Myelography is a medical procedure used to examine parts of the central nervous system within the vertebral canal. It is an important radiologic modality for diagnosing disorders of the spinal cord.
What is Myelography?
Myelography is a radiological investigation of the vertebral canal. It usually employs two types of modalities— fluoroscopy and radiologic imaging. Myelography is a form of fluoroscopy because it involves the usage of a contrast dye that is injected into the space within the vertebral column. The dye is usually injected using a lumbar puncture, a medical procedure that includes making a small hole in the lumbar part of your spine. At the same time, it uses a CT scan (occasionally, an X-ray scan) to highlight the dye in white. This way, doctors can visualize structures like your spinal cord in real time.1Walker, M. T., Spitzer, E. M., Murugusundaram Veeramani, & Russell, E. J. (2011). Anatomy, imaging, and common pain-generating degenerative pathologies of the spine. Elsevier EBooks, 53–82. https://doi.org/10.1016/b978-1-4377-2242-0.00018-3
Myelogram vs. Myelography
A myelogram is an image produced by a myelography procedure. It is shown on a radiograph, such as an X-ray or CT scan film. It shows details about the spinal cord, various nerve roots, and their surrounding anatomical parts. On the other hand, myelography is the procedure in which a health professional trained in imaging and nuclear medicine visualizes these body parts. A qualified radiologist interprets the results.
Types of Myelograms
Sometimes, myelograms are classified on the basis of the region being scanned or the type of scans being used, such as:
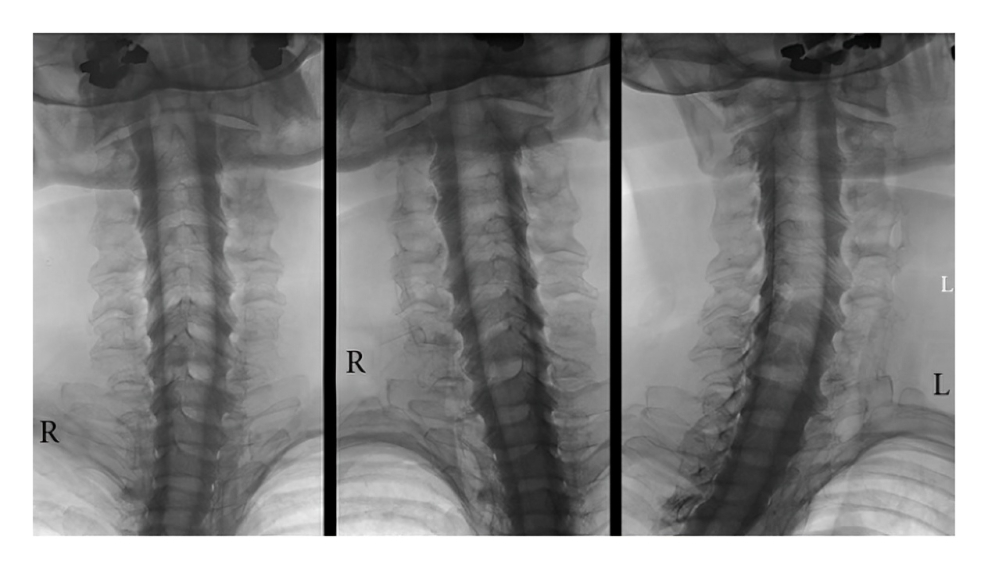
- Cervical myelograms focus on the cervical spine present in your neck
- Thoracic myelograms show structures in your thoracic vertebral column or chest
- Lumbar myelograms are the most common ones and target the region of your lower back
- Conventional X-ray myelograms use X-rays to highlight various anomalies
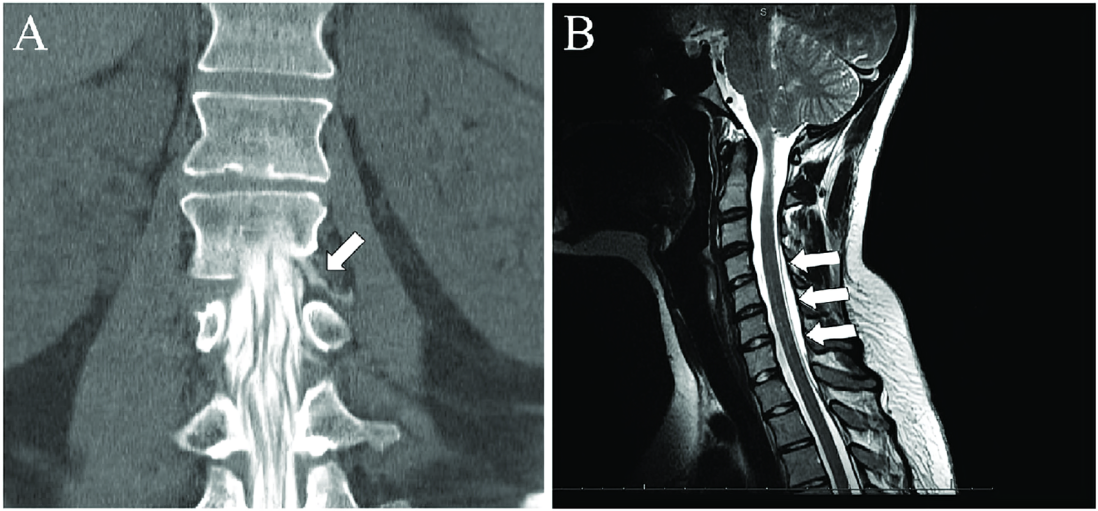
- CT myelograms use computerized tomography (a type of highly concentrated X-ray scan) to visualize your spine
- MR myelograms use the safe imaging of an MRI scan2Gaillard, F. (2024). Myelography. Radiopaedia; Radiopaedia.org. https://radiopaedia.org/articles/myelography
Indications for Myelography
Given the availability of nonionizing imaging like MRI scans, myelography is usually restricted to situations where other modalities cannot be employed. It is excellent for visualizing pathologies of the thecal sac, a layer of protective sheath or meninges that surrounds the spinal cord.3Patel, D. M., Weinberg, B. D., & Hoch, M. J. (2020). CT Myelography: Clinical Indications and Imaging Findings. RadioGraphics, 40(5), 1353-1365. https://doi.org/10.1148/rg.2020190135
