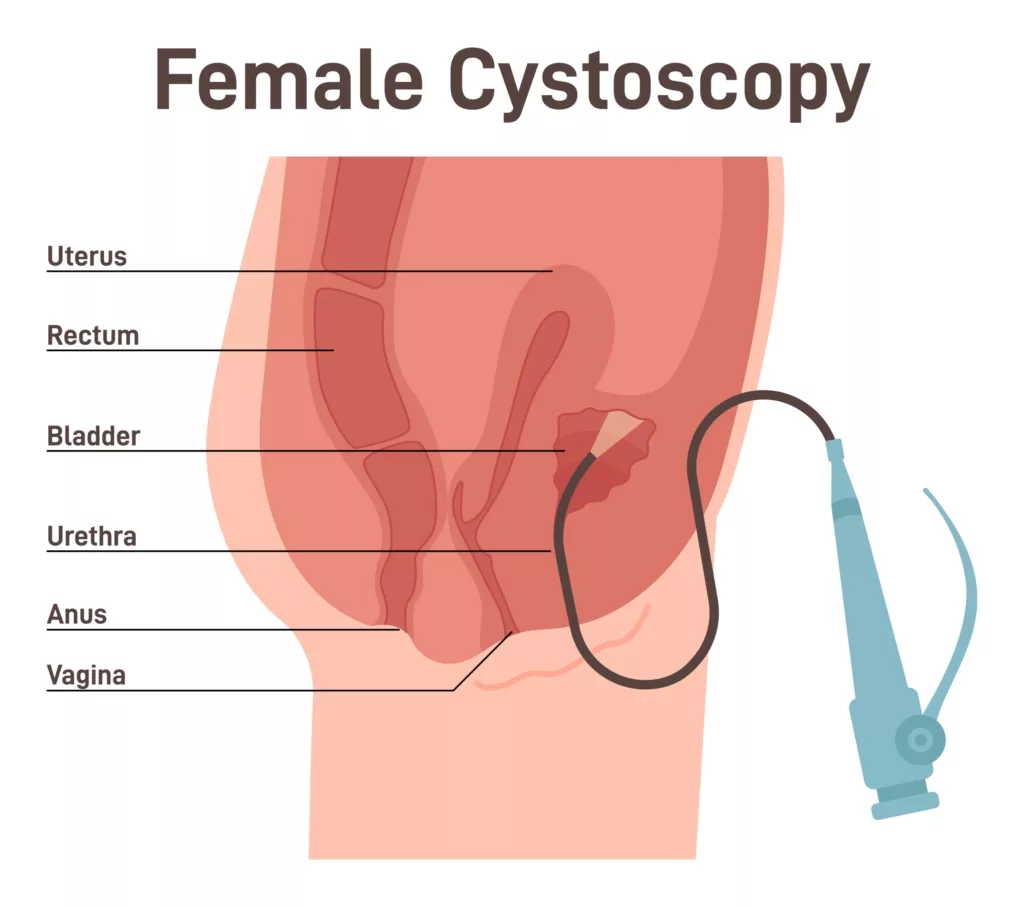
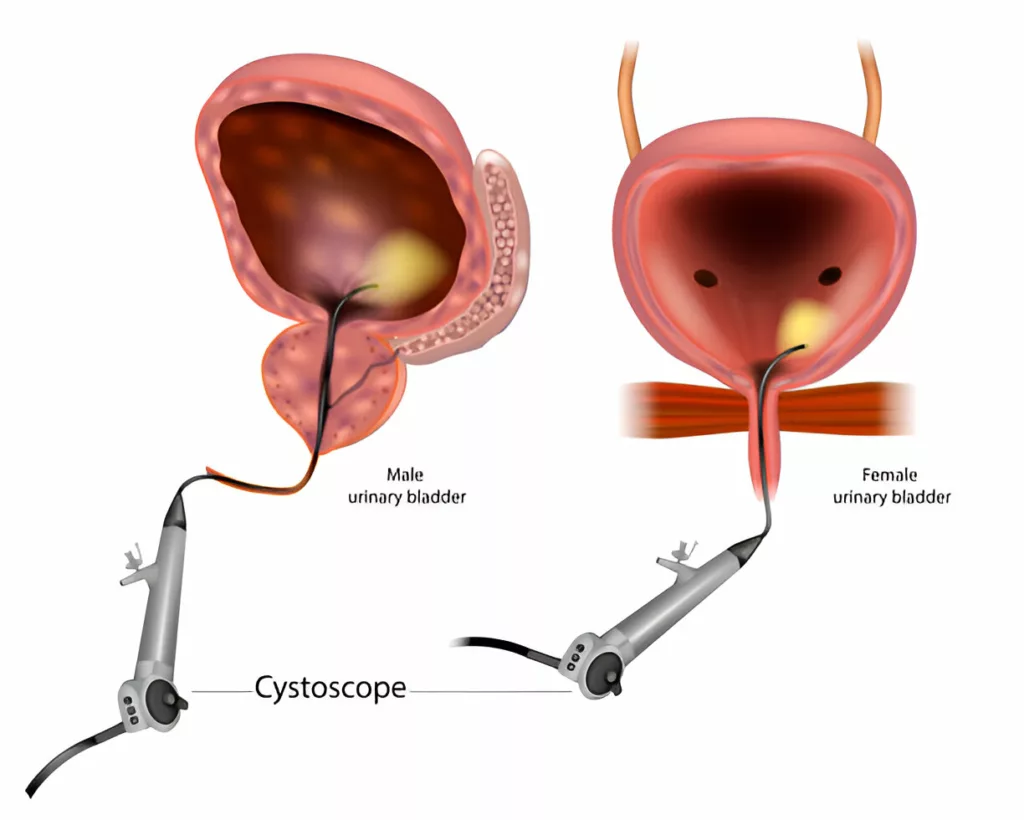
Cystoscopy is the procedure for visually inspecting the inside of your bladder and urethra. Healthcare professionals perform it using a thin, flexible or rigid instrument called a cystoscope, which has a camera and light at its tip. This procedure is commonly performed to diagnose and treat various urinary tract conditions, ranging from recurrent infections to bladder cancer. It can be done in different settings, including a doctor’s office, outpatient clinic, or operating room, depending on the complexity of the procedure. Depending on the type of cystoscopy performed, patients may receive a topical anesthetic gel, local anesthesia, sedation, or general anesthesia to ensure comfort during the procedure.1Matulewicz, R.S., J.O. DeLancey, and J.J. Meeks, Cystoscopy. JAMA, 2017. 317(11): p. 1187-1187.
Cystoscopy Indications
Cystoscopy is a diagnostic tool in urology and urogynecology practice. Urologists can use it for:
- Getting samples of urine from your ureters
- Injecting medicines
- Injecting dye to track urine flow
- Removal and insertion of ureteral stents
- Take samples of urethral or bladder tissues for biopsy.
The common diagnostic indications of cystoscopy include:
- Recurrent urinary tract infections (UTIs) (presence of more than two UTIs in a period of six months or three UTIs over one year or more).
- Urethral syndrome
- Abnormal urine cytology
- Bladder abnormalities in imaging studies
- Microscopic or macroscopic haematuria
- Bladder pain syndrome (Interstitial cystitis and chronic pelvic pain)2Acar, Ö. and T. Tarcan, Cystoscopic evaluation and clinical phenotyping in interstitial cystitis/bladder pain syndrome. Journal of the Turkish German Gynecological Association, 2019. 20(2): p. 117.
- Voiding abnormalities
- Assessment of urinary fistula3Tamilselvi, A., Role of Cystoscopy. Ambulatory Urology and Urogynaecology, 2021: p. 53-61.
- Intra-operative inspection of ureteral, bladder, or urethral integrity during pelvic surgeries or anti-continence procedures
- Overactive bladder symptoms
- Assessment of anterior wall vaginal wall cysts4Foon, R., H. Elbiss, and P.A. Moran, Cystoscopy for gynecologists. The Obstetrician & Gynaecologist, 2006. 8(2): p. 78-85.
- Evaluation of bladder involvement in cervical cancer
- Identification of diverticular openings
Healthcare providers also use cystoscopy as a treatment modality for:
- Injecting urethral bulking agents
- Hydrodistension
- Removal of bladder polyps, calculi, and tumors
- Injecting botox injection
- Treating urethral strictures5Tamilselvi, A., Role of Cystoscopy. Ambulatory Urology and Urogynaecology, 2021: p. 53-61.
Contraindications
Healthcare providers contraindicate the procedure if there is evidence of acute urinary infection. Acute urinary infections can put patients at risk of developing sepsis. Due to this reason, the provider recommends a urinalysis five to seven days before the scheduled cystoscopy. If the urinalysis confirms a UTI, they first focus on treating the infection appropriately. Urethral stricture can also make cystoscopy impossible. If the patient is intolerant to pain and feels discomfort during flexible cystoscopy, it requires a trip to the operating room for cystoscopy under anesthesia.6Engelsgjerd, J.S. and C.M. Deibert, Continuing Education Activity.
Types of Cystoscopes
The instrument used in cystoscopy (cystoscope) comes in two options.
Rigid Cystoscope
It comprises a telescope, bridge, obturator, and a metal sheath. The telescope includes a light source, and the operator selects different lens angles depending on the area needing visualization. The sheath has channels for irrigation fluid, usually normal saline or sterile water. The bridge may contain one or two working channels for inserting instruments. The size of these cystoscopes is measured in French units. For adults, the sheath diameter ranges from 17 to 24 French, while pediatric cystoscopes are typically 8 French in diameter. Rigid cystoscopes offer advantages such as a larger lumen for irrigation, wider working channels, easier orientation and handling, and superior optical clarity. In office settings, the procedure can be done under local anesthesia, though larger rigid scopes may require intravenous sedation or general anesthesia.7Engelsgjerd, J.S. and C.M. Deibert, Cystoscopy. 2018.
Flexible Cystoscope
A flexible cystoscope consists of a telescope, fiber optic bundles, and irrigated channel combined in a single unit. It is advantageous for visualizing all parts of the bladder and urethra due to its deflectable tip, which can move from 0 to 220 degrees. The diameter of a flexible cystoscope ranges from 15 to 18 French. It is better suited for office-based procedures but requires more extensive training compared to rigid cystoscopy.8Engelsgjerd, J.S. and C.M. Deibert, Cystoscopy. 2018.
Preparation before Cystoscopy
Before the procedure, the provider will obtain informed consent and may ask you:
- Are you currently taking any medications?
- When was your last meal? (You may be advised to avoid eating for at least eight hours before the procedure.)
- Have you emptied your bladder? (You will likely be asked to urinate before the procedure.)
A urine sample will be collected for urinalysis or urine culture. If a urinary tract infection is present, the procedure will be postponed. Prophylactic antibiotics may be recommended if the patient has any of the following risk factors:
- Advanced age
- Smoking history
- Poor nutritional status
- Poorly controlled diabetes
- Ongoing or recurrent infections
- Chronic corticosteroid use
- Presence of foreign bodies or anatomical abnormalities in the urinary tract9Engelsgjerd, J.S. and C.M. Deibert, Cystoscopy. 2018.
The healthcare provider will prepare the skin using an antiseptic, typically an aqueous iodophor (e.g., Betadine). Alcohol-based and chlorhexidine gluconate solutions can be damaging to the mucous membrane of the genitalia.10JS Jr, W., Urologic surgery antimicrobial prophylaxis best practice policy panel: best practice policy statement on urologic surgery antimicrobial prophylaxis. J. Urol., 2008. 179: p. 1379-1390.
After cleaning the skin with an anti-septic agent, the urologist injects lubricating gel into the urethra. The lubricating gel can be plain or lidocaine gel, which can help reduce the pain during the procedure.11Aaronson, D.S., et al., Meta‐analysis: does lidocaine gel before flexible cystoscopy provide pain relief? BJU international, 2009. 104(4): p. 506-510.
Procedure
The cystoscopy procedure follows these steps:
- You’ll lie on your back with knees bent and feet in stirrups.
- If required, you will receive local or general anesthesia.
- After numbing the urethra with lidocaine gel and waiting a few minutes, the doctor will gently insert the cystoscope. Doctors usually use smaller scopes unless surgical tools need to be passed into the bladder.
- The lens on the end of the cystoscope magnifies the inner surfaces of the bladder and urethra. A sterile fluid is used to fill and distend the bladder for better visualization.
- After the inspection, the fluid will be drained, or you’ll be asked to urinate.
- If required, your doctor will take tissue samples for testing and other procedures.
Results
The urologist may discuss initial findings immediately or during a follow-up visit. If your cystoscopy involves collecting a biopsy, you have to wait a few days for the results.
Recovery
Most people recover within one or two days from a cystoscopy. You might feel some abdominal discomfort, a burning sensation during urination, or the urge to urinate frequently. Applying a warm compress or taking a warm bath may help. Stay hydrated and take pain relievers if advised.
Side Effects or Complications of the Procedure
Usually, the complications of the cystoscopy are minor to moderate. They can include:
- Hematuria (Blood in urine)
- UTI
- Injury to the urethra or bladder
- Dysuria (Painful Urination)
Immediate complications like bleeding or urinary retention typically resolve within 24–48 hours.12Tamilselvi, A., Role of Cystoscopy. Ambulatory Urology and Urogynaecology, 2021: p. 53-61.
Cystoscopy as a Surgical Tool
Cystoscopy also plays a therapeutic role in various urological procedures:
- It assists in suprapubic catheter placement.
- It is used for hydrodistension in patients with interstitial cystitis.
- In cystolithotripsy, it helps fragment and remove bladder stones using lasers or lithotripters.
- Urethral bulking agents (e.g., Macroplastique, collagen) are injected under cystoscopic guidance to treat stress urinary incontinence.
- It is used to guide intradetrusor botulinum toxin injections for treating detrusor overactivity.13Tamilselvi, A., Role of Cystoscopy. Ambulatory Urology and Urogynaecology, 2021: p. 53-61.
However, drawbacks include equipment costs, patient discomfort, and the limited view confined to the bladder and urethral surfaces. Cystoscopy cannot evaluate adjacent extravesical structures.14Vining, D.J., et al., CT cystoscopy: an innovation in bladder imaging. American Journal of Roentgenology, 1996. 166: p. 409-410.
Cystoscopy vs. Cystogram
A comparative overview of cystoscopy and cystogram is given below:
| Cystoscopy | Cystogram |
| Cystoscopy involves the insertion of a flexible or rigid scope with a camera into the urethra and bladder. | Cystogram is an imaging technique that uses X-ray to visualize the inside of the bladder. Urologists insert a urinary catheter to fill the bladder with a contrast dye for clear imaging. |
Used to diagnose bladder problems such as:
|
Used to diagnose bladder problems such as:
|
| Invasive technique | Non-invasive as compared to cystoscopy. |
| Allow direct visualization of the internal surface and suspected areas of the bladder and urethra. | It does not provide direct visualization of the bladder lining. |
| It may cause discomfort to the patient and may require anesthesia. | Limit in detecting subtle abnormalities and small tumors. |
Cystoscopy vs. Ureteroscopy
While both cystoscopy and ureteroscopy are endoscopic procedures used to visualize the urinary tract, they differ significantly in their scope and purpose. Cystoscopy involves the insertion of a scope through the urethra to examine the bladder and is commonly used to evaluate conditions like bladder tumors, stones, infections, or structural abnormalities. In contrast, ureteroscopy is performed using a longer, narrower scope that extends beyond the bladder into the ureters and sometimes the renal pelvis, making it ideal for managing ureteral or kidney stones, strictures, or tumors in the upper urinary tract.15 Türk, C., Petřík, A., Sarica, K., Seitz, C., Skolarikos, A., Straub, M., & Knoll, T. (2016). EAU Guidelines on Interventional Treatment for Urolithiasis. European Urology, 69(3), 475–482. https://doi.org/10.1016/j.eururo.2015.07.041
Cystoscopy is generally less complex and is often done in an outpatient setting under local anesthesia. Ureteroscopy, however, typically requires general or regional anesthesia due to the deeper navigation and potential for stone removal or laser fragmentation. Though both procedures are minimally invasive, they serve distinct roles depending on the location and nature of the urologic issue.
Final Review
Cystoscopy is an important diagnostic tool. This procedure is relatively simple and is often performed in an office setting. Providing a valuable diagnostic tool, it helps identify various conditions. Additionally, it plays a crucial role in assessing ureteral or bladder integrity during surgery. The two most immediate complications of this process are urinary obstructions and bleeding. Abnormal results from the cystoscopy may include impairments of the urethra, bladder stones, or bladder cancer. However, only highly trained urologists and gynecologists can perform the procedure precisely. Additionally, interprofessional teamwork will result in the best care of the patient and the best outcomes.
Refrences
- 1Matulewicz, R.S., J.O. DeLancey, and J.J. Meeks, Cystoscopy. JAMA, 2017. 317(11): p. 1187-1187.
- 2Acar, Ö. and T. Tarcan, Cystoscopic evaluation and clinical phenotyping in interstitial cystitis/bladder pain syndrome. Journal of the Turkish German Gynecological Association, 2019. 20(2): p. 117.
- 3Tamilselvi, A., Role of Cystoscopy. Ambulatory Urology and Urogynaecology, 2021: p. 53-61.
- 4Foon, R., H. Elbiss, and P.A. Moran, Cystoscopy for gynecologists. The Obstetrician & Gynaecologist, 2006. 8(2): p. 78-85.
- 5Tamilselvi, A., Role of Cystoscopy. Ambulatory Urology and Urogynaecology, 2021: p. 53-61.
- 6Engelsgjerd, J.S. and C.M. Deibert, Continuing Education Activity.
- 7Engelsgjerd, J.S. and C.M. Deibert, Cystoscopy. 2018.
- 8Engelsgjerd, J.S. and C.M. Deibert, Cystoscopy. 2018.
- 9Engelsgjerd, J.S. and C.M. Deibert, Cystoscopy. 2018.
- 10JS Jr, W., Urologic surgery antimicrobial prophylaxis best practice policy panel: best practice policy statement on urologic surgery antimicrobial prophylaxis. J. Urol., 2008. 179: p. 1379-1390.
- 11Aaronson, D.S., et al., Meta‐analysis: does lidocaine gel before flexible cystoscopy provide pain relief? BJU international, 2009. 104(4): p. 506-510.
- 12Tamilselvi, A., Role of Cystoscopy. Ambulatory Urology and Urogynaecology, 2021: p. 53-61.
- 13Tamilselvi, A., Role of Cystoscopy. Ambulatory Urology and Urogynaecology, 2021: p. 53-61.
- 14Vining, D.J., et al., CT cystoscopy: an innovation in bladder imaging. American Journal of Roentgenology, 1996. 166: p. 409-410.
- 15Türk, C., Petřík, A., Sarica, K., Seitz, C., Skolarikos, A., Straub, M., & Knoll, T. (2016). EAU Guidelines on Interventional Treatment for Urolithiasis. European Urology, 69(3), 475–482. https://doi.org/10.1016/j.eururo.2015.07.041

