Mirsaeidi, M. (2023). Role of anti-tumor necrosis factor-alpha agents in the treatment of sarcoidosis: A meta-analysis. European Journal of Internal Medicine, 109, 42-49. https://doi.org/10.1016/j.ejim.2022.12.017 The treatment is slightly more effective in overcoming extrapulmonary sarcoidosis symptoms (75% Vs. 70%).
However, this treatment modality is for selected patients only (aggressive and advanced disease forms).
Lung Transplantation:
Advanced pulmonary sarcoidosis, characterized by severe lung fibrosis and pulmonary hypertension that resists treatment, can significantly impair quality of life due to oxygen dependence and limited mobility. In such cases, a lung transplant may become necessary.
Before proceeding with a transplant, it’s essential to identify and address any additional factors, such as myocardial disease or malignancy, that could impact the success of the new lung transplant.22Meyer K. C. (2019). Lung transplantation for pulmonary sarcoidosis. Sarcoidosis, vasculitis, and diffuse lung diseases: official journal of WASOG, 36(2), 92–107. https://doi.org/10.36141/svdld.v36i2.7163
Conclusion:
Sarcoidosis is a multi-systemic inflammatory condition in which your immune system initiates an attack against your own body viscera, particularly the lungs, lymph nodes, heart, nervous system, ocular system, and musculoskeletal system.
Refrences
- 1American Lung Association. Learn about sarcoidosis. https://www.lung.org/lung-health-diseases/lung-disease-lookup/sarcoidosis/learn-about-sarcoidosis/
- 2Arkema, E. V., & Cozier, Y. C. (2020). Sarcoidosis epidemiology: recent estimates of incidence, prevalence and risk factors. Current opinion in pulmonary medicine, 26(5), 527–534. https://doi.org/10.1097/MCP.0000000000000715
- 3Bokhari SRA, Zulfiqar H, Mansur A. Sarcoidosis. [Updated 2023 Jun 25]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430687/
- 4Polverino, F., Balestro, E., & Spagnolo, P. (2020). Clinical Presentations, Pathogenesis, and Therapy of Sarcoidosis: State of the Art. Journal of Clinical Medicine, 9(8), 2363. https://doi.org/10.3390/jcm9082363
- 5Maller V, Elfeky M, Knipe H, et al. Thoracic sarcoidosis (staging). Reference article, Radiopaedia.org (Accessed on 26 Sep 2024) https://doi.org/10.53347/rID-4997
- 6Sarcoidosis Prognosis – Foundation for Sarcoidosis Research. (2019, January 18). Foundation for Sarcoidosis Research. https://www.stopsarcoidosis.org/what-is-sarcoidosis/prognosis/
- 7Kobak S. (2020). Catch the rainbow: Prognostic factor of sarcoidosis. Lung India: official organ of Indian Chest Society, 37(5), 425–432. https://doi.org/10.4103/lungindia.lungindia_380_19
- 8Belperio, J. A., Fishbein, M. C., Abtin, F., Channick, J., Balasubramanian, S. A., & Lynch, J. P., III. (2023). Pulmonary sarcoidosis: A comprehensive review: Past to present. Journal of Autoimmunity, 103107. https://doi.org/10.1016/j.jaut.2023.103107
- 9Brown F, Modi P, Tanner LS. Lofgren Syndrome. [Updated 2023 Jul 31]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482315/
- 10Nunes, H., Uzunhan, Y., Gille, T., Lamberto, C., Valeyre, D., & Brillet, P. (2012). Imaging of sarcoidosis of the airways and lung parenchyma and correlation with lung function. European Respiratory Journal, 40(3), 750–765. https://doi.org/10.1183/09031936.00025212
- 11Sharma, R., Guleria, R., Mohan, A., & Das, C. (2004). Scadding criteria for diagnosis of sarcoidosis: Is there a need for change? CHEST Journal, 126(4), 754S. https://doi.org/10.1378/chest.126.4_meetingabstracts.754s
- 12Yao, Q., Ji, Q., & Zhou, Y. (2023). Pulmonary Function in Pulmonary Sarcoidosis. Journal of Clinical Medicine, 12(21), 6701. https://doi.org/10.3390/jcm12216701
- 13Ungprasert, P., Ryu, J. H., & Matteson, E. L. (2019). Clinical Manifestations, Diagnosis, and Treatment of Sarcoidosis. Mayo Clinic proceedings. Innovations, quality & outcomes, 3(3), 358–375. https://doi.org/10.1016/j.mayocpiqo.2019.04.006
- 14Belperio, J. A., Fishbein, M. C., Abtin, F., Channick, J., Balasubramanian, S. A., & Lynch, J. P., III. (2023b). Pulmonary sarcoidosis: A comprehensive review: Past to present. Journal of Autoimmunity, 103107. https://doi.org/10.1016/j.jaut.2023.103107
- 15Huitema, M., Mathijssen, H., Bakker, A., Mager, J., Van Houten, L., Grutters, J., & Post, M. (2022). Four-year survival rate in pulmonary sarcoidosis with extensive pulmonary hypertension screening. Respiratory Medicine, 195, 106762. https://doi.org/10.1016/j.rmed.2022.106762
- 16Belperio, J. A., Fishbein, M. C., Abtin, F., Channick, J., Balasubramanian, S. A., & Lynch, J. P., III. (2023c). Pulmonary sarcoidosis: A comprehensive review: Past to present. Journal of Autoimmunity, 103107. https://doi.org/10.1016/j.jaut.2023.103107
- 17Thillai, M., Atkins, C. P., Crawshaw, A., Hart, S. P., Ho, L.-P., Kouranos, V., Patterson, K. C., Screaton, N. J., Whight, J., & Wells, A. U. (2021). *BTS Clinical Statement on Pulmonary Sarcoidosis*. Thorax. https://doi.org/10.1136/thoraxjnl-2019-214348
- 18Paramothayan, N. S., Lasserson, T. J., & Jones, P. (2005). Corticosteroids for pulmonary sarcoidosis. Cochrane Library, 2010(5). https://doi.org/10.1002/14651858.cd001114.pub2
- 19Melani, A. S., Bigliazzi, C., Cimmino, F. A., Bergantini, L., & Bargagli, E. (2021). A Comprehensive Review of Sarcoidosis Treatment for Pulmonologists. Pulmonary Therapy, 7(2), 325–344. https://doi.org/10.1007/s41030-021-00160-x
- 20Fang, C., Zhang, Q., Wang, N., Jing, X., & Xu, Z. (2019). Effectiveness and tolerability of methotrexate in pulmonary sarcoidosis: A single center real-world study. Sarcoidosis Vasculitis and Diffuse Lung Diseases, 36(3), 217–227. https://doi.org/10.36141/svdld.v36i3.8449
- 21Rezaee, M., Zangiabadian, M., Soheili, A., Calcagno, T. M., Rahmannia, M., Dinparastisaleh, R., Nasiri, M. J., & Mirsaeidi, M. (2023). Role of anti-tumor necrosis factor-alpha agents in the treatment of sarcoidosis: A meta-analysis. European Journal of Internal Medicine, 109, 42-49. https://doi.org/10.1016/j.ejim.2022.12.017
- 22Meyer K. C. (2019). Lung transplantation for pulmonary sarcoidosis. Sarcoidosis, vasculitis, and diffuse lung diseases: official journal of WASOG, 36(2), 92–107. https://doi.org/10.36141/svdld.v36i2.7163