In addition, certain populations cannot undergo routine MRI exams, e.g., patients with pacemakers, metallic screws, and wires inserted during surgery, patients who cannot lie still and complete an MRI scan, etc. Myelography is an important diagnostic tool for such patients.
Myelography is often performed when patients show signs and symptoms of neurological and musculoskeletal damage in their backbone, such as:
- Back pain
- Numbness and tingling in arms or legs
- Weakness in one’s arms or legs
- Trouble standing or walking
- Loss of bladder control
- Loss of bowel control
- Sharp pain, shooting down the legs
- Unexplained muscle weakness4Hasan Burak Gündüz, Aysegul Esen Aydin, Aysegul Ozdemir Ovalioglu, Emel, E., Ozden Erhan Sofuoglu, Mustafa Levent Uysal, Muslum Gunes, Murad Asiltürk, & Talat Cem Ovalioglu. (2021). The Role and Contribution of Lumbar Myelography in the Diagnosis and Treatment of Patients With Lumbar Degenerative Disorders: Clinical and Statistical Evaluation of Post-Myelography Treatment of 63 Patients. Cureus. https://doi.org/10.7759/cureus.15987
Nerve Damage
The contrast dye used in mylography highlights the nerves within the spinal canal. This way, areas of potential nerve damage or neuropathy become more visible to physicians, who can determine if you have any nerve compression, impingement, or trauma causing your symptoms.
CSF Leaks
Cerebrospinal fluid leaks happen when the fluid that surrounds and protects structures like the brain and spinal cord starts to leak out of its regular pathways. They are often caused by a tear in the dura mater and result in head and neck pain, photophobia, and nausea. Myelography shows the exact location of these leaks with high precision, helping doctors diagnose and treat them in time.
Spinal Abnormalities
Myelograms are an important modality for identifying as well as differentiating between different abnormalities of the spine and the spinal canal:
- Spinal stenosis occurs when the spinal canal narrows, putting pressure on the nerves and spinal cord. This compression can cause pain, stiffness, or weakness. Myelography pinpoints the exact locations where the spinal cord is restricted during spinal stenosis.
- Herniated discs happen when the nucleus pulposus — the soft inner substance of a disc — bulges out and puts pressure on nerves or the spinal cord nearby. Myelography highlights any such bulging or protruding parts pressing on your nearby nerves or the spinal cord.
- Degenerative disc disease, in which the discs in the spine wear away over time. This can change the spinal canal and put pressure on nerves. Myelography outlines these areas of damage, as well as their severity.
- Myelography can show various changes associated with spine arthritis, such as the presence of bony spurs or osteophytes and spondylolisthesis, which is the displacement of one vertebra over the other.
Tumors & Malignancy
Doctors use myelography to assess how various tumors and types of cancer impact the spinal column for prompt diagnosis and treatment. It can indicate how metastatic lesions affect the spinal canal, particularly leptomeningeal involvement. It helps design targeted treatments like radiation therapy. Myelography can also help identify various primary tumors of the spinal cord, such as:
- Schwannomas
- Astrocytomas
- Ependymomas
- Hemangioblastomas
- Oligodendrogliomas
- Neurofibromas
- Gangliogliomas
Infection & Inflammation
Myelography can outline collections of pus and inflammatory fluids in the spinal canal, particularly when these infections lead to swelling and space-occupying lesions in the spinal column. Examples include:
- Epidural abscess
- Discitis
- Spinal osteomyelitis
- Tuberculous spondylitis
- Pyogenic spondylitis
- Fungal spondylitis
- Arachnoiditis
Cysts
Cysts are small fluid-filled sacs that develop within the spinal column. They often impact surrounding structures if they are large enough in size, all of which can be determined using myelography. Examples of cysts diagnosed by myelography include:
- Arachnoid cysts
- Synovial cysts
- Epidermoid cysts
- Dermoid cysts
- Radicular cysts
- Neuroenteric cysts
What are the Contraindications for Myelography?
Myelography has a few contraindications, which are mainly associated with the use of X-rays, contrast dyes as well as the involvement of lumbar puncture procedure, including:
- Allergy to constituents of contrast dye, especially iodinated contrast media
- Pregnancy and lactating mothers
- Conditions with abnormally raised intracranial pressure
- A patient who is unable or unwilling to remain still or follow instructions
- Patients with a medical history of connective tissue disorders, e.g., Marfan syndrome, Ehlar Danlos syndrome
- Uncontrolled hypertension and diabetes
- Infections within the central nervous system, e.g., encephalitis, meningitis5Myelography. (2020). Medlineplus.gov. https://medlineplus.gov/lab-tests/myelography/
What can I do for Myelography Prep?
Myelography does not involve extensive preparation. The main preparation lies in ensuring the patient is not allergic to contrast or can get harmed by radiation during the process.6Pomerantz, S. R. (2016). Myelography. Handbook of Clinical Neurology, 193–208. https://doi.org/10.1016/b978-0-444-53485-9.00010-6
History & Examination
Doctors will ask you about your current complaints, past medical history, and any allergies you have to medications. In addition, they will ask you to undergo a neurological exam, a spine exam, a pain assessment, and a nutritional status exam. Lab investigations for myelography include:
- Complete blood count
- Coagulation profile
- Serum electrolytes
- Renal function tests
- Infection screening
Informed Consent
Informed consent for myelography usually involves explaining all the steps, risks, and expected outcomes of a myelogram. It may also require additional consent for a lumbar puncture, which is the procedure through which contrast dye is injected into your spinal canal.
Do’s & Don’ts Before Myelography
Your doctor will ask you to adopt a few practices to make sure you have a comfortable experience during your myelography procedure, such as:
- Inform your healthcare team about any allergic reactions you have had to medications. This is even more important if you have a past or family history of reactions to contrast dyes used in fluoroscopic procedures.
- Other than blood thinners, you can continue to take your prescribed medications as usual unless advised.
- Don’t eat or drink anything for at least 6 hours before your myelography procedure. If absolutely necessary, your doctor might allow you to take your daily medications with a small sip of water.
- Arrive at least 60 minutes before your scheduled appointment time to allow for any pre-procedure prep.
- Bring all relevant X-ray, CT, or MRI scans of your spine or brain to your myelography procedure.
- Leave all valuable items like jewellery at your house to avoid misplacing them.
- If you choose to have an outpatient procedure, avoid taking blood thinners like aspirin for at least five days before your appointment. In addition, bring a caregiver with you to drive you back home, as you cannot drive immediately after a myelogram.
Step-by-Step Procedure for Myelography
Myelography is performed in a hospital’s radiology or nuclear medicine department. It involves a team of nurses, radiologists, and radiologic imaging technicians and can be performed as an inpatient or outpatient procedure.
Anesthesia & Premedication
Local anesthesia is the most common type of anesthesia used for myelography. However, general anesthesia might be used, too. A prophylactic antibiotic cover is usually not required. However, different drugs to prevent anxiety and vomiting are now being used to improve patients’s experiences during myelography, such as:
- Diazepam
- Lorazepam
- Ondansetron
- Metoclopramide
As far as the contrast dye for myelography is concerned, it is usually a water-soluble, nonionic, and iodinated substance. It should also be visualized easily using radiologic modalities. Examples include:
- Iohexol
- Iopamidol
- Iopanoic acid
During the Myelography Procedure
First of all, you will be asked to change into a hospital gown, lie on your side, and draw your legs and knees up to your chest. This position widens the space in your spinal canal. Your back will be exposed.
- Depending on your condition, an antiseptic solution cleans a part of your lumbar (and sometimes cervical) region. The lumbar region constitutes the lower back, where the lumbar puncture occurs.
- A sterile needle is inserted into your spinal canal.
- The doctor slowly injects a contrast dye into the spinal canal via this needle.
- As the dye circulates throughout your spinal column, an X-ray or CT machine takes images of your spinal cord and its surrounding structures.7Bahman Rasuli. (2024, July 3). CT myelography. Radiopaedia; Radiopaedia.org. https://radiopaedia.org/articles/ct-myelography
What happens after a Myelogram?
Once the myelography procedure ends, you will be asked to lie down for at least two hours to prevent accidental CSF leaks. Your doctor will give you extra fluids to flush out the contrast dye, as its accumulation can lead to headaches. They will monitor and discharge you once you are vitally stable. You will also be asked to rest at home and avoid unnecessary movements for the remainder of the day.
What risks are associated with Myelography?
The most significant risk associated with myelography is related to complications of lumbar puncture and an allergic reaction to the contrast dye used to highlight various structures. Allergies can cause anything from milder symptoms like superficial swelling, headache, and hives to multiorgan failure and death during anaphylactic shock. On the other hand, the risks of lumbar puncture associated with myelography are:
- Hemorrhage
- Infection at the injection site
- Rupture of meninges
- Severe headache
- CSF leakage
- Short-term numbness, tingling sensations, or pain in your back and legs
Myelography vs. MRI
Myelography is a relatively older diagnostic modality than MRI. In fact, MRI scans have mostly replaced myelograms for most indications. This is because of the totally noninvasive nature of the MRI, as well as the absence of potentially harmful radiation. However, myelography is still a top choice for patients for whom an MRI is contraindicated or cannot be used.8Christoph Ozdoba, Gralla, J., Rieke, A., Binggeli, R., & Schroth, G. (2011). Myelography in the Age of MRI: Why We Do It, and How We Do It. Radiology Research and Practice, 2011, 1–6. https://doi.org/10.1155/2011/329017
Conclusion
Myelography is a diagnostic modality that uses X-rays and a contrast dye to visualize various conditions of the spinal cord and its nearby structures. The dye highlights various anomalies, and the results are captured on a machine. After recovery time, patients can be discharged on the same day. It is associated with some pain and minor risks. MRI scans have mostly replaced it.
Refrences
- 1Walker, M. T., Spitzer, E. M., Murugusundaram Veeramani, & Russell, E. J. (2011). Anatomy, imaging, and common pain-generating degenerative pathologies of the spine. Elsevier EBooks, 53–82. https://doi.org/10.1016/b978-1-4377-2242-0.00018-3
- 2Gaillard, F. (2024). Myelography. Radiopaedia; Radiopaedia.org. https://radiopaedia.org/articles/myelography
- 3Patel, D. M., Weinberg, B. D., & Hoch, M. J. (2020). CT Myelography: Clinical Indications and Imaging Findings. RadioGraphics, 40(5), 1353-1365. https://doi.org/10.1148/rg.2020190135
- 4Hasan Burak Gündüz, Aysegul Esen Aydin, Aysegul Ozdemir Ovalioglu, Emel, E., Ozden Erhan Sofuoglu, Mustafa Levent Uysal, Muslum Gunes, Murad Asiltürk, & Talat Cem Ovalioglu. (2021). The Role and Contribution of Lumbar Myelography in the Diagnosis and Treatment of Patients With Lumbar Degenerative Disorders: Clinical and Statistical Evaluation of Post-Myelography Treatment of 63 Patients. Cureus. https://doi.org/10.7759/cureus.15987
- 5Myelography. (2020). Medlineplus.gov. https://medlineplus.gov/lab-tests/myelography/
- 6Pomerantz, S. R. (2016). Myelography. Handbook of Clinical Neurology, 193–208. https://doi.org/10.1016/b978-0-444-53485-9.00010-6
- 7Bahman Rasuli. (2024, July 3). CT myelography. Radiopaedia; Radiopaedia.org. https://radiopaedia.org/articles/ct-myelography
- 8Christoph Ozdoba, Gralla, J., Rieke, A., Binggeli, R., & Schroth, G. (2011). Myelography in the Age of MRI: Why We Do It, and How We Do It. Radiology Research and Practice, 2011, 1–6. https://doi.org/10.1155/2011/329017

