TMJ Arthroscopy is a multipurpose procedure to diagnose and treat different types of temporomandibular joint (TMJ) disorders. It is particularly valuable when the clinical diagnosis remains unclear or when non-surgical treatments fail to relieve symptoms. Bilateral TMJ arthroscopy is the first line of treatment for moderate-to-severe TMJ disorders, which leads to a reduction in open TMJ surgeries.1Ângelo, D. F., Sanz, D., & Cardoso, H. J. (2023). Bilateral arthroscopy of the temporomandibular joint: clinical outcomes and the role of a second intervention—a prospective study. Clinical oral investigations, 27(10), 6167-6176. It is a safe, minimally invasive procedure with good effectiveness. Generally, patients have a good acceptance of arthroscopy.
TMJ Arthroscopy Vs Arthrocentesis:
Many people often confuse TMJ arthroscopy with arthrocentesis, as both are minimally invasive procedures performed on the temporomandibular joint. However, they are distinctly different. Arthroscopy involves inserting a small camera (arthroscope) into the joint space, allowing direct visualization, diagnosis, and treatment of internal joint structures. In contrast, arthrocentesis is a simpler procedure that involves lavaging (washing out) the joint using two needles, without the use of an arthroscope. Arthroscopy offers a broader range of therapeutic interventions, while arthrocentesis is typically used for less complex joint disorders.2Al-Moraissi EA. Arthroscopy versus arthrocentesis in the management of internal derangement of the temporomandibular joint: a systematic review and meta-analysis. Int J Oral Maxillofac Surg. 2015 Jan;44(1):104-12. doi: 10.1016/j.ijom.2014.07.008. Epub 2014 Aug 7. PMID: 25123511.
Anatomy Of The Temporomandibular Joint
Understanding the structural components of the TMJ is essential for recognizing the types of pathologies that arthroscopy can address. The temporomandibular joint comprises different hard and soft tissues. Soft tissues attach the lower jaw (mandible) to the cranium (skull) in a flexible way to allow movement. The main anatomical structures and landmarks of the joint include:
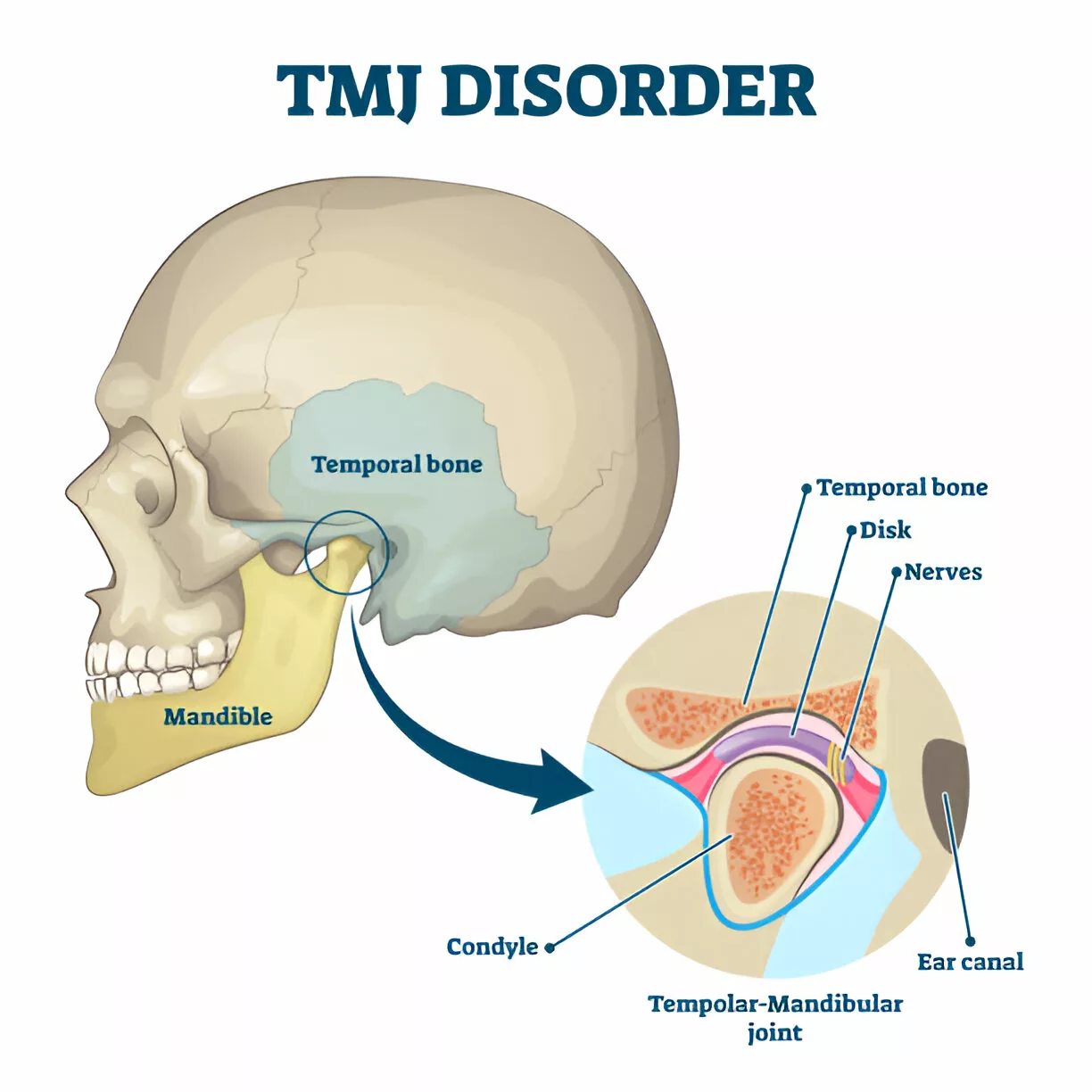
- Glenoid fossa: A socket in the temporal bone of the skull to which the mandible articulates.
- Articular disc: A soft tissue disc that is present between the glenoid fossa and the condyle of the mandible. Made up of fibrocartilage, this disc divides the joint into two synovial cavities. It allows smooth gliding of the mandible and acts as a shock absorber.
- Synovial fluid: The lining of the joint is made up of synovial membrane, which contains the synovial fluid. This fluid lubricates the joint and reduces friction between the moving parts.
- Condyle: Rounded head of the mandible that articulates with the temporal glenoid fossa.
- Ligaments: Multiple ligaments, including sphenomandibular, temporomandibular, and stylomandibular ligaments, are soft tissue structures that provide stability and support to the joint.
- Capsule: A fibrous structure called the capsule encapsulates the joint.
Indications For TMJ Arthroscopy
Your doctor will advise a TMJ arthroscopy in the following conditions:
- Pain, jaw clicking, and dysfunction from TMJ disorder are unresponsive to conventional and non-surgical strategies.
- In cases of degenerative conditions like TMJ osteoarthritis.3Mélou, C., Pellen-Mussi, P., Jeanne, S., Novella, A., Tricot-Doleux, S., & Chauvel-Lebret, D. (2022). Osteoarthritis of the temporomandibular joint: a narrative overview. Medicina, 59(1), 8.
- Diagnosis and management of internal derangements, such as disc displacement with or without reduction.
- Management of patients with atypical facial pain in the periauricular region when other causes have been ruled out.
- Diagnosis of the cause of frequent jaw dislocations.
- Identification of post-traumatic complications of the TMJ.
- Diagnostic confirmation of a pathology before extensive surgery.
- Identification of pseudotumors.
- Biopsy of suspected lesions in the TMJ.
Conditions Treated with TMJ Arthroscopy
Common disorders that respond well to arthroscopic management include internal disc displacement, joint degeneration, muscle spasms, and structural displacements of the jaw.
