An Embolic Stroke occurs when a clot, such as a blood clot or another particle like plaque, obstructs an artery in the brain, disrupting the supply of oxygen to that area. Typically, this type of stroke is caused by a blood clot that originates in another part of the body and subsequently travels to the brain via the bloodstream.
Stroke is a major public health concern. It is the most common cause of long-term disability (morbidity) and ranks as the fifth leading cause of death (mortality) in the United States.1Virani SS, Alonso A, Benjamin EJ, Bittencourt MS, Callaway CW, Carson AP, Chamberlain AM, Chang AR, Cheng S, Delling FN, Djousse L, Elkind MSV, Ferguson JF, Fornage M, Khan SS, Kissela BM, Knutson KL, Kwan TW, Lackland DT, Lewis TT, Lichtman JH, Longenecker CT, Loop MS, Lutsey PL, Martin SS, Matsushita K, Moran AE, Mussolino ME, Perak AM, Rosamond WD, Roth GA, Sampson UKA, Satou GM, Schroeder EB, Shah SH, Shay CM, Spartano NL, Stokes A, Tirschwell DL, VanWagner LB, Tsao CW., American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee. Heart Disease and Stroke Statistics-2020 Update: A Report From the American Heart Association. Circulation. 2020 Mar 03;141(9):e139-e596 It is a frightening event for those affected and their loved ones. Having a proper understanding of a stroke can help save someone’s life in your surroundings.
What is an Embolic Stroke?
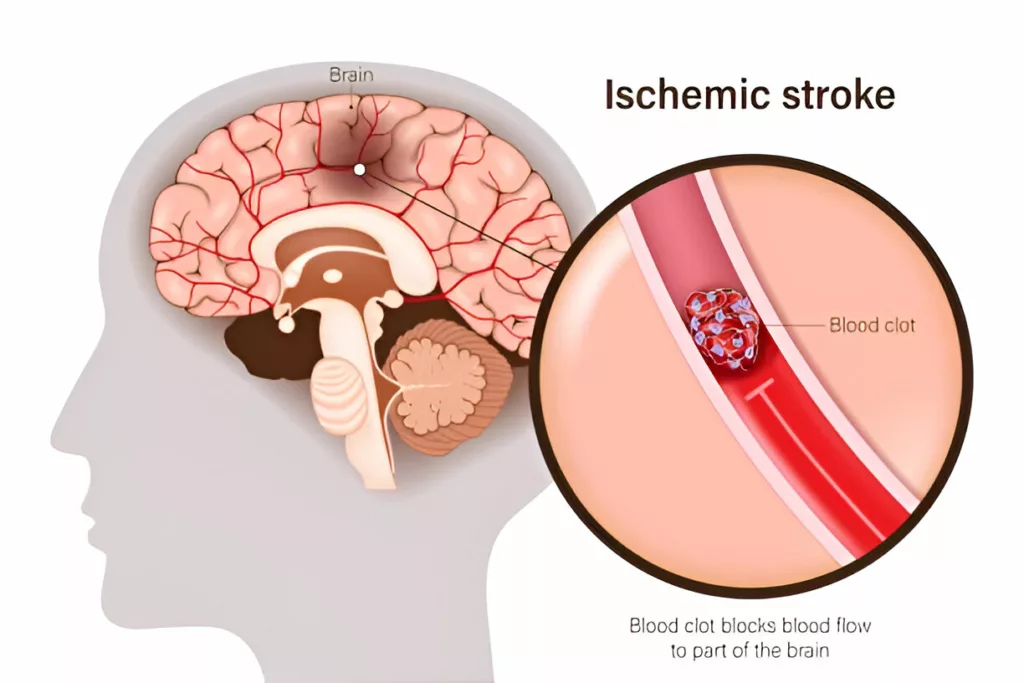
A stroke is a medical emergency that occurs when blood flow to a part of the brain is reduced or blocked, depriving brain cells of oxygen and nutrients. As a result, the affected area of the brain begins to die within minutes, leading to sudden and often serious symptoms. Stroke can be broadly categorized into two main types: ischemic (due to blockage) and hemorrhagic (due to bleeding). The majority of strokes are ischemic.
An embolic stroke is a subtype of ischemic stroke that occurs when the blood supply to the brain is interrupted. It is characterized by hypoxia (decreased oxygen supply), ultimately leading to ischemia and serving as a precursor to tissue damage.
An embolic stroke occurs when a thrombus dislodges from its site of origin, such as an atherosclerotic plaque, and travels through the bloodstream. Once dislodged, it is referred to as an embolus. This embolus can get stuck in the smaller and distal tributaries of blood vessels supplying the brain. In most cases, the embolus is a blood clot. However, in rare cases, it may consist of non-thrombotic material such as air, fat, foreign bodies, tumor fragments, or even amniotic fluid.2Hart RG, Diener HC, Coutts SB, Easton JD, Granger CB, O’Donnell MJ, Sacco RL, Connolly SJ. Embolic strokes of undetermined source: the case for a new clinical construct. The Lancet Neurology. 2014 Apr 1;13(4):429-38.
Causes of an Emboli Formation
An embolus can develop due to a litany of reasons, including:
Blood Stasis:
Blood stasis occurs when blood flow becomes sluggish or stagnant, often in the setting of atrial fibrillation, prolonged immobility, or heart failure. This lack of circulation encourages clot formation, especially in the left atrial appendage during atrial fibrillation. Contributing factors may include diabetes, high cholesterol, hypertension, smoking, and excessive alcohol consumption.
Calcific Degeneration of Valves:
Degeneration of the heart valves—most often due to age—can lead to the narrowing or thickening of valve tissue (stenosis). This disturbed flow creates turbulence, fostering clot formation. Rheumatic heart disease and aortic valve sclerosis are classic examples.
Abnormally Enlarged Left Heart:
Conditions like dilated cardiomyopathy or longstanding hypertension can enlarge the left side of the heart, particularly the left atrium and ventricle. This enlargement may impair normal heart rhythm and contractility, leading to blood pooling and thrombus formation.3Weir NU. An update on cardioembolic stroke. Postgrad Med J 2008;84:133–42; quiz 139–40. https://doi.org/10.1136/pgmj.2007.066563.
In rare cases, a clot from the venous system (such as in Deep Vein Thrombosis) can bypass the lungs and reach the arterial system through a patent foramen ovale (PFO) or atrial septal defect (paradoxical embolism). This allows a clot to directly travel to the brain and cause an embolic stroke.4Weir NU. An update on cardioembolic stroke. Postgrad Med J. 2008 Mar;84(989):133-42; quiz 139-40
Atrial Fibrillation:
AF is the most common identifiable cause of embolic stroke. It leads to irregular, ineffective atrial contractions that allow blood to stagnate and clot, especially in the left atrial appendage. The risk of stroke from AF increases significantly with age.5Ferro JM. Brain embolism – Answers to practical questions. J Neurol. 2003 Feb;250(2):139-47.
Risk Factors for Embolic Stroke
Risk factors of an embolic stroke can be divided into two subgroups: modifiable and non-modifiable risk factors. Modifiable risk factors include:
- High cholesterol
- Hypertension (high blood pressure)
- Smoking
- Obesity
- Sedentary lifestyle
On the other hand, non-modifiable risk factors include:
- Recent childbirth
- People with a family history of stroke
- Age over 40
- Heart diseases
- Structural heart defects (e.g., PFO, atrial septal aneurysm)
Types of Embolic Stroke
Embolic strokes can be classified based on the source of the embolus, and understanding these categories is critical for diagnosis, treatment, and prevention.6Ay H, Furie KL, Singhal A, Smith WS, Sorensen AG, Koroshetz WJ. An evidence-based causative classification system for acute ischemic stroke. Ann Neurol. 2005 Nov;58(5):688-97. doi: 10.1002/ana.20617. PMID: 16240340.
Cardioembolic Stroke (Known Cardiac Source):
These strokes originate from clots formed within the heart, often due to atrial fibrillation, heart valve disease, recent myocardial infarction, or the presence of cardiac tumors like atrial myxoma. This type is usually associated with sudden onset and may affect multiple brain territories.7 Stroke: Etiology, classification, and epidemiology. Available at: https://www.uptodate.com/contents/stroke-etiology-classification-and-epidemiology?search=embolic%20stroke&source=search_result&selectedTitle=5~150&usage_type=default&display_rank=5. Accessed March 21, 2025.
High-risk cardiac sources include:
- Atrial fibrillation (paroxysmal or sustained)
- Mechanical or bioprosthetic heart valves
- Rheumatic mitral or aortic valve disease
- Recent or chronic myocardial infarction
- Dilated cardiomyopathy etc.
Possible Cardiac or Aortic Source:
In some cases, a potential embolic source is detected via imaging—especially echocardiography—but the direct link to the stroke is uncertain. These are considered potential cardiac sources because they may not always produce emboli.
Examples include:
- Patent foramen ovale (PFO)
- Atrial septal aneurysm (with or without PFO)
- Complex atheroma in the ascending aorta or aortic arch
Arterial Source (Artery-to-Artery Embolism):
This occurs when a thrombus forms in a large artery (such as the carotid or vertebral artery) and travels downstream, lodging in a smaller artery in the brain. It’s common in patients with atherosclerosis and can mimic other types of stroke.
Embolic Stroke of Undetermined Source (ESUS):
In some cases, extensive testing fails to identify a clear cause. These are termed cryptogenic or “of undetermined source.” ESUS accounts for a significant portion of embolic strokes, and ongoing research aims to clarify hidden sources like intermittent atrial fibrillation or silent aortic plaque.8Hart RG, Diener HC, Coutts SB, Easton JD, Granger CB, O’Donnell MJ, Sacco RL, Connolly SJ; Cryptogenic Stroke/ESUS International Working Group. Embolic strokes of undetermined source: the case for a new clinical construct. Lancet Neurol. 2014;13:429–438. doi: 10.1016/S1474-4422(13)70310-7.
How Does a Stroke Present Itself?
Symptoms and presentation of an embolic are very similar to other types of ischemic stroke, which can generally include:
- Numbness or weakness on one side of the body
- Difficulty speaking words or slurred speech
- Dizziness
- Temporary paralysis
- Loss of muscle coordination
- Altered level of consciousness (ALOC)
- Nausea
- Difficulty swallowing
- Decreased vision
- Diplopia (double vision)9Learn More Stroke Warning Signs and Symptoms. WwwStrokeOrg n.d. https://www.stroke.org/en/about-stroke/stroke-symptoms/learn-more-stroke-warning-signs-and-symptoms (accessed June 16, 2023).
Recognizing the signs and symptoms of an embolic stroke can be crucial when someone is experiencing a stroke in your presence. It is important to pay attention to three key aspects: facial symptoms, arm function, and speech. A mnemonic FAST can be helpful when remembering the symptoms.
F – Face: Observe if the person has a drooping smile or if one side of their face appears uneven or droopy. Facial asymmetry can be a sign of a stroke and should be taken seriously
A – Arms: Ask the person to lift both arms simultaneously. If they are unable to raise one arm or if one arm drifts downward compared to the other, it could indicate a potential stroke.
S – Speech: Assess their speech by asking them to repeat a simple sentence. Slurred speech, difficulty finding words, or incoherent speech patterns may be indicative of a stroke.
T – Time/Treatment: Time to call emergency services immediately. If you observe any of the above mentioned signs, it is important to act promptly.
How To Diagnose an Embolic Stroke?
There are various steps to a diagnosis of an embolic stroke. However, a physical exam and neuroimaging are crucial for accurate diagnosis. In addition to that, the best and the earliest diagnostic modalities for an embolic stroke are CT and MRIs. The early diagnosis of a stroke is crucial as it can lead to prompt treatment and prevent permanent brain damage.
CT Scan:
A non-contrast CT scan is usually the first imaging test performed in suspected stroke cases. It uses strong X-rays to better visualize the blood vessels, bones, and brain matter. It can help detect any bleeding, which is crucial in differentiating between an ischemic stroke and a hemorrhagic stroke.
In the early stages of an ischemic stroke such as an embolic stroke, a CT may appear normal, but subtle signs may still suggest infarction. CT is crucial because administering thrombolytic therapy (such as tPA) is only appropriate once bleeding is ruled out.
MRI:
An MRI, particularly diffusion-weighted imaging (DWI), is more sensitive than a CT scan in detecting early ischemic changes. It can locate smaller infarcts and is better at identifying the exact brain area affected by the embolus. However, MRIs are not always as readily available as CT scans, especially in emergency settings.10Wessels T, Wessels C, Ellsiepen A, et al. Contribution of diffusion-weighted imaging in the determination of stroke etiology. AJNR Am J Neuroradiol. 2006;27:35–9.
CT Angiogram:
It is the same as a CT scan. However, a CT angiogram involves injecting a dye that helps detect any obstruction in the blood supply of the brain, which might be the potential cause of an embolic stroke. It may take up to 48 hours for a CT-Scan to diagnose an ischemic stroke whereas a hemorrhagic stroke can be located immediately, as it presents with a fresh bleed.
Echocardiogram:
An echocardiogram, particularly a transesophageal echocardiogram (TEE), uses ultrasound to visualize the heart and can help identify embolic sources such as cardiac thrombi, valvular vegetations, or patent foramen ovale (PFO). Identifying the source of the embolus is critical for secondary prevention.
Additional Workup
Once a stroke has been confirmed, various labs are run to confirm the cause and risk factors for the stroke; these labs can include:
- Blood tests, including a complete blood count (CBC), electrolytes, glucose levels, and renal function.
- Coagulation studies such as PT/INR, aPTT, and fibrinogen levels, help assess for hypercoagulability or bleeding disorders.
- Cardiac monitoring, including ECG and continuous telemetry, may reveal arrhythmias like atrial fibrillation, a common source of emboli.
- In younger patients or those with no obvious source, tests for hypercoagulable states may be done, including protein C and S levels, antiphospholipid antibodies, and genetic mutations like Factor V Leiden.11Hooda, A., Khandelwal, P. D., & Saxena, P. (2009). Protein S deficiency: Recurrent ischemic stroke in young. Annals of Indian Academy of Neurology, 12(3), 183. https://doi.org/10.4103/0972-2327.56319
How is it Treated?
The treatment of embolic stroke depends on the time passed since the stroke has occurred; the sooner the treatment, the better the outcome. One of the most common approaches is breaking up the clot, which is mainly performed by using an intravenous Tissue Plasminogen Activator (tPA). However, according to the 2018 treatment guidelines of the American Heart Association (AHA) for embolic stroke, this treatment option can only be used within 4.5 hours after the stroke.12Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al. 2018 Guidelines for the Early Management of Patients With Acute Ischemic Stroke: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke 2018;49. https://doi.org/10.1161/STR.0000000000000158.
Mechanical thrombectomy is another treatment option and is used if the stroke is caused by a large vessel occlusion. This minimally invasive procedure involves threading a catheter into the blocked artery to physically retrieve the clot. Thrombectomy is most effective within 6 hours of stroke onset, though select patients may benefit up to 24 hours after onset based on advanced imaging criteria.
After emergency management, patients are usually prescribed secondary prevention medications, which aim to prevent future strokes. These often include:
- Antiplatelet agents such as aspirin or clopidogrel
- Anticoagulants like warfarin, or dabigatran, especially if atrial fibrillation or another high-risk cardiac source is present
- Statins to control cholesterol levels
- Antihypertensives to control blood pressure
How Can You Prevent an Embolic Stroke?
Prevention is always better than cure. Unfortunately, factors such as family history and previous MI are not manageable. However, you can always pay attention to modifiable factors such as cholesterol, body weight, activity, etc. Here is how you can decrease the risk of an embolic stroke:
- Adapt a healthy lifestyle
- Include fruits and vegetables in your diet
- Reduce your cholesterol
- Control your alcohol intake
Conclusion
As explained above, an embolic stroke leads to severe physical and cognitive disability however, this impairment can be minimized with timely management and treatment. Furthermore, it is always best to avoid causative risk factors such as high cholesterol, lack of exercise, smoking, etc.
Refrences
- 1Virani SS, Alonso A, Benjamin EJ, Bittencourt MS, Callaway CW, Carson AP, Chamberlain AM, Chang AR, Cheng S, Delling FN, Djousse L, Elkind MSV, Ferguson JF, Fornage M, Khan SS, Kissela BM, Knutson KL, Kwan TW, Lackland DT, Lewis TT, Lichtman JH, Longenecker CT, Loop MS, Lutsey PL, Martin SS, Matsushita K, Moran AE, Mussolino ME, Perak AM, Rosamond WD, Roth GA, Sampson UKA, Satou GM, Schroeder EB, Shah SH, Shay CM, Spartano NL, Stokes A, Tirschwell DL, VanWagner LB, Tsao CW., American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee. Heart Disease and Stroke Statistics-2020 Update: A Report From the American Heart Association. Circulation. 2020 Mar 03;141(9):e139-e596
- 2Hart RG, Diener HC, Coutts SB, Easton JD, Granger CB, O’Donnell MJ, Sacco RL, Connolly SJ. Embolic strokes of undetermined source: the case for a new clinical construct. The Lancet Neurology. 2014 Apr 1;13(4):429-38.
- 3Weir NU. An update on cardioembolic stroke. Postgrad Med J 2008;84:133–42; quiz 139–40. https://doi.org/10.1136/pgmj.2007.066563.
- 4Weir NU. An update on cardioembolic stroke. Postgrad Med J. 2008 Mar;84(989):133-42; quiz 139-40
- 5Ferro JM. Brain embolism – Answers to practical questions. J Neurol. 2003 Feb;250(2):139-47.
- 6Ay H, Furie KL, Singhal A, Smith WS, Sorensen AG, Koroshetz WJ. An evidence-based causative classification system for acute ischemic stroke. Ann Neurol. 2005 Nov;58(5):688-97. doi: 10.1002/ana.20617. PMID: 16240340.
- 7Stroke: Etiology, classification, and epidemiology. Available at: https://www.uptodate.com/contents/stroke-etiology-classification-and-epidemiology?search=embolic%20stroke&source=search_result&selectedTitle=5~150&usage_type=default&display_rank=5. Accessed March 21, 2025.
- 8Hart RG, Diener HC, Coutts SB, Easton JD, Granger CB, O’Donnell MJ, Sacco RL, Connolly SJ; Cryptogenic Stroke/ESUS International Working Group. Embolic strokes of undetermined source: the case for a new clinical construct. Lancet Neurol. 2014;13:429–438. doi: 10.1016/S1474-4422(13)70310-7.
- 9Learn More Stroke Warning Signs and Symptoms. WwwStrokeOrg n.d. https://www.stroke.org/en/about-stroke/stroke-symptoms/learn-more-stroke-warning-signs-and-symptoms (accessed June 16, 2023).
- 10Wessels T, Wessels C, Ellsiepen A, et al. Contribution of diffusion-weighted imaging in the determination of stroke etiology. AJNR Am J Neuroradiol. 2006;27:35–9.
- 11Hooda, A., Khandelwal, P. D., & Saxena, P. (2009). Protein S deficiency: Recurrent ischemic stroke in young. Annals of Indian Academy of Neurology, 12(3), 183. https://doi.org/10.4103/0972-2327.56319
- 12Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al. 2018 Guidelines for the Early Management of Patients With Acute Ischemic Stroke: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke 2018;49. https://doi.org/10.1161/STR.0000000000000158.

