What is Scleroderma?
Scleroderma is a group of complex autoimmune disorders characterized by hardening and tightening of the skin and connective tissue. The condition may affect various organs and negatively impact the individual’s quality of life. Understanding the symptoms, complications, cause, stage, and type of scleroderma is important for the patient, healthcare professional, and caregiver.
Scleroderma is much more common in women than in men.1Bairkdar, Majd, et al. “Incidence and prevalence of systemic sclerosis globally: a comprehensive systematic review and meta-analysis.” Rheumatology 60.7 (2021): 3121-3133. It is typically found in people between 30 and 50. Many people are diagnosed with this disease every year, and the death rate because of the most serious form of this disease is also very high.
Types of Sclerodermas
There are two main types of sclerodermas: localized and systemic. These types have further subtypes, each consisting of several conditions.
Localized Scleroderma
Typically, the skin is the only organ affected in this type. However, tissue injury may extend into the underlying tissues like fascia, subcutaneous tissue, muscle, and bone, damaging them too. The prognosis of localized scleroderma is good. The skin lesions caused by localized scleroderma can improve with time and even be completely cured. There are further subtypes of localized scleroderma.
Circumscribed Morphea
Morphea causes patches of hard, thickened skin. These discolored patches may be a single patch or multiple patches. Depending on the severity, the patches may vary in size and shape. They typically have a red border and a thickened yellow center.
Generalized Morphea
This type has many morphea patches in the trunk, arms, legs, and neck, which merge.
Linear Scleroderma
In linear scleroderma, tight, thick bands are seen in the body, mostly in the trunk, extremities, buttocks, or face. It often appears as one single band, but sometimes it is present in combination with the morphea. Linear scleroderma is more common in younger age groups in children ten and under.2Bairkdar, Majd, et al. “Incidence and prevalence of systemic sclerosis globally: a comprehensive systematic review and meta-analysis.” Rheumatology 60.7 (2021): 3121-3133.
Systemic Scleroderma
This is a severe form of scleroderma, also called systemic sclerosis. It affects the skin and other structures, such as blood vessels, the heart, kidneys, the gastrointestinal tract, muscles, and joints. Facial involvement is common, and the quality of a patient’s life is affected. Here are the types of systemic scleroderma or systemic sclerosis:
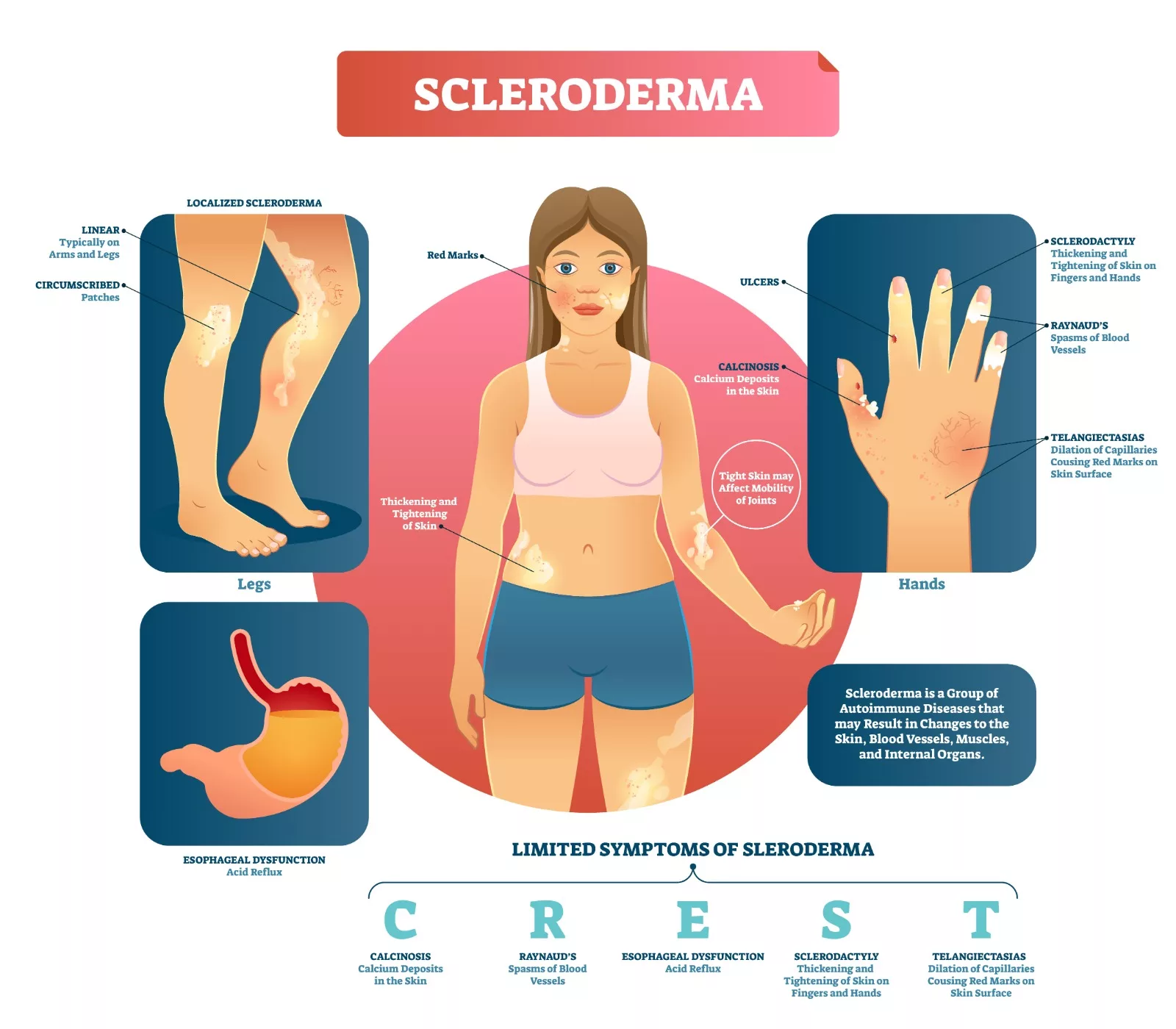
Limited Cutaneous Scleroderma
This is the most common type. The skin hardening and tightening is usually limited to the fingers and hands; rarely, the forearm and face are also involved. Patients typically present with puffy fingers beyond the knuckles (metacarpophalangeal or MCP joints). Over time, they develop skin hardening extending beyond the elbows and knees and, to a lesser extent, the face and neck. The trunk, upper arms, and legs are usually spared. Internal organ damage is usually less. In general, patients have a normal life expectancy, but some may show GI tract issues like heartburn, and in severe cases, there can be musculoskeletal pain and Raynaud’s phenomenon. CREST syndrome is a subtype of limited scleroderma.
CREST is an acronym that highlights the most common symptoms.
C – Calcinosis: Calcium deposits under the skin and tissues
R – Raynaud’s Phenomenon: Tips of the fingers and toes change color and become numb and tingling due to changes in temperature
E – Esophageal dysmotility: Food or liquids do not easily pass down the esophagus in this disease. This causes problems with swallowing, thus leading to heartburn.
S – Sclerodactyly: The skin of the fingers becomes thick.
T – Telangiectasias: small, widened blood vessels on the skin that appear red.
Diffuse Cutaneous Scleroderma
Diffuse scleroderma, a subtype of Systemic sclerosis, involves excess collagen production, which causes skin thickening over large body areas. These thickenings usually affect the hands, fingers, arms, legs, face, and anterior trunk. Moreover, this condition can lead to significant organ damage, including kidneys, gastrointestinal tract, heart, and lungs. Additionally, tightening of the skin comes with itching and dryness. Musculoskeletal pain is also a common symptom.
Life-threatening complications arise when the lungs and heart are involved. Kidney damage can occur due to acute severe systemic high blood pressure. Understanding these impacts emphasizes the need for early and comprehensive management of diffuse scleroderma.
Sine Scleroderma
Sine scleroderma is a distinct form of systemic scleroderma that presents features of systemic organ disease, including Raynaud’s phenomenon, but notably lacks the characteristic skin symptoms. Consequently, patients with sine scleroderma can experience a range of symptoms and complications typical of either limited or diffuse scleroderma, such as cardiac, renal, gastrointestinal, and pulmonary involvement, but they do not develop skin thickening. Diagnosing sine scleroderma is crucial for healthcare professionals to understand the disease’s systemic nature, ensuring appropriate diagnosis and management.
Systemic Scleroderma with Overlap Syndrome
Patients with systemic scleroderma (SSc) of any of the above subtypes can also show symptoms of other systemic rheumatic diseases, such as systemic lupus erythematosus (SLE), rheumatoid arthritis, polymyositis, or Sjögren’s disease.
Symptoms of Scleroderma
Scleroderma is a multifaceted autoimmune disorder that manifests in various symptoms, ranging from mild to severe, significantly impacting an individual’s quality of life. Understanding these symptoms is essential for early diagnosis and management. The symptoms of scleroderma may appear differently in each individual. For some, it may only affect the skin, but it can extend deeper in others, impacting the joints, digestive tract, and internal organs. These symptoms can range from being merely bothersome to extremely painful, and in severe cases, they may even be life-threatening.
Skin Changes
- Thickening and Swelling: The most easily recognizable manifestation is skin thickening and swelling. However, it may not be present in all patients.
- Atrophic, Dry, and Scaly Skin: In later stages, the involved skin becomes atrophic, dry, and scaly due to the loss of natural oils (sebaceous gland damage).3Adnan, Zainal Arifin. “Diagnosis and treatment of scleroderma.” Acta Med Indones 40.2 (2008): 109-12
- Taut, Shiny, Darker Skin: Large areas of skin may appear taut, shiny, and darker, causing problems with movement.
- Calcium Bumps: Calcium deposits (calcinosis) can form on fingers or other bony areas such as elbows and knees.
- Sores on Fingertips and Knuckles: Ulcers or sores may develop on the fingertips and knuckles.
Raynaud’s Phenomenon
- Pale and Dusky Fingertips: Fingers may become pale and dusky, often turning numb and tingling when exposed to cold or stress.4Kahaleh, M. Bashar. “Raynaud phenomenon and the vascular disease in scleroderma.” Current opinion in rheumatology 16.6 (2004): 718-722 This is usually an early sign of scleroderma.
Joint and Muscle Symptoms
- Joint Pain and Stiffness (Arthralgia): Joint pain and stiffness are common, especially in areas around the tendons. Joint mobility is often limited and painful.
- Limited Mobility: Muscle weakness is another feature that leads to limited mobility or immobility of fingers, wrists, or elbows. This occurs due to skin thickening or muscle atrophy and fibrosis.
Gastrointestinal Symptoms
- Heartburn: A common symptom where patients complain of a sensation that food is lodged in the chest behind the sternum.
- Dysphagia (Trouble Swallowing): Difficulty in swallowing due to esophageal involvement.
- Grating Noise: Movement may produce a grating noise from inflamed joints and tissues.
Pulmonary Symptoms
- Shortness of Breath: Due to pulmonary involvement, patients may experience difficulty breathing.
- Pulmonary Hypertension: Increased blood pressure in the lungs’ arteries, leading to further respiratory issues.
Cardiac Symptoms
- Abnormal Heart Rhythms: Irregular heartbeats can occur.
- Heart Failure: Severe cases may lead to heart failure due to the disease’s impact on the heart muscle.
Renal Symptoms
- High Blood Pressure: This can lead to kidney failure if not managed properly.
- Scleroderma Renal Crisis (SRC): Occurs in 10% of patients and is characterized by sudden onset of malignant hypertension. This includes very high blood pressure, headaches, visual disturbances, and heart failure.
