Splenectomy refers to the surgical removal of the spleen, either partially or entirely, and is typically performed when the spleen becomes damaged, diseased, or is contributing to certain blood disorders. The spleen is a vital organ of the immune system, located just beneath the ribcage on the left side of the upper abdomen. It plays a key role in filtering the blood by removing old or damaged red blood cells, storing white blood cells, and helping to fight blood-borne infections.
What is Splenectomy?
Splenectomy is a surgical procedure in which all or part of the spleen is removed. It is generally considered when less invasive treatments are ineffective or inappropriate. Common indications include trauma (such as a ruptured spleen), hematologic diseases (like hereditary spherocytosis or idiopathic thrombocytopenic purpura), certain cancers (like lymphoma), or autoimmune conditions affecting blood cells.1Katz SC, Pachter HL. Indications for splenectomy. Am Surg. 2006 Jul;72(7):565-80. PMID: 16875077.
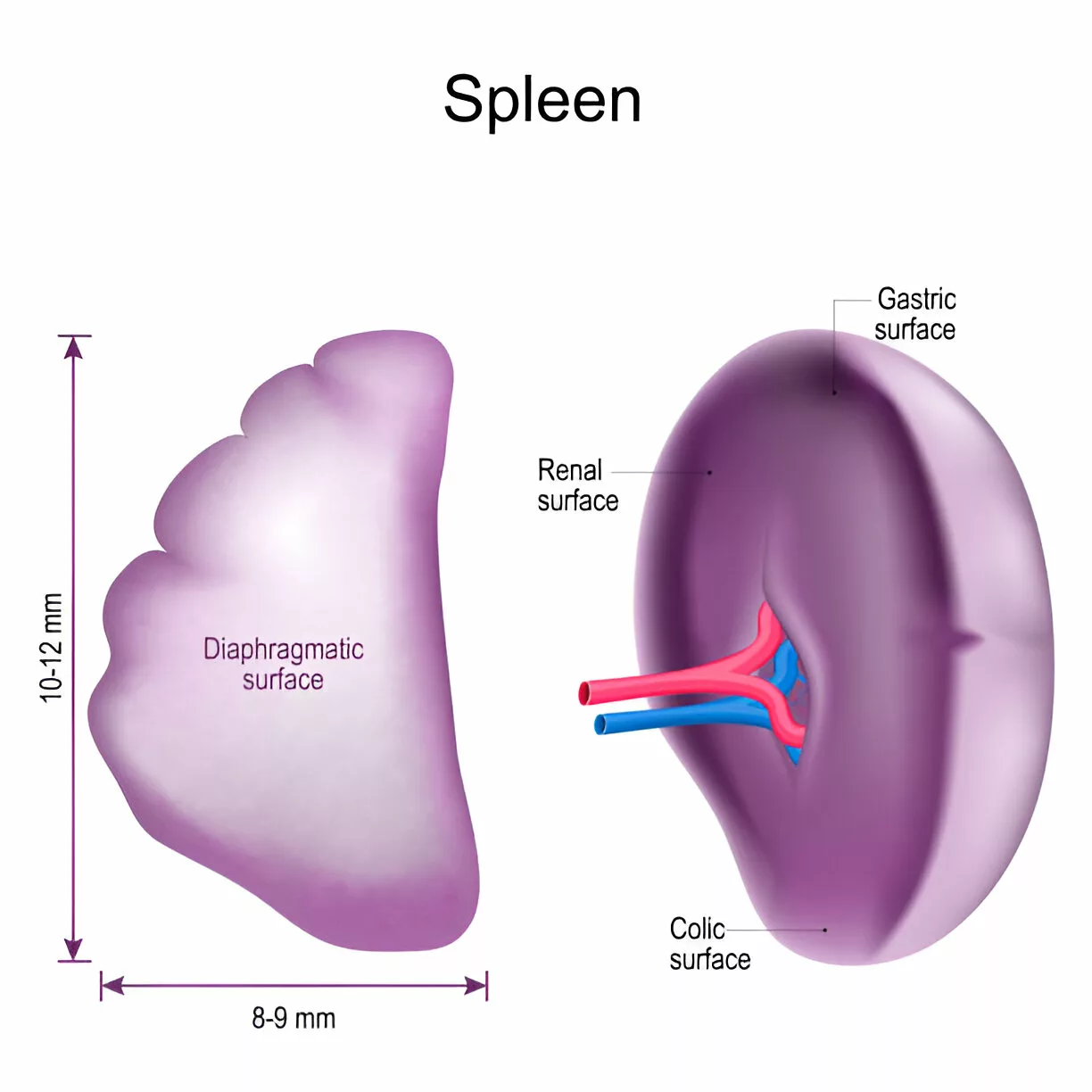
Spleen Anatomy
To understand the procedure and outcomes of splenectomy, it’s important to have a basic understanding of spleen anatomy and function. The spleen is a soft, vascular organ located in the upper left abdomen, just beneath the diaphragm, and protected by the lower ribs. It is approximately 10–12 cm long and 8–9 cm wide. The spleen has two main surfaces: the diaphragmatic surface, which is smooth and convex, and the visceral surface, which has impressions from surrounding organs such as the stomach (gastric surface), kidney (renal surface), and colon (colic surface). It gets blood from the splenic artery and empties it into the splenic vein, which joins the portal vein to return blood to the liver.2Mebius, R. E., & Kraal, G. (2005). Structure and function of the spleen. Nature reviews. Immunology, 5(8), 606–616. https://doi.org/10.1038/nri1669
Functions of Spleen
Before we talk about splenectomy, one should first understand what spleen does.
Hematologic Function:
The spleen acts as an internal filtration system that gathers aged or broken red blood cells from the bloodstream. It also plays a role in recycling iron and breaking down hemoglobin, the oxygen-carrying protein in red blood cells. This process helps maintain healthy blood composition and prevents the accumulation of dysfunctional cells.
