Keratoconus is an eye disorder it occurs when your cornea, a clear and transparent layer of eye, changes its shape from dome to cone shape. This leads to double vision and distorted vision making it difficult to see the things clearly. The cause of the keratoconus is still unclear. However, it often starts in the teenage years or early adulthood.
Early detection of keratoconus is important for treatment and preventing its progression. The primary diagnostic tools for detecting keratoconus include corneal topography and tomography. It is easy to prevent the disease’s progression once it is diagnosed. The condition can be corrected with glasses, contact lens and cross collagen linking sometimes corneal transplant is required.
What is Keratoconus?
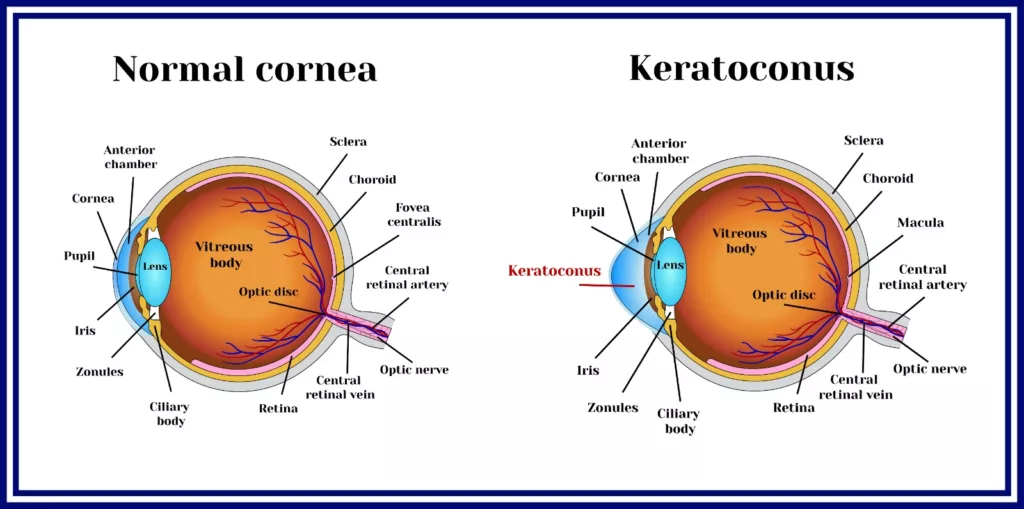
Keratoconus is a bilateral progressive corneal disease in which the cornea gradually thins and bulges outward, causing changes in its curvature that lead to a reduction in the quality of vision. Keratoconus often affects both eyes, though one eye may be more affected than the other. The condition generally starts in the teenage years and advances until the mid-thirties, but it can occur at any age. Keratoconus may continue to develop slowly over the course of ten years or more. It occurs in around 50-230 per 100,000 individuals and equally affects both genders.1Asimellis G, Kaufman EJ. Keratoconus. [Updated 2024 Apr 12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470435/
Eye Cornea & Its Function:
A cornea is a clear and transparent layer at the front of the eye that allows light to enter and reach the lens. The primary function of the cornea is to refract and bend the light that enters it. It has a dome-shaped structure made of small protein fibers called collagen. These collagens help the cornea hold the structure; when these fibers weaken, the cornea goes from a normal round to a dome shape. This happens when there is a lack of protective antioxidants, which help get rid of the harmful byproducts and protect the collagen. The collagen fibers weaken if there is a low level of protective antioxidants. As a result, the cornea thins and bulges outward.
Causes of Keratoconus
Both genetic and environmental factors contribute to its development. However, the exact cause of keratoconus is still unknown.2Davidson, A., Hayes, S., Hardcastle, A., et al. The pathogenesis of keratoconus. Eye 28, 189–195 (2014). https://doi.org/10.1038/eye.2013.278
Frequent eye injuries and eye rubbing can initiate the condition, particularly in genetically predisposed individuals. Additionally, thinning of the cornea contributes to both keratoconus and its progression. Several systemic conditions, including Down syndrome and Ehlers-Danlos syndrome, are also associated with keratoconus.