General Pain & Discomfort
- Pain: Pain in scleroderma may range from a feeling of discomfort to unbearable pain, affecting the patient’s daily life.
Understanding these varied symptoms helps recognize the extent and severity of scleroderma, ensuring timely and effective management to improve the quality of life for those affected by this complex disease.
Risk factors
Unfortunately, the exact cause of scleroderma is still unknown, but according to research, like many other autoimmune diseases, scleroderma stems from problems with our immune systems. However, some factors are considered a potential risk for developing this condition. These include:
Gender
Women are more likely to get scleroderma. 80% of the diagnosed patients with scleroderma are women.5Adnan, Zainal Arifin. “Diagnosis and treatment of scleroderma.” Acta Med Indones 40.2 (2008): 109-12
Age
Approximately half of the cases of localized scleroderma are diagnosed before the age of 40, while cases of systemic scleroderma are usually diagnosed between the ages of 30 and 50.
Ethnicity
Several US studies have suggested that black patients have a higher age-specific incidence rate and more severe disease than white patients.6Mayes, Maureen D. “Scleroderma epidemiology.” Rheumatic Disease Clinics of North America 22.4 (1996): 751-764
Familial Scleroderma
Reports indicate that some families have multiple cases of scleroderma. Additionally, some cases involve individuals who have family members with either scleroderma or scleroderma spectrum diseases.
Environmental Factors
Some environmental factors, such as exposure to silica, contribute to the risk of developing scleroderma. Certain drugs and solvents can also increase the risk.
Immunogenetic Links
Genetics plays a role in scleroderma, but it is not transferred from parents to children. Multiple studies have tried to establish a link between HLA types and scleroderma.
Diagnosis
Scleroderma symptoms are similar to those of several other conditions. It can take longer to determine whether scleroderma is the cause or which of the different types of scleroderma is present.
Some common scleroderma symptoms, like Raynaud’s phenomenon and sudden puffy and swollen skin, can make it easy to diagnose. The common course of action when a patient presents with scleroderma is.
Medical History
Healthcare professionals begin by taking a detailed medical history, observing the symptoms, and considering the onset and duration of the disease. They will also ask about family history and other environmental factors that may have contributed.
Physical Examination
A thorough physical examination can clarify the picture. Doctors assess hands, fingers, legs, and other body parts for skin thickening, tightening, and discoloration.
Nailfold Capillaroscopy
It is a simple, safe, and noninvasive imaging technique specific for scleroderma that looks at the skin near the base of the fingernail with a magnifier to determine if there is capillary (small blood vessels in the skin) loss or distortion, such as dilatation.7Etehad Tavakol, Mahnaz, et al. “Nailfold capillaroscopy in rheumatic diseases: which parameters should be evaluated?.” BioMed research international 2015.1 (2015): 974530
Blood Tests
Antinuclear Antibodies (ANA)
This test checks for the presence of antinuclear antibodies, which are often elevated in autoimmune diseases like scleroderma. The results of an ANA test alone don’t determine a diagnosis of scleroderma, which is a clinical diagnosis that takes into account all factors.
Anti-Scl-70 (Anti-Topoisomerase I) Antibodies
The presence of Anti-Scl-70 antibodies is associated with diffuse cutaneous systemic sclerosis and indicates a higher risk of pulmonary fibrosis.
Anti-Centromere Antibodies
The purpose of this test is to detect antibodies against centromeres. These antibodies are commonly found in patients with limited cutaneous systemic sclerosis (CREST syndrome). It indicates a slower disease progression and later onset of internal organ involvement.
Imaging Tests
Chest X-ray
This helps identify any lung involvement, such as interstitial lung disease or pulmonary fibrosis, which are common complications of systemic scleroderma.
High-Resolution CT Scan
It is more detailed than X-ray and provides a clearer picture.
Electrocardiogram (EKG or ECG) & Echocardiogram
These tests evaluate heart function and check for potential complications caused by scleroderma. An echocardiogram examines the structure and function of the heart.
Pulmonary Function Tests
These tests check lung capacity and function and check for potential pulmonary hypertension and complications due to scleroderma.
Gastrointestinal Tests
Gastrogram
An X-ray is done after a barium swallow. This shows the structure and function of the esophagus.
Endoscopy
This procedure helps the doctor examine the esophagus, stomach, and upper small intestine for scarring, inflammation, and abnormalities.
Skin Biopsy
Physicians may excise a small sample of skin and observe it under the microscope to see the changes caused by scleroderma-like fibrosis and increased collagen deposition.
Urinalysis
Kidney function and any abnormalities can be detected through this test. It can identify scleroderma-related kidney diseases.
Specialist Referral
According to the primary findings, the general physician can refer the patient to specialists like:
- Rheumatologist
- Pulmonologist
- Cardiologist
- Gastroenterologist
Accurate diagnosis of scleroderma requires a combination of thorough medical history, physical examination, and a range of diagnostic tests. Early and precise diagnosis is crucial for effective management and improving the quality of life for individuals with scleroderma.
Management & Treatment
Scleroderma is a chronic disease affecting a patient’s physical and mental well-being. Currently, there is no treatment specifically for scleroderma, but doctors make a combination that works best to decrease the severity and symptoms of the disease.
Treatment may include the following:
Medication
- Pain relief either through Nonsteroidal anti-inflammatory drugs (NSAIDs) or through corticosteroids.
- Immunosuppressants like methotrexate may be given to manage skin and joint issues.
- Administering lotions and moisturizers to ease skin itching.
- Vasodilators like calcium channel blockers are used to manage Raynaud’s phenomenon by dilating blood vessels.
- Angiotensin-converting enzyme (ACE) inhibitors effectively manage renal crises and reduce blood pressure.
- Gastroesophageal reflux disease (GERD) and esophageal symptoms can be relieved by proton pump inhibitors like omeprazole.
- Nintedanib is an antifibrotic agent that was recently approved for treating interstitial lung disease in systemic sclerosis.
Physical & Occupational Therapy
- Range of motion exercises maintain joint mobility.
- Strengthening and stretching exercises to reduce skin tightness and increase flexibility.
- Splinting can correct deformities, particularly in hands and feet.
- Adaptive devices can be used for daily work and to improve hand function.
Pulmonary Rehabilitation
Breathing and aerobic exercises can enhance lung capacity and improve cardiovascular health and overall endurance.
Skin & Wound Care
Regular skin monitoring can ensure early detection and management of wounds and ulcers. If a wound exists, dressing it can prevent infections and speed up healing.
Gastrointestinal Management
Managing digestive tract function to optimize nutritional intake is important. Smaller, frequent meals: Reduces symptoms of bloating and discomfort. Laxatives and stool softeners can address constipation and improve bowel function.
Counseling & Therapy
Individual therapy addresses emotional and psychological challenges associated with chronic illness. Patients can also join support groups that provide peer support and shared experiences, reducing feelings of isolation.
Cosmetic and Functional Improvement
Scleroderma-related reconstructive surgery addresses significant deformities or functional impairments, improving quality of life.
Routine check-ups
Monitor disease progression, assess treatment efficacy, and adjust management plans as necessary.
Difference between Scleroderma & Systemic Sclerosis
Scleroderma and systemic sclerosis share the common feature of skin involvement, but there are a few differences. Understanding these differences is crucial for diagnosis, treatment, and management of the conditions.