Immunologic Function:
The spleen is a critical immune organ, producing various white blood cells and antibodies. It helps detect and eliminate blood-borne pathogens by filtering microbes and foreign particles. Additionally, it contributes to the production of immunoglobulins and supports immune surveillance and response.

Indications for Splenectomy
Medical professionals opt for splenectomy under several conditions, including:3Bonnet, S., Guédon, A., Ribeil, J. A., Suarez, F., Tamburini, J., & Gaujoux, S. (2017). Indications and outcome of splenectomy in hematologic disease. Journal of visceral surgery, 154(6), 421–429. https://doi.org/10.1016/j.jviscsurg.2017.06.011
- Trauma or injury: This includes splenic rupture or deep lacerations, typically from accidents or blunt abdominal trauma.
- Enlarged spleen (splenomegaly): This can be brought on by a number of illnesses, including thrombocytopenia, portal hypertension, and hemolytic anemia.
- Hypersplenism: A condition where the spleen overactively removes blood cells—especially red blood cells, white blood cells, and platelets—causing cytopenias.
- Spleen tumors: Benign or malignant splenic tumors.
- Infections: Severe splenic infections, including splenic abscesses
- Autoimmune diseases: Splenectomy is a possible treatment for autoimmune diseases such as Evans syndrome and ITP (immune thrombocytopenic purpura).
- Blood disorders: In the case of various blood disorders for example, hereditary spherocytosis which is characterized by abnormal red blood cells, splenectomy may be recommended as a therapeutic measure to alleviate symptoms and improve overall health.
Contraindications of Splenectomy
While there are no absolute contraindications to splenectomy, there are specific medical conditions where it’s generally avoided due to lack of benefit or increased risk of severe complications.4Schrier, S. L., & Grace, R. F. (2024). Elective, diagnostic, or therapeutic splenectomy. UpToDate. Retrieved April 13, 2025, from https://www.uptodate.com/contents/elective-diagnostic-or-therapeutic-splenectomy?search=splenectomy&source=search_result&selectedTitle=2~150&usage_type=default&display_rank=2#H579413995
- Severