Priapism is a full or partial erection that continues for more than 4 hours, unrelated to sexual stimulation and ejaculation. The term comes from Priapus, the Greek god of fertility, often depicted with an exaggerated erection.
This condition develops when blood becomes trapped in the penis and cannot drain. The resulting erection is usually, but not always, painful. It’s rare (1.5 per 100,000 men annually),1Eland, I. A., van der Lei, J., Stricker, B. H., & Sturkenboom, M. J. (2001). Incidence of priapism in the general population. Urology, 57(5), 970–972. but when it does happen, it typically affects males in their 30s. Blood disorders and some medications are among the most common causes.
Major health organizations like The American Urological Association (AUA) recognize priapism as a urologic emergency because without proper and immediate treatment, it can cause scarring of the penis and permanent erectile dysfunction.2Bivalacqua TJ, Allen BK, Brock GB, et al. The diagnosis and management of recurrent ischemic priapism, priapism in sickle cell patients, and non-ischemic priapism: an AUA/SMSNA guideline. J Urol. 2022;208(1):43-52.
Types of Priapism
It is classified according to the cause and blood flow dynamics involved.
Ischemic Priapism (Low-Flow):
It’s the most common and most dangerous form of priapism, accounting for more than 95% of the cases.3Capece M, Falcone M, Cai T, et al. : Penile Prosthesis Implantation in Refractory Ischaemic Priapism: Patient Selection and Special Considerations. Res Rep Urol. 2022; 14: 1–6.
It results from venous outflow obstruction: blood enters the penis but gets trapped in the corpora cavernosa. As oxygenated blood can’t circulate, the tissue becomes hypoxic and acidotic, increasing the risk of necrosis and permanent damage. The shaft becomes rigid and painful, and the longer it persists, the higher the risk of permanent damage.4Alnajjar, H. M., & Muneer, A. (2022). Recent advances in understanding and treating priapism. Faculty reviews, 11, 23.
It’s typically caused by impaired relaxation of cavernosal smooth muscle or obstruction of venous drainage. Common triggers include sickle cell disease, certain medications (e.g., trazodone, antipsychotics), and intracavernosal injections (for ED).
Non-Ischemic Priapism (High-Flow):
This type is less common and usually painless. It usually follows blunt trauma to the perineum or penis, which creates an abnormal connection between an artery and erectile tissue (arteriocavernosal fistula).
Because blood is still oxygenated and circulating, the erection is typically only partially rigid, not fully firm. and the risk of tissue damage is lower.5Alnajjar, H. M., & Muneer, A. (2022). Recent advances in understanding and treating priapism. Faculty reviews, 11, 23.
Unlike ischemic priapism, it’s not an emergency, and resolution is possible.
Stuttering Priapism (Recurrent Ischemic Priapism):
This is the rarest type of the disease, but it’s chronic, with repeated episodes of ischemic priapism. The erections are usually painful, last less than four hours, and are unpredictable, sometimes days apart, sometimes several in a single day.6Alnajjar, H. M., & Muneer, A. (2022). Recent advances in understanding and treating priapism. Faculty reviews, 11, 23.
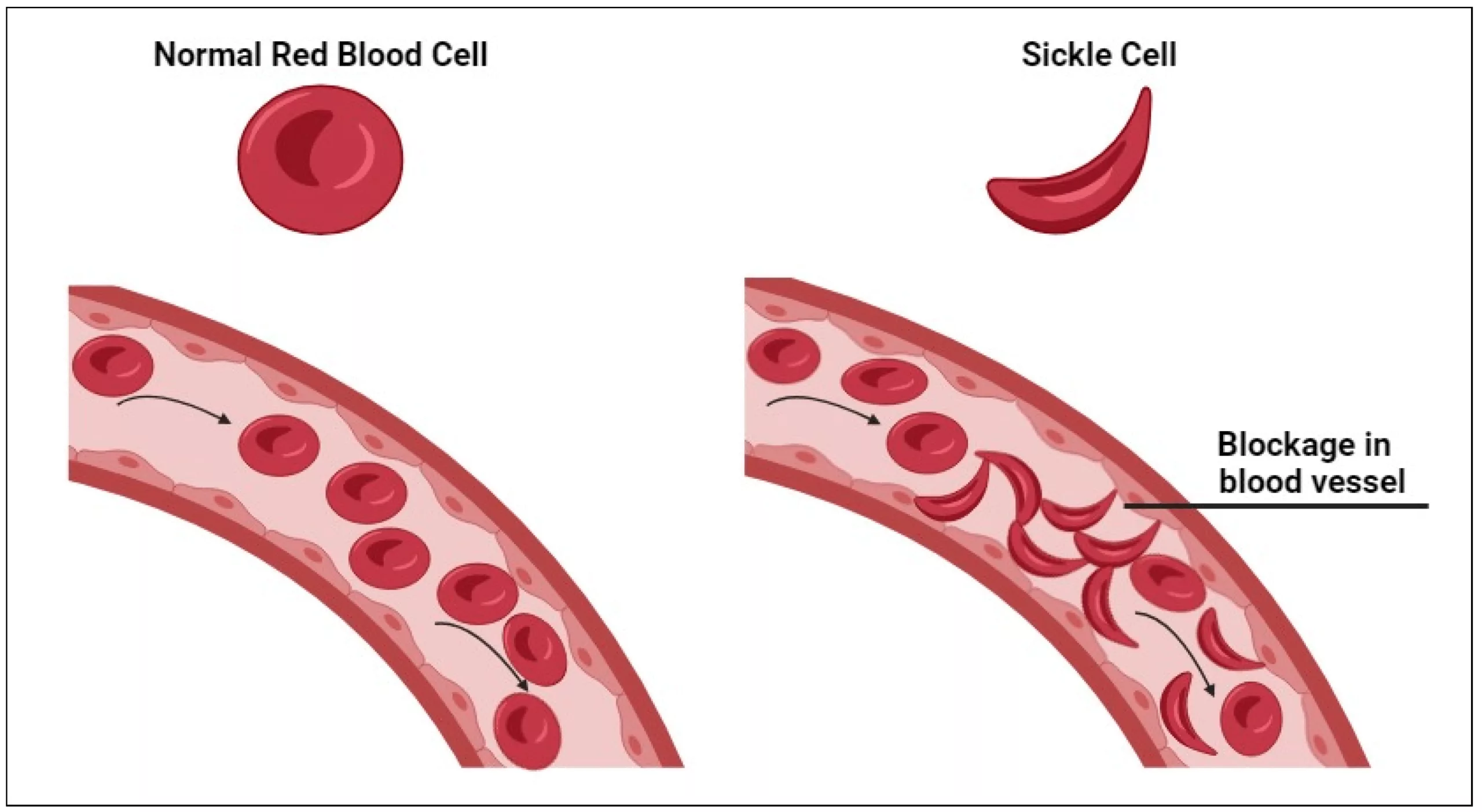
Most common in patients with sickle cell disease, where vaso-occlusion causes transient ischemia. Over time, these episodes can progress to full ischemic priapism and increase the risk of erectile dysfunction.
Triggers include fever, dehydration, alcohol, and sexual arousal, but sometimes there is no identifiable factor.
Causes & Risk Factors of Priapism
Priapism is uncommon, but it’s usually due to an underlying condition or trigger that disrupts normal blood flow.
- In children and young adults, sickle cell disease (SCD) is the most common cause, responsible for up to 42% of ischemic priapism cases. 7Ahuja, G., Ibecheozor, C., Okorie, N. C., Jain, A. J., Coleman, P. W., Metwalli, A. R., & Tonkin, J. B. (2021). Priapism and Sickle Cell Disease: Special Considerations in Etiology, Management, and Prevention. Urology, 156, e40–e47. The sickling of red blood cells causes microvascular occlusion and hypoxia in the corpora cavernosa.
- Drug-induced priapism is another major cause. This includes erectile dysfunction meds like sildenafil, trazodone (an antidepressant), and antipsychotics like risperidone; recreational substances like cocaine and alcohol cause up to 20% of cases.8Rezaee, M. E., & Gross, M. S. (2020). Are We Overstating the Risk of Priapism With Oral Phosphodiesterase Type 5 Inhibitors?. The journal of sexual medicine, 17(8), 1579–1582.
- Blood malignancies (e.g., leukemia, thalassemia) and neurological disorders (e.g., spinal cord injuries) also contribute. Blunt perineal trauma causes most cases of non-ischemic priapism. In 5–10% of adults, no cause is found (idiopathic priapism).
Risk Factors:
This condition is uncommon, but it tends to affect the following individuals most:
- Males aged 20-50
- Children with sickle cell disease9Ahuja, G., Ibecheozor, C., Okorie, N. C., Jain, A. J., Coleman, P. W., Metwalli, A. R., & Tonkin, J. B. (2021). Priapism and Sickle Cell Disease: Special Considerations in Etiology, Management, and Prevention. Urology, 156, e40–e47.
- Individuals with blood-related issues (e.g., leukemia or thalassemia)
- Users of ED drugs, antidepressants, antipsychotics, or alpha-blockers10Ahuja, G., Ibecheozor, C., Okorie, N. C., Jain, A. J., Coleman, P. W., Metwalli, A. R., & Tonkin, J. B. (2021). Priapism and Sickle Cell Disease: Special Considerations in Etiology, Management, and Prevention. Urology, 156, e40–e47.
- Those with HIV/AIDS or recent COVID-19 infection11Creta, M., Sagnelli, C., Celentano, G., Napolitano, L., La Rocca, R., Capece, M., Califano, G., Calogero, A., Sica, A., Mangiapia, F., Ciccozzi, M., Fusco, F., Mirone, V., Sagnelli, E., & Longo, N. (2021). SARS-CoV-2 infection affects the lower urinary tract and male genital system: A systematic review. Journal of medical virology, 93(5), 3133–3142.
- History of recent trauma to the genitals, pelvis, or spine
- Users of recreational drugs, cocaine, and alcohol
Symptoms of Priapism
The main symptom of this condition is an erection that lasts more than four hours. However, different types of priapism have their own variable symptoms and levels of urgency.
Symptoms of Ischemic (Low-Flow) Priapism:
- Persistent, painful erection, rigid shaft with a soft or flaccid glans
- Worsening pain over a period of time
- Tenderness or swelling in the penis
- No relief with ejaculation
- Possible discoloration (dark red or bluish hue)
This is a medical emergency. It doesn’t allow oxygen rich blood to reach the tissues of the penis. If not relieved, this can cause permanent damage to the tissue.
Symptoms of Non-Ischemic (High-Flow) Priapism:
- An erection that’s not fully rigid
- Usually painless
- Often follows injury to the pelvis or perineum
- It may go away on its own
Because this type doesn’t involve trapped, oxygen-deprived blood, it’s less urgent, but still important to get it checked to rule out complications.
Symptoms of Stuttering Priapism:
- Repeated episodes of short-lived, painful erections
- Each episode typically lasts under 4 hours
- More common in people with sickle cell disease
Even if the episodes stop on their own, repeated attacks can evolve into a full ischemic crisis.
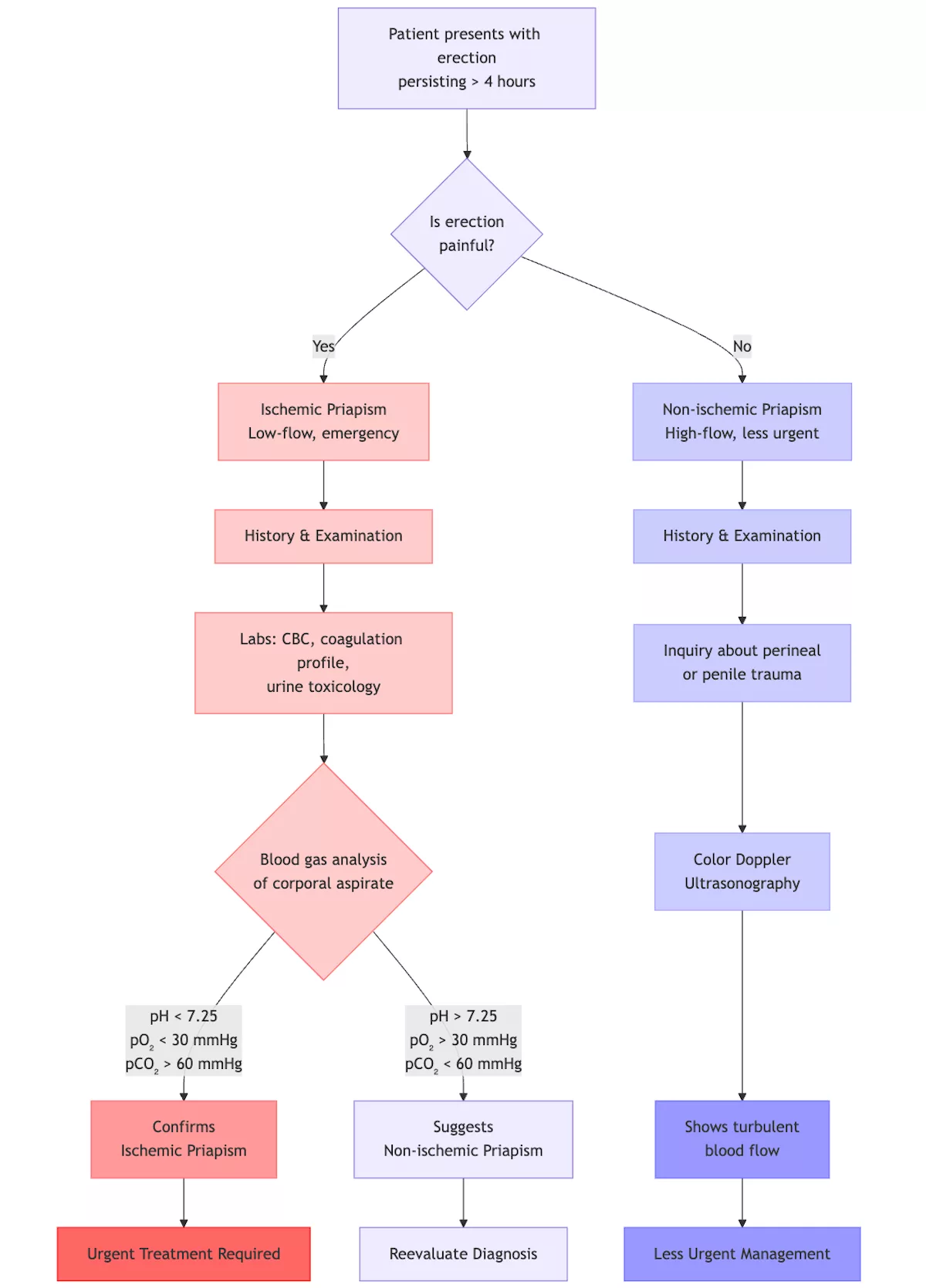
Diagnosis of Priapism
Diagnosis focuses on differentiating between emergency and non-emergency types and helping doctors prevent lasting damage.12Bivalacqua TJ, Allen BK, Brock GB, et al. The diagnosis and management of recurrent ischemic priapism, priapism in sickle cell patients, and non-ischemic priapism: an AUA/SMSNA guideline. J Urol. 2022;208(1):43-52.
Medical History & Physical Exam:
The first step is usually a quick but thorough assessment:
- When did the erection start?
- Is there any pain, and if so, where?
- Are you taking any medications?
- Do you have a history of blood disorders or trauma?
During the physical exam, the doctor will check:
- Whether the erection is fully rigid or partially soft.
- Any visible signs of injury, swelling, or discoloration.
Blood Gas Analysis (Penile Blood Test):
This is a key test that involves drawing a small sample of blood directly from the penis using a needle.
- Dark, low-oxygen blood → Ischemic
- Bright red, oxygenated blood → Non-ischemic
Blood Tests:
To identify or rule out underlying causes:
- Complete Blood Count (CBC) to check for blood disorders
- Sickle cell testing (especially in younger males or those with a family history)
- Toxicology screen if drug-related causes are suspected
Doppler Ultrasound:
Organizations like the American Urological Association (AUA), British Association of Urological Surgeons (BAUS), and the European Association of Urology (EAU) recommend the use of Doppler ultrasound to distinguish between low-flow and high-flow types.13Bivalacqua TJ, Allen BK, Brock GB, et al. The diagnosis and management of recurrent ischemic priapism, priapism in sickle cell patients, and non-ischemic priapism: an AUA/SMSNA guideline. J Urol. 2022;208(1):43-52.
- Assess blood flow in and out of the penile arteries
- Detect trauma, abnormal connections, or clots
- Confirm the diagnosis when other tests are inconclusive
Additional Imaging (if needed):
In rare or complicated cases, your doctor might recommend:
- MRI or CT scan if there’s concern about a tumor or spinal cord involvement
- Pelvic imaging if trauma was involved
Differential Diagnosis
There are a lot of diseases with symptoms that involve penile pain, swelling, and priapism-like complaints. These should be ruled out, even after history and exam, before a final diagnosis can be made.
The most common conditions to exclude, and the differentiating points are:
- Paraphimosis: The foreskin becomes trapped behind the head of the penis, causing swelling and a painful, engorged penis. However, the erection is not persistent.
- Penile Fracture: It leads to sudden pain, swelling, and sometimes a cracking sound. Unlike priapism, the erection usually disappears after the injury.
- Urethral Obstruction: This causes difficulty urinating, which might make the penis feel swollen or tense, but doesn’t usually involve an erection.
- Penile Cancer: Tumors in or around the penis or pelvis can mimic high-flow priapism by disturbing blood flow or causing pressure buildup.
- Infectious or Inflammatory Conditions: Balanitis (inflammation of the glans) or cellulitis may cause swelling and pain, but not prolonged erections.
Priapism vs Paraphimosis
| Feature | Priapism | Paraphimosis14Choe J. M. (2000). Paraphimosis: current treatment options. American family physician, 62(12), 2623–2628. |
|---|---|---|
| Cause | Blood flow imbalance | Trapped foreskin |
| Erection | Persistent (often painful) | Usually absent |
| Glans (tip) | Often soft (in ischemic priapism) | Swollen, possibly discolored |
| Urgency | Emergency (esp. ischemic) | Emergency |
| Treatment | Blood drainage, meds | Manual reduction or minor procedure |
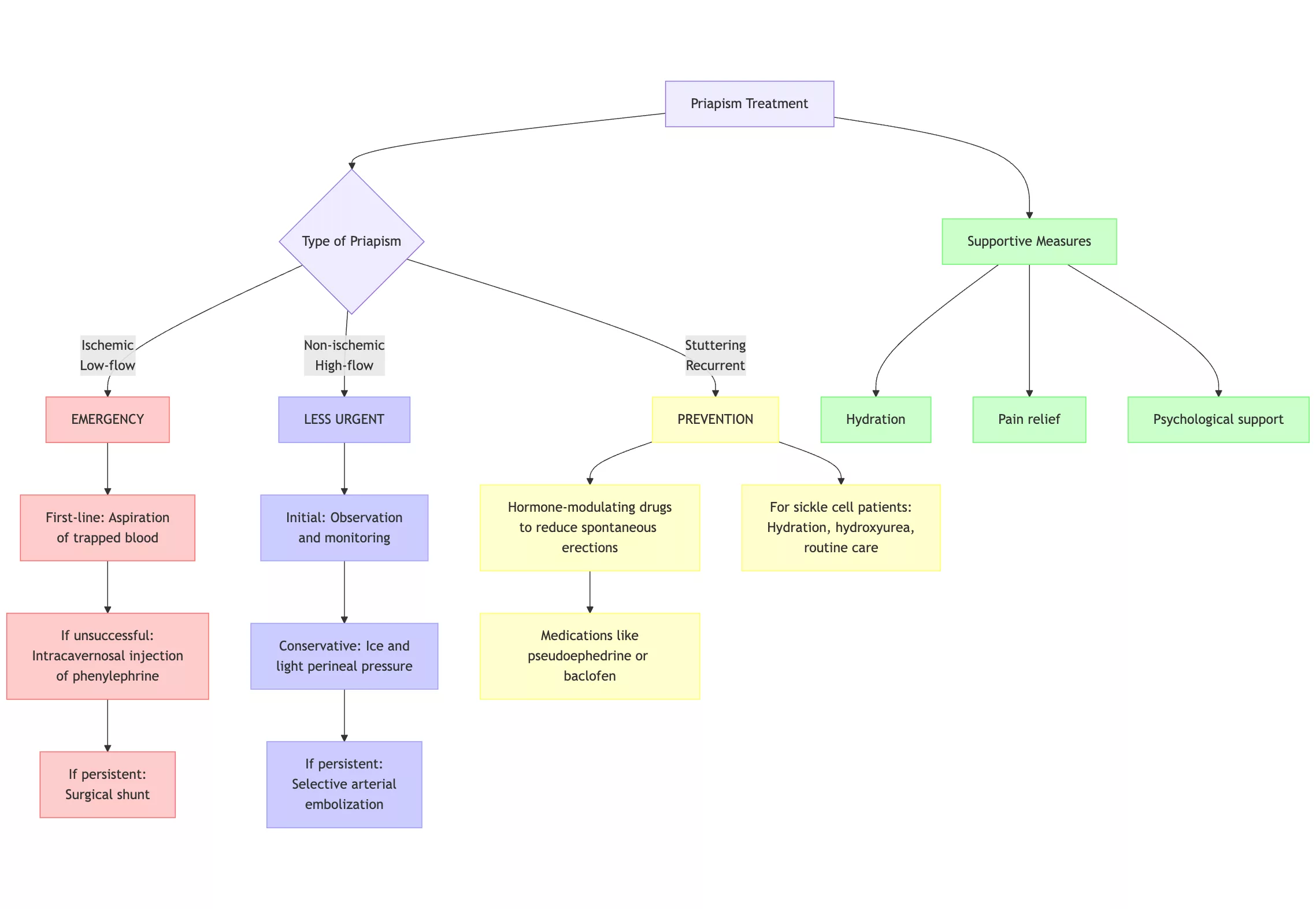
Treatment Options for Priapism
The main management goal is to relieve the erection and prevent permanent damage. Other than supportive measures like hydration, pain relief, and psychological support, specific treatment depends upon the type of priapism.15Bivalacqua TJ, Allen BK, Brock GB, et al. The diagnosis and management of recurrent ischemic priapism, priapism in sickle cell patients, and non-ischemic priapism: an AUA/SMSNA guideline. J Urol. 2022;208(1):43-52.
For Ischemic (Low-Flow) Priapism:
Immediate action is needed to restore normal blood flow and protect erectile tissue.
- The first-line treatment in hospitals is immediate aspiration where a fine needle is used to draw out trapped blood from the penis.
- If aspiration doesn’t work, a drug like phenylephrine (a vasoconstrictor) is injected directly into the penis (Intracavernosal) to help narrow blood vessels and encourage drainage.
- In severe or prolonged cases, surgeons may create a small passage (shunt) to redirect blood flow out of the penis.
For Non-Ischemic (High-Flow) Priapism:
This type is less urgent and often resolves on its own.
- If there’s no pain and the erection is partial, doctors may simply monitor the situation. Many high-flow cases resolve without intervention.
- Applying ice and light pressure to the perineum may help slow blood flow and ease the erection.
- If the condition persists, an interventional radiologist may block the injured artery, causing the issue.
For Stuttering Priapism:
Recurring priapism can result in permanent erectile dysfunction. The goal is to prevent these episodes, especially in patients with sickle cell disease.
- Hormone-modulating drugs are used to reduce spontaneous erections, especially in adolescents or those with frequent episodes.
- Medications like pseudoephedrine or baclofen are used to reduce the frequency and severity.
- For sickle cell patients, preventing crises through proper hydration, medication (like hydroxyurea), and routine care can reduce episodes.
Complications of Priapism
Beyond the physical, there’s the emotional toll: chronic episodes can cause significant stress and strain on personal relationships. If not treated in time, this condition can have serious consequences:
- Permanent erectile dysfunction
- Scar tissue formation in the penis
- Damage to blood vessels and nerves
- Emotional stress or relationship strain
Conclusion
It is rare, but ignoring it can lead to serious complications, permanent erectile dysfunction, and tissue damage. If your erection lasts more than four hours, especially if it’s painful or discolored, seek medical help immediately.
This also applies if you’ve had repeated episodes, recently started a new medication, or have a blood-related condition like sickle cell disease or leukemia. In this case, prevention matters. Stay well hydrated, manage underlying health issues, and avoid known triggers like certain medications or recreational drugs. If you’ve had priapism before, even brief episodes should be monitored to catch warning signs early.
Refrences
- 1Eland, I. A., van der Lei, J., Stricker, B. H., & Sturkenboom, M. J. (2001). Incidence of priapism in the general population. Urology, 57(5), 970–972.
- 2Bivalacqua TJ, Allen BK, Brock GB, et al. The diagnosis and management of recurrent ischemic priapism, priapism in sickle cell patients, and non-ischemic priapism: an AUA/SMSNA guideline. J Urol. 2022;208(1):43-52.
- 3Capece M, Falcone M, Cai T, et al. : Penile Prosthesis Implantation in Refractory Ischaemic Priapism: Patient Selection and Special Considerations. Res Rep Urol. 2022; 14: 1–6.
- 4Alnajjar, H. M., & Muneer, A. (2022). Recent advances in understanding and treating priapism. Faculty reviews, 11, 23.
- 5Alnajjar, H. M., & Muneer, A. (2022). Recent advances in understanding and treating priapism. Faculty reviews, 11, 23.
- 6Alnajjar, H. M., & Muneer, A. (2022). Recent advances in understanding and treating priapism. Faculty reviews, 11, 23.
- 7Ahuja, G., Ibecheozor, C., Okorie, N. C., Jain, A. J., Coleman, P. W., Metwalli, A. R., & Tonkin, J. B. (2021). Priapism and Sickle Cell Disease: Special Considerations in Etiology, Management, and Prevention. Urology, 156, e40–e47.
- 8Rezaee, M. E., & Gross, M. S. (2020). Are We Overstating the Risk of Priapism With Oral Phosphodiesterase Type 5 Inhibitors?. The journal of sexual medicine, 17(8), 1579–1582.
- 9Ahuja, G., Ibecheozor, C., Okorie, N. C., Jain, A. J., Coleman, P. W., Metwalli, A. R., & Tonkin, J. B. (2021). Priapism and Sickle Cell Disease: Special Considerations in Etiology, Management, and Prevention. Urology, 156, e40–e47.
- 10Ahuja, G., Ibecheozor, C., Okorie, N. C., Jain, A. J., Coleman, P. W., Metwalli, A. R., & Tonkin, J. B. (2021). Priapism and Sickle Cell Disease: Special Considerations in Etiology, Management, and Prevention. Urology, 156, e40–e47.
- 11Creta, M., Sagnelli, C., Celentano, G., Napolitano, L., La Rocca, R., Capece, M., Califano, G., Calogero, A., Sica, A., Mangiapia, F., Ciccozzi, M., Fusco, F., Mirone, V., Sagnelli, E., & Longo, N. (2021). SARS-CoV-2 infection affects the lower urinary tract and male genital system: A systematic review. Journal of medical virology, 93(5), 3133–3142.
- 12Bivalacqua TJ, Allen BK, Brock GB, et al. The diagnosis and management of recurrent ischemic priapism, priapism in sickle cell patients, and non-ischemic priapism: an AUA/SMSNA guideline. J Urol. 2022;208(1):43-52.
- 13Bivalacqua TJ, Allen BK, Brock GB, et al. The diagnosis and management of recurrent ischemic priapism, priapism in sickle cell patients, and non-ischemic priapism: an AUA/SMSNA guideline. J Urol. 2022;208(1):43-52.
- 14Choe J. M. (2000). Paraphimosis: current treatment options. American family physician, 62(12), 2623–2628.
- 15Bivalacqua TJ, Allen BK, Brock GB, et al. The diagnosis and management of recurrent ischemic priapism, priapism in sickle cell patients, and non-ischemic priapism: an AUA/SMSNA guideline. J Urol. 2022;208(1):43-52.