Internal Derangement
This disorder is characterized by abnormal intra-articular disc position in relation to the mandible’s condyle. The misalignment of the disc leads to functional difficulties and pain. Clinical studies show that operative arthroscopy can be beneficial in managing advanced stages of internal derangement of the TMJ.4Muñoz-Guerra, M. F., Rodríguez-Campo, F. J., Escorial-Hernández, V., Sanz-García, A., Brabyn, P. J., & Fernández-Domínguez, M. (2022). Temporomandibular joint arthroscopy in advanced stages of internal derangement: a retrospective cohort study on the influence of age. International Journal of Oral and Maxillofacial Surgery, 51(12), 1579-1586.
Oral and maxillofacial surgeons frequently use the Wilkes classification to define the extent of the problem (internal derangement) of the joint:
- Stage Ⅰ: The joint is normal with slight disc displacement but no symptoms (clicking and pain).
- Stage Ⅱ: Disc displacement is present with reduction (the disc returns to its normal place). Symptoms at this stage include occasional locking of the jaw and pain.
- Stage Ⅲ: There is a transition from reducing to non-reducing disc displacement in this stage, and patients frequently experience a locked jaw, limited movement, along with joint pain.
- Stage Ⅳ: Early degenerative changes of the joint appear at this stage, and disc displacement may be reducing or non-reducing. Bone damage and the impact of degeneration by osteoarthritis can be seen in this late stage.
- Stage Ⅴ: Non-reducing disc displacement is present with severe degeneration of the joint armamentarium. Patients experience restricted jaw motion and pain.
Osteoarthritis
OA is a highly prevalent joint disease that causes degeneration of the hard structures. The use of arthroscopy has been shown to improve symptoms of osteoarthritis. With an arthroscope in place, doctors can aptly identify issues like loose bodies and scar tissues (adhesions). The surgeon can then remove these adhesions, which potentially leads to improvement in joint mobility. Professionals can pair arthroscopy with procedures like arthrocentesis (flushing of the joint) to remove inflammatory cells and enhance joint function.
Spasm Of The Jaw
Hemimasticatory spasm (HMS) is a muscle disorder that causes forceful contractions of the jaw muscles, leading to clenching. Patients experience involuntary jaw closure (forceful), jaw pain, and muscle twitching. Chewing and speaking difficulties lead to a poor quality of life. Doctors suspect a nerve issue to be the likely cause of this disorder. A 2023 study revealed that arthroscopy-assisted masseter nerve avulsion effectively improved symptoms and preserved masticatory effectiveness in HMS patients.5Pillai, A. R., Kumar, G. J., Kumar, P., Nizar, S. A., Pendyala, S. K., & Baig, F. A. H. (2023). Assessment of the efficacy of TMJ arthroscopy-assisted masseter nerve avulsion on hemimasticatory spasm: an original research. Journal of Pharmacy and Bioallied Sciences, 15(Suppl 1), S110-S113.
Jaw Displacement
TMJ arthroscopy is a minimally invasive procedure to manage jaw displacements. Clinical reports find it to be a safe and effective treatment strategy for anterior displacements of the lower jaw. 6Zhu, Y., Zheng, C., Deng, Y., & Wang, Y. (2012). Arthroscopic surgery for treatment of anterior displacement of the disc without reduction of the temporomandibular joint. British Journal of Oral and Maxillofacial Surgery, 50(2), 144-148.
Contraindications Of TMJ Arthroscopy
You are not an ideal candidate for TMJ arthroscopy if there is:
- Presence of malignant tumors.
- Excessive resorption of the glenoid fossa.
- Advanced ankylosis (bony or fibrous) or ankylosing osteoarthritis
- High risk of hemorrhage
Benefits Of TMJ Arthroscopy
Better Diagnosis:
Mostly, oral surgeons perform a diagnostic arthroscopy when diagnosis can not be reached with conventional non-surgical diagnostic methods. TMJ arthroscopies provide plenty of data regarding the hard and soft tissues of the joint. However, the interpretation of this data requires wide experience and ample training in the field of temporomandibular disorders. This means that TMJ specialists can reach an accurate diagnosis via this technique.7Brüning, L. L., Rösner, Y., Meisgeier, A., & Neff, A. (2024). Arthroscopic Assessment of Temporomandibular Joint Pathologies—Is It Possible for Non-Specialists in Arthroscopy? Analysis of Variability and Reliability of Dental Students’ Ratings after a Comprehensive One-Semester Introduction. Journal of Clinical Medicine, 13(14), 3995.
Minimally Invasive:
The greatest benefit of therapeutic TMJ arthroscopy is that the procedure is minimally invasive. This gives it the advantage of better acceptability by the patient. Moreover, there are fewer complications like bleeding and scarring etc. Healing is also quick and mostly uneventful. Most patients are capable of returning to their masticatory capacity in a short period. Thus, patients have another reason to like TMJ arthroscopy.8Ângelo, D. F., Prior, A., & Cardoso, H. J. (2023). Postoperative Recovery after TMJ Arthroscopy: Masticatory Improvement and Postoperative Diet. Oral, 3(2), 191-202.
Treatment For Various TMDs:
TMJ arthroscopy serves as a treatment tool for various temporomandibular joint disorders. The effectiveness of this procedure is commendable. Minimally invasive procedures like arthroscopy help impart the following therapeutic benefits in TMJ disorders management:9Badri, O., Davis, C. M., & Warburton, G. (2024). Arthroscopic management and recent advancements in the treatment of temporomandibular joint disorders. British Journal of Oral and Maxillofacial Surgery, 62(9), 820-825.
- Alleviation of symptoms
- Improvement in joint function
- Enhancement of the overall quality of life
Levels Of Arthroscopy
Based on the complexity of the work, clinicians divide temporomandibular arthroscopy into three different levels:
Level Ⅰ: Diagnostic Arthroscopy:
This is the basic level of arthroscopy that primarily aims to provide diagnostic information. Surgeons perform a single puncture at this level. With an arthroscope, doctors can assess the extent of cartilage damage and the level of inflammation, etc. Additionally, doctors can perform simple therapeutic procedures.
Although this level is diagnostic, limited therapeutic interventions such as lysis of adhesions and lavage of the joint can be performed. In this context, lavage involves irrigating the joint space with sterile fluid to remove inflammatory mediators and improve joint mobility. While arthrocentesis also involves lavage, it is typically performed without arthroscopic guidance using two needles. In contrast, lavage during arthroscopy allows for direct visualization and precise targeting of adhesions, making it a more controlled approach.10Soni, A. (2019). Arthrocentesis of temporomandibular joint-bridging the gap between non-surgical and surgical treatment. Annals of maxillofacial surgery, 9(1), 158-167.
Lysis, or breaking down fibrous adhesions within the joint, is often paired with lavage to relieve joint stiffness and improve mouth opening. Studies have shown that combining these techniques results in significant improvement in maximum mouth opening and symptom relief. 11Lee, K. M., Jang, W. H., You, M. S., & Lee, B. K. (2021). An additional lysis procedure during arthrocentesis of the temporomandibular joint. Maxillofacial Plastic and Reconstructive Surgery, 43(1), 38.
Level Ⅱ: Operative Arthroscopy:
At level Ⅱ, doctors go for double punctures and position the surgical instruments and the arthroscope such that the working ends of the instruments form an imaginary triangle. This triangle formation is called triangulation. At this level, doctors are capable of performing complex surgical procedures like:
- Cutting (myotomy) of the lateral pterygoid muscle
- Ablation (removal) of retrodiscal tissue
- Tissue biopsy (to detect pathologies like neoplasms)
- Synovectomy (removal of the inflamed synovial membrane/lining)
- Disc manipulation
- Capsular stretch
Lateral pteryoid myotomy helps reduce repeated anterior displacement of the jaw. A 2023 study revealed that arthroscopy-assisted release of the lateral pterygoid muscle paired with ablation of retrodiscal tissues helped improve symptoms in patients who did not respond to conservative treatments in anteriorly displaced discs. The vast majority of patients reported the disappearance of clicking sounds.12Mosleh, A. A. E. L., Nowair, I. M., Saad, K. A. E. H., & Abd El-Mongy, A. E. F. (2023). Arthroscopic assisted release of lateral pterygoid versus scarification of retrodiscal tissue in management of internal derangement of temporomandibular joint-A randomized clinical trial. Journal of Cranio-Maxillofacial Surgery, 51(5), 303-308.
Repositioning of the problematic disc (disc manipulation) is done at this operative level, which leads to a resolution of symptoms. Your healthcare provider may use medical lasers (radiofrequency ablation device or holium YAG laser) or specialized surgical instruments for tissue cutting and coagulation. It is effective in the management of Wilkes Ⅱ and Ⅲ patients. Studies show that operative arthroscopy is superior to arthrocentesis in reducing postoperative pain and increasing mouth opening.13Atteya, A. M., Warda, M. H., Fata, M. M., Medra, A. M., & Gil, F. M. (2021). Prospective randomized study between arthrocentesis and operative arthroscopy in the management of temporomandibular joint internal derangement. Alexandria Dental Journal, 46(1), 58-65.
Level Ⅲ: Advanced Operative Arthroscopy:
At this advanced level of intervention, doctors carry out even more complex TMJ procedures. One of the most common procedures is the correction of TMJ disc displacement. To tackle advanced disease, surgeons perform procedures like meniscal repair or discopexy (fixation of the disc) and meniscectomy. For discopexy, doctors usually go for multiple punctures. They reposition and maintain the disc’s position with the help of special instruments and sutures.
Discopexy Techniques
Based on the condition, professionals adopt different techniques of discopexy, including non-rigid fixation, semi-rigid fixation, and rigid fixation. Recent studies show that the semi-rigid technique yields the best results in mouth opening and pain.14López, J. P., Orjuela, M. P., Diaz-Baez, D., & González, L. V. (2024). Comparison of the TMJ arthroscopy discopexy techniques: A systematic review and meta-analysis. Journal of Cranio-Maxillofacial Surgery, 52(5), 558-564. In non-rigid fixation, sutures are placed on the lateral aspect of the joint capsule, and in semi-rigid fixation, they are anchored to the tragus cartilage. However, in rigid fixation, doctors use resorbable pins (or anchors) to the glenoid fossa or the condyle to fix the disc in place.
Another technique, called Yang’s technique, has shown good results in managing disc problems. In this specific technique, doctors insert sutures through the junction of the disc (and the retrodiscal tissues) and tie them under the external auditory canal. This technique is easier to follow. The positive impact of arthroscopic discopexy in internal derangement has been proven by studies. The minimally invasive procedure helps restore the bony structure, increases disc length, and alleviates symptoms.15Sah, M. K., Abdelrehem, A., Chen, S., & Yang, C. (2023). Arthroscopic discopexy versus natural course of temporomandibular joint anterior disc displacement: a longitudinal study of clinical and radiological outcomes. International Journal of Oral and Maxillofacial Surgery, 52(1), 98-106.
In severe, unresolving cases of jaw clicking and pain, surgeons remove the meniscus (fibrocartilagenous structure between the mandible and the temporal bone of the skull) with the help of an arthroscope.
TMJ Arthroscopy Procedure
Arthroscopy of the temporomandibular joint is a simple procedure generally completed within a couple of hours. The duration of the minimal surgery can range anywhere between 30 minutes and 2 hours, depending on the level of arthroscopy.
The steps of the procedure are as follows:
Anesthesia:
Surgeons typically perform TMJ arthroscopy under general anesthesia.
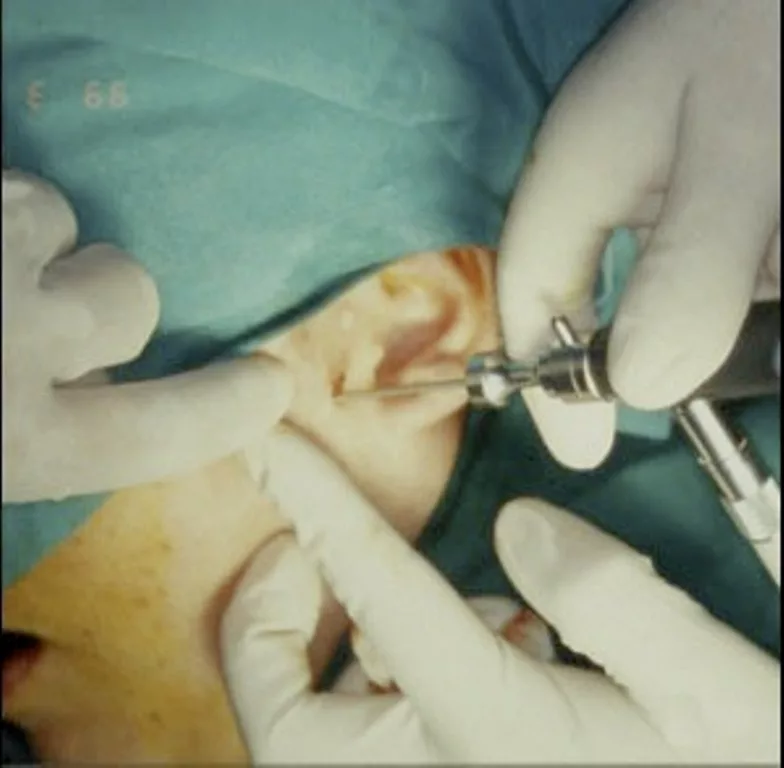
Incision:
A small skin incision is made just in front of the ear, typically along the tragus-lateral canthus line, allowing entry into the superior joint space through a minimally invasive approach. Surgeons then insert the arthroscope through this keyhole to visualize and treat intra-articular structures.
Depending on the patient’s anatomy and the type of procedure, oral and maxillofacial surgeons may choose from several arthroscopic portals, including:
- Superior postolateral approach
- Inferior postolateral approach
- Superior anterolateral approach
- Inferior anterolateral approach
- Endaural approach (less common in arthroscopy)
These access points allow for triangulation of instruments and optimal visualization during diagnostic or therapeutic procedures.
Arthroscope Insertion:
After incision, a thin tube with light, i.e, the arthroscope, along with a camera, is inserted into the joint space. The images taken by the camera inside are displayed on a monitor that allows the health professional to visualize the joint in real time. It helps in diagnosing the problem and fixing it.
Surgical Intervention:
For diagnostic arthroscopy, doctors give only one incision/puncture. However, in the case of operative and advanced operative arthroscopies, 2 or more incisions are made to insert additional surgical instruments. After carefully positioning the instruments inside, the surgeon can perform lavage, lysis, tissue biopsy, repositioning of the disc, etc. Advanced operations like discopexy and meniscectomy may also be performed. Many doctors use arthroscopy to inject useful medicines into the intraarticular space.
Stitch Up:
After completion of the surgery, doctors close the wound with the help of sutures.
TMJ Arthroscopy Recovery
Due to the minimal exposure, recovery is quick. Most patients return home on the same day and can resume routine activities within a few days. However, patients who have undergone advanced operative procedures may take up to a week to return to their normal routine. You might feel some pain, bruising, and swelling on the surgical site for a few days after the procedure, but don’t worry, that is normal. Most patients notice alleviation of symptoms and improvements in mouth opening by the end of 3rd week.
Post TMJ Arthroscopy Care:
You can adopt the following steps to speed up healing and prevent complications:
- Shift to a softer diet for the first week to prevent injury and strain on the jaw.
- Apply cold to the wound site to lower inflammation.
- Take over-the-counter pain killer medications to manage postoperative pain.
- Strictly follow your doctor’s prescription and schedule appointments regularly.
- Perform gentle jaw exercises (as prescribed by your doctor) to reduce joint stiffness and restore movement range.
- Physiotherapy is also known to improve function and increase the range of motion in patients.16Abboud, W. A., Yarom, N., Yahalom, R., Joachim, M., Reiter, S., Koren, O., & Elishoov, H. (2018). Comparison of two physiotherapy programmes for rehabilitation after temporomandibular joint arthroscopy. International journal of oral and maxillofacial surgery, 47(6), 755-761.
TMJ Arthroscopy Complications
Even minimally invasive surgical interventions like TMJ arthroscopy can have some complications. Common side effects include swelling, bruising, and some discomfort. Infection of the surgical site can also develop. Some patients experience temporary jaw stiffness, which typically resolves over time.
Though uncommon, the following complications have also been observed in arthroscopy cases:
- Temporary deficit of the trigeminal nerve (affects sensations and muscle control of the face/mouth)
- Partial hearing loss
- Temporary facial nerve paresis (facial paralysis)
- Soft palate/parapharyngeal and preauricular edema
The overall complication rate of the procedure was found to be 7.7%.17González-García, R., & Monje, F. (2024). Complications of temporomandibular joint arthroscopy. A critical appraisal of the literature. Journal of Cranio-Maxillofacial Surgery, 52(10), 1122-1132.
Final Word
TMJ arthroscopy is a minimally invasive surgical procedure to diagnose and treat disorders of the temporomandibular joint. Doctors insert an arthroscope (a camera to visualize the inside of the joint) and surgical instruments in the joint through a small incision (keyhole). An arthroscopy is beneficial in the management of internal derangement, TMJ osteoarthritis, suspected cancers (for biopsy), and disc issues, etc.
Level Ⅰ of arthroscopy involves diagnosing the issue and carrying out small procedures like joint lavage (arthrocentesis) and breakage of scar tissues (lysis of adhesions). Levels Ⅱ and Ⅲ are characterized by extensive operative procedures like synovectomy, myotomy, and disc manipulation, etc. Performed with lasers, the process is short, and healing is quick. It effectively reduces clicking, joint stiffness, pain and improves joint movement. However, patients may experience postoperative temporary stiffness, muscle paralysis, and sensation/hearing loss, which go away with time.
Refrences
- 1Ângelo, D. F., Sanz, D., & Cardoso, H. J. (2023). Bilateral arthroscopy of the temporomandibular joint: clinical outcomes and the role of a second intervention—a prospective study. Clinical oral investigations, 27(10), 6167-6176.
- 2Al-Moraissi EA. Arthroscopy versus arthrocentesis in the management of internal derangement of the temporomandibular joint: a systematic review and meta-analysis. Int J Oral Maxillofac Surg. 2015 Jan;44(1):104-12. doi: 10.1016/j.ijom.2014.07.008. Epub 2014 Aug 7. PMID: 25123511.
- 3Mélou, C., Pellen-Mussi, P., Jeanne, S., Novella, A., Tricot-Doleux, S., & Chauvel-Lebret, D. (2022). Osteoarthritis of the temporomandibular joint: a narrative overview. Medicina, 59(1), 8.
- 4Muñoz-Guerra, M. F., Rodríguez-Campo, F. J., Escorial-Hernández, V., Sanz-García, A., Brabyn, P. J., & Fernández-Domínguez, M. (2022). Temporomandibular joint arthroscopy in advanced stages of internal derangement: a retrospective cohort study on the influence of age. International Journal of Oral and Maxillofacial Surgery, 51(12), 1579-1586.