Symptoms
Keratoconus usually gets worse over time. The symptoms change as the condition advances. Some common signs of keratoconus are:
- Double vision: You may see overlapping or double images.
- Blurred vision: As the cornea changes shape, light doesn’t focus correctly, causing blurry vision.
- Distorted vision: Objects may look wavy or uneven due to the cornea’s irregular shape.
- Increased light sensitivity: Bright lights can feel uncomfortable or too intense.
- Reduced vision clarity: Over time, your ability to see clearly decreases.
- Glare: You may become more sensitive to glare, especially at night.
How Keratoconus Affects Your Vision
There are two ways keratoconus affects your vision in;
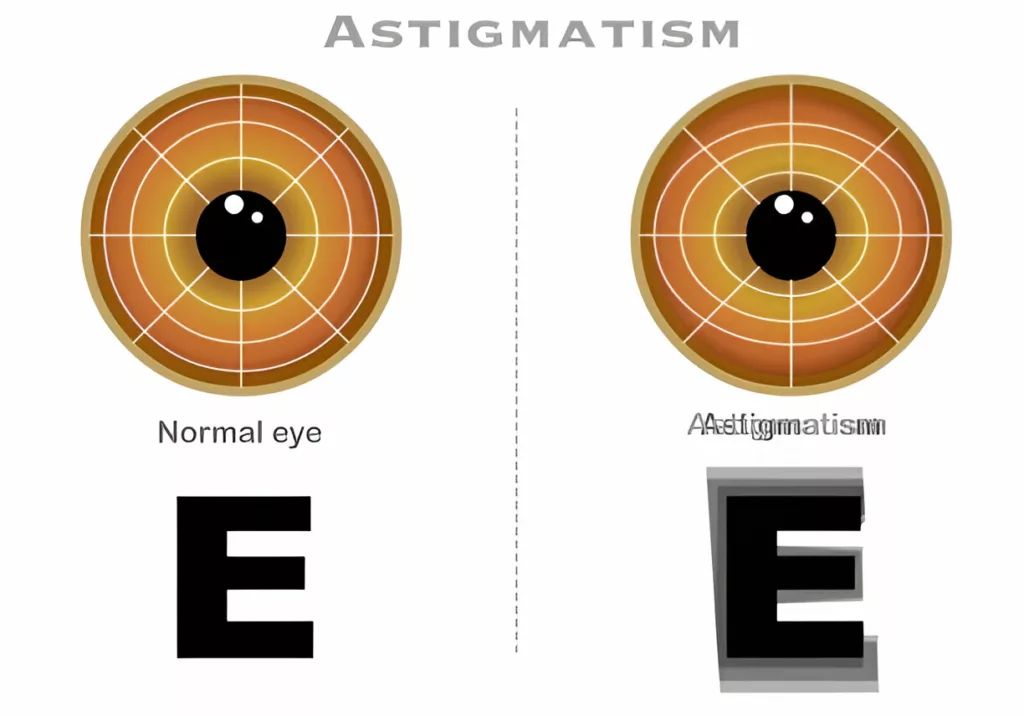
- The cornea changes its shape from dome to cone, making its smooth surface wavy and causing irregular astigmatism. Keratoconus and astigmatism are closely related yet distinct conditions that impact vision differently. Astigmatism is a common refractive error, not a disease, and occurs when the cornea or lens has an irregular shape. This irregularity causes light to bend unevenly, resulting in blurred or distorted vision at any distance. In most cases, astigmatism is symmetrical and easily correctable with glasses, contact lenses, or laser surgery.On the other hand, keratoconus is an eye disease that causes the cornea to thin and bulge into a cone shape. This distortion leads to irregular astigmatism, where light bends in asymmetrical and inconsistent ways, often smearing vision in multiple directions.
- As the cornea bulges out, it causes shortsightedness (myopia), which means you can see close objects clearly, but distant objects appear wavy and blurry.3Ernst BJ, Hsu HY. Keratoconus association with axial myopia: a prospective biometric study. Eye Contact Lens. 2011 Jan;37(1):2-5. doi: 10.1097/ICL.0b013e3181fb2119. PMID: 21178694.
Risk Factors of keratoconus
Some of the risk factors that may contribute to development of keratoconus are;
Family History:
Keratoconus often runs in families. If your family has a history of keratoconus, you may be at risk of developing this condition. It’s important to check your children’s eyes for signs of keratoconus, as it often begins during the teenage years.4Hashemi, Hassan MD*; Heydarian, Samira PhD†; Hooshmand, Elham MSc‡; Saatchi, Mohammad PhD§; Yekta, Abbasali PhD¶; Aghamirsalim, Mohamadreza MD‖; Valadkhan, Mehrnaz M.Sc*; Mortazavi, Mehdi MD**; Hashemi, Alireza MD††; Khabazkhoob, Mehdi PhD‡‡. The Prevalence and Risk Factors for Keratoconus: A Systematic Review and Meta-Analysis. Cornea 39(2):p 263-270, February 2020. | DOI: 10.1097/ICO.0000000000002150
Age:
Keratoconus usually begins in the early years, usually in the 20s and 30s; it can also occur in the 40s, which is less common.
Systemic Conditions:
Several systemic conditions may be associated with keratoconus. These conditions include Down syndrome, Ehlers-Danlos syndrome, and osteogenesis imperfecta.
Eye Rubbing:
Frequent eye rubbing can damage the cornea and worsen the condition, especially if there’s a family history of keratoconus.5Bettahar, T., Rahmoune, C., & Benazzouz, D. (2020). Keratoconus prognosis study for patients with corneal external mechanical stress mode. International ophthalmology, 40(7), 1673–1686. https://doi.org/10.1007/s10792-020-01335-2
Environmental Factor:
Studies showed keratoconus’s association with environmental factors like asthma, hay fever, and atopic dermatitis.
Diagnosis of keratoconus
Your opthalmologist will review your medical history and perform a detailed eye exam to detect keratoconus. In addition to the exam, they may perform specific tests like corneal topography and corneal tomography, slit lamp test, and pachymetry for further evaluation of the cornea and irregularities.
Corneal Topography:
Corneal topography is the best tool for detecting keratoconus. The test checks the front surface of the cornea closely for irregularities or problems. It is also helpful in planning eye surgeries and assessing astigmatism.
Corneal Tomography:
This test provides a comprehensive view of both the front and back surfaces of the cornea and measures its thickness. It helps detect keratoconus early, allowing for timely treatment, such as collagen cross-linking, to slow the keratoconus progression and avoid more invasive procedures later.6 Bui, A. D., Truong, A., Pasricha, N. D., & Indaram, M. (2023). Keratoconus Diagnosis and Treatment: Recent Advances and Future Directions. Clinical Ophthalmology, 17, 2705–2718. https://doi.org/10.2147/OPTH.S392665
Both corneal tomography and topography are crucial for the early detection of keratoconus in suspected cases. They are also effective for monitoring the progression of the condition and guiding suitable treatment options.7Stephen D. Klyce, Tetsuro Oshika, Chapter 9 – Corneal structure and function: Placido-based corneal topography, Editor(s): Frederick S. Brightbill, Peter J. McDonnell, Ayad A. Farjo, Charles N.J. McGhee, Olivia N. Serdarevic, Cook Lhowe Laurel, Corneal Surgery (Fourth Edition), Mosby, 2009, Pages 75-82, ISBN 9780323048354, https://doi.org/10.1016/B978-0-323-04835-4.50015-X. (https://www.sciencedirect.com/science/article/pii/B978032304835450015X)
Slit Lamp Test:
The slit lamp test evaluates the outer and middle layers of the cornea. However, in the initial stages of keratoconus, results often appear normal, making it less effective for early detection of the condition.
Pachymetry:
Pachymetry examines the curvature and thickness of the cornea with a corneal pachymeter. An uneven or raised posterior corneal surface can suggest the presence of keratoconus.
Stages of keratoconus
Keratoconus develops in three main stages, each with different symptoms and complications. Each person’s time to move from one stage to the next varies. Treatment depends on the stage and how quickly the condition progresses. Knowing these stages helps manage keratoconus, prevent it from worsening, and effectively treat vision problems.
Early Keratoconus:
In the early stages, when corneal changes are minimal, eyeglasses are commonly prescribed to resolve vision. The symptoms at the early stage are often mild and the condition remains unnoticed, as the symptoms like blurry vision, vision distortion, increased sensitivity to light and eye irritation can mimic other eye problems.
Many people find their prescription changes frequently because at this stage, the cornea begins to deform, which causes frequent changes in the prescription of glasses. Diagnostic tools such as corneal topography can correctly diagnose keratoconus in the early stage.
Moderate Keratoconus:
At this stage, the changes in the cornea become prominent as the cornea continues to thin and bulge out. This results in increased vision distortion, double vision, and blurry vision. Daily activities like driving, reading, and face identification become compromised.
An effective approach to treatment is essential to correcting vision problems. This includes rigid gas-permeable contact lenses that help reshape the cornea and encourage tear healing. Another special procedure called collagen cross-link is also effective, as it enhances collagen fibers in the cornea and strengthens its structure.
Advanced Keratoconus:
In the advanced stage of keratoconus, the cornea becomes very thin and bulges outward. There may also be scarring on the cornea. The symptoms are severe, including severe distortion of vision, blurring, double vision, and sensitivity to light.
The advanced stage may present complications like hydrops, which cause sudden and painful corneal pain that needs immediate attention. The treatment for this stage is scleral contact lenses, which improve vision. Another treatment option for this stage is a corneal transplant, where the damaged cornea is replaced with a healthy cornea from a donor.
How Is Keratoconus Treated?
The treatment for keratoconus varies based on the severity of symptoms. In the early stages, mild symptoms can often be managed with eyeglasses to improve vision. As the condition progresses, specially designed hard contact lenses may be needed to maintain clear focus.
Surgical Interventions for Keratoconus:
If the condition doesn’t improve by previous intervention, the doctor may opt for surgical correction.
Collagen Cross-Linking
Collagen cross-linking is a medical treatment used to strengthen the cornea in individuals with keratoconus. The process strengthens the weaker bonds in the cornea, stabilizing the corneal structure. The method uses riboflavin, which is a vitamin B2 with ultraviolet A light. A small portion of the cornea surface is removed, and riboflavin is applied to it. After this, ultraviolet light activates the riboflavin, which will help make new bonds in the cornea and stabilize the structure. This effective process helps stop the keratoconus progression in early phases, though it does not reverse the condition. It can significantly improve vision and prevent the need for corneal transplants in advanced cases. The procedure is suitable for both children and adults. However, contact lenses may still be required after the procedure for optimal vision.8Sykakis, E., Karim, R., Evans, J. R., Bunce, C., Amissah-Arthur, K. N., Patwary, S., McDonnell, P. J., & Hamada, S. (2015). Corneal collagen cross-linking for treating keratoconus. The Cochrane database of systematic reviews, 2015(3), CD010621. https://doi.org/10.1002/14651858.CD010621.pub2
Corneal Transplant
A corneal transplant (keratoplasty) may be suggested if contact lenses are no longer effective. This procedure replaces the damaged cornea with donor tissue. Corneal transplants have a high success rate, but there is a risk of tissue rejection. This risk can be managed with corticosteroid medications.
Aftercare for Surgical Methods
You can expect the following after surgical correction:
- Your doctor will prescribe medications to prevent infection, reduce pain, and control inflammation
- Contact lenses or glasses are often suggested to fix refractive errors after surgery
- Don’t rub your eyes to avoid irritation
- Avoid heavy lifting and activities that put pressure on your eyes
- Regular check-ups with your eye doctor are important to monitor healing and deal with any problems
Prognosis
The prognosis depends on age. People of younger ages experience quick progression of the condition. Early detection and treatment of the keratoconus can greatly lower the chance of worsening the condition.
Complications
Keratoconus condition and its treatment may bring some complications, including;
- Pain and swelling in the cornea
- Scarring in the cornea
- Visual disturbances, including increased sensitivity to light and blurred vision
- Risk of getting infection after surgery
- Anxiety and depression due to visual problems
Takeaway
Keratoconus is an eye condition characterized by the bulging of the cornea from a normal round shape, which results in astigmatism, double vision, blurry vision, and short-sightedness. Early diagnosis of the condition is essential for an effective treatment, improving vision and preventing its progression. The best diagnostic tool to detect this eye condition is corneal topography, and the best treatment protocol is collagen cross-linking, which strengthens the cornea structure. Moreover, avoiding frequent eye rubbing can help prevent the development of keratoconus. Regular eye check-ups are important if keratoconus runs in your family.
Refrences
- 1Asimellis G, Kaufman EJ. Keratoconus. [Updated 2024 Apr 12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470435/
- 2Davidson, A., Hayes, S., Hardcastle, A., et al. The pathogenesis of keratoconus. Eye 28, 189–195 (2014). https://doi.org/10.1038/eye.2013.278
- 3Ernst BJ, Hsu HY. Keratoconus association with axial myopia: a prospective biometric study. Eye Contact Lens. 2011 Jan;37(1):2-5. doi: 10.1097/ICL.0b013e3181fb2119. PMID: 21178694.
- 4Hashemi, Hassan MD*; Heydarian, Samira PhD†; Hooshmand, Elham MSc‡; Saatchi, Mohammad PhD§; Yekta, Abbasali PhD¶; Aghamirsalim, Mohamadreza MD‖; Valadkhan, Mehrnaz M.Sc*; Mortazavi, Mehdi MD**; Hashemi, Alireza MD††; Khabazkhoob, Mehdi PhD‡‡. The Prevalence and Risk Factors for Keratoconus: A Systematic Review and Meta-Analysis. Cornea 39(2):p 263-270, February 2020. | DOI: 10.1097/ICO.0000000000002150
- 5Bettahar, T., Rahmoune, C., & Benazzouz, D. (2020). Keratoconus prognosis study for patients with corneal external mechanical stress mode. International ophthalmology, 40(7), 1673–1686. https://doi.org/10.1007/s10792-020-01335-2
- 6Bui, A. D., Truong, A., Pasricha, N. D., & Indaram, M. (2023). Keratoconus Diagnosis and Treatment: Recent Advances and Future Directions. Clinical Ophthalmology, 17, 2705–2718. https://doi.org/10.2147/OPTH.S392665
- 7Stephen D. Klyce, Tetsuro Oshika, Chapter 9 – Corneal structure and function: Placido-based corneal topography, Editor(s): Frederick S. Brightbill, Peter J. McDonnell, Ayad A. Farjo, Charles N.J. McGhee, Olivia N. Serdarevic, Cook Lhowe Laurel, Corneal Surgery (Fourth Edition), Mosby, 2009, Pages 75-82, ISBN 9780323048354, https://doi.org/10.1016/B978-0-323-04835-4.50015-X. (https://www.sciencedirect.com/science/article/pii/B978032304835450015X)
- 8Sykakis, E., Karim, R., Evans, J. R., Bunce, C., Amissah-Arthur, K. N., Patwary, S., McDonnell, P. J., & Hamada, S. (2015). Corneal collagen cross-linking for treating keratoconus. The Cochrane database of systematic reviews, 2015(3), CD010621. https://doi.org/10.1002/14651858.CD010621.pub2