| Scleroderma | Systemic Sclerosis | |
| Definition | Autoimmune disease causes hardening and tightening of the skin. | A subtype of scleroderma that affects skin, blood vessels, and internal organs. |
| Scope | Primarily involves the skin and sometimes the underlying tissues. | Involves skin, blood vessels, and internal organs |
| Severity | Generally less severe, it can be disabling if skin involvement is extensive. | It can be life-threatening due to organ involvement and complications. |
| Progression | Often slow | Can be rapid |
| Treatment | Focuses on managing skin symptoms | Involves immunosuppressants, vasodilators, and treatments targeting specific organs. |
Differential Diagnosis for Scleroderma
Differential diagnosis is a process in which we distinguish a particular disease from other conditions with similar clinical features. Scleroderma has many symptoms that overlap with other diseases, making diagnosing it challenging for health professionals. Some common conditions similar to scleroderma are
- Systemic Lupus Erythematosus (SLE)
- Mixed Connective Tissue Disease (MCTD)
- Rheumatoid Arthritis (RA)
- Eosinophilic Fasciitis
- Nephrogenic Systemic Fibrosis (NSF)
- Sjögren’s Syndrome
Below is a table highlighting the similarities and differences between scleroderma, systemic lupus erythematosus (SLE), and rheumatoid arthritis (RA)
| Aspect | Scleroderma | Systemic Lupus Erythematosus (SLE) | Rheumatoid Arthritis (RA)
|
| Definition | It is an autoimmune disease causing hardening and tightening of skin and connective tissue. | An autoimmune disease that causes inflammation of multiple organs in the body. | An autoimmune disorder primarily affects the joints, leading to swelling and deformation. |
| Primary Symptoms | Skin thickening, Raynaud’s phenomenon, joint pain, organ involvement (lungs, kidneys, heart). | Malar rash, joint pain, photosensitivity, and fatigue. | Joint pain and stiffness, especially in the hands and feet |
| Skin involvement | Significant skin thickening and hardening; taut, shiny skin. | A butterfly-shaped rash on the face (malar rash), discoid rash. | Rarely affects the skin directly, except for subcutaneous nodules. |
| Joint involvement | Joint pain and stiffness, less inflammation compared to RA. | Symmetrical joint pain and inflammation, often with swelling. | Symmetrical joint inflammation with swelling and deformity. |
| Raynaud’s Phenomenon | Common and often an early symptom. | It can occur but is less common than in scleroderma. | It can occur but is less common than in scleroderma. |
| Treatment | Immunosuppressants and symptom-specific treatments. | Immunosuppressants, corticosteroids, antimalarials, NSAIDs. 8Basta, Fabio, et al. “Systemic lupus erythematosus (SLE) therapy: the old and the new.” Rheumatology and Therapy 7.3 (2020): 433-446 | Disease-modifying anti-rheumatic drugs (DMARDs), biologics, NSAIDs, and corticosteroids. |

Conclusion
Scleroderma is a complex autoimmune disorder that can have a very profound effect on an individual’s life. Understanding the symptoms is crucial for early diagnosis of the disease. Ongoing research into the underlying mechanisms of scleroderma is essential for developing more effective treatments and ultimately finding a cure.
Refrences
- 1Bairkdar, Majd, et al. “Incidence and prevalence of systemic sclerosis globally: a comprehensive systematic review and meta-analysis.” Rheumatology 60.7 (2021): 3121-3133.
- 2Bairkdar, Majd, et al. “Incidence and prevalence of systemic sclerosis globally: a comprehensive systematic review and meta-analysis.” Rheumatology 60.7 (2021): 3121-3133.
- 3Adnan, Zainal Arifin. “Diagnosis and treatment of scleroderma.” Acta Med Indones 40.2 (2008): 109-12
- 4Kahaleh, M. Bashar. “Raynaud phenomenon and the vascular disease in scleroderma.” Current opinion in rheumatology 16.6 (2004): 718-722
- 5Adnan, Zainal Arifin. “Diagnosis and treatment of scleroderma.” Acta Med Indones 40.2 (2008): 109-12
- 6Mayes, Maureen D. “Scleroderma epidemiology.” Rheumatic Disease Clinics of North America 22.4 (1996): 751-764
- 7Etehad Tavakol, Mahnaz, et al. “Nailfold capillaroscopy in rheumatic diseases: which parameters should be evaluated?.” BioMed research international 2015.1 (2015): 974530
- 8Basta, Fabio, et al. “Systemic lupus erythematosus (SLE) therapy: the old and the new.” Rheumatology and Therapy 7.3 (2020): 433-446