- 5Pillai, A. R., Kumar, G. J., Kumar, P., Nizar, S. A., Pendyala, S. K., & Baig, F. A. H. (2023). Assessment of the efficacy of TMJ arthroscopy-assisted masseter nerve avulsion on hemimasticatory spasm: an original research. Journal of Pharmacy and Bioallied Sciences, 15(Suppl 1), S110-S113.
- 6Zhu, Y., Zheng, C., Deng, Y., & Wang, Y. (2012). Arthroscopic surgery for treatment of anterior displacement of the disc without reduction of the temporomandibular joint. British Journal of Oral and Maxillofacial Surgery, 50(2), 144-148.
- 7Brüning, L. L., Rösner, Y., Meisgeier, A., & Neff, A. (2024). Arthroscopic Assessment of Temporomandibular Joint Pathologies—Is It Possible for Non-Specialists in Arthroscopy? Analysis of Variability and Reliability of Dental Students’ Ratings after a Comprehensive One-Semester Introduction. Journal of Clinical Medicine, 13(14), 3995.
- 8Ângelo, D. F., Prior, A., & Cardoso, H. J. (2023). Postoperative Recovery after TMJ Arthroscopy: Masticatory Improvement and Postoperative Diet. Oral, 3(2), 191-202.
- 9Badri, O., Davis, C. M., & Warburton, G. (2024). Arthroscopic management and recent advancements in the treatment of temporomandibular joint disorders. British Journal of Oral and Maxillofacial Surgery, 62(9), 820-825.
- 10Soni, A. (2019). Arthrocentesis of temporomandibular joint-bridging the gap between non-surgical and surgical treatment. Annals of maxillofacial surgery, 9(1), 158-167.
- 11Lee, K. M., Jang, W. H., You, M. S., & Lee, B. K. (2021). An additional lysis procedure during arthrocentesis of the temporomandibular joint. Maxillofacial Plastic and Reconstructive Surgery, 43(1), 38.
- 12Mosleh, A. A. E. L., Nowair, I. M., Saad, K. A. E. H., & Abd El-Mongy, A. E. F. (2023). Arthroscopic assisted release of lateral pterygoid versus scarification of retrodiscal tissue in management of internal derangement of temporomandibular joint-A randomized clinical trial. Journal of Cranio-Maxillofacial Surgery, 51(5), 303-308.
- 13Atteya, A. M., Warda, M. H., Fata, M. M., Medra, A. M., & Gil, F. M. (2021). Prospective randomized study between arthrocentesis and operative arthroscopy in the management of temporomandibular joint internal derangement. Alexandria Dental Journal, 46(1), 58-65.
- 14López, J. P., Orjuela, M. P., Diaz-Baez, D., & González, L. V. (2024). Comparison of the TMJ arthroscopy discopexy techniques: A systematic review and meta-analysis. Journal of Cranio-Maxillofacial Surgery, 52(5), 558-564.
- 15Sah, M. K., Abdelrehem, A., Chen, S., & Yang, C. (2023). Arthroscopic discopexy versus natural course of temporomandibular joint anterior disc displacement: a longitudinal study of clinical and radiological outcomes. International Journal of Oral and Maxillofacial Surgery, 52(1), 98-106.
- 16Abboud, W. A., Yarom, N., Yahalom, R., Joachim, M., Reiter, S., Koren, O., & Elishoov, H. (2018). Comparison of two physiotherapy programmes for rehabilitation after temporomandibular joint arthroscopy. International journal of oral and maxillofacial surgery, 47(6), 755-761.
- 17González-García, R., & Monje, F. (2024). Complications of temporomandibular joint arthroscopy. A critical appraisal of the literature. Journal of Cranio-Maxillofacial Surgery, 52(10), 1122-1132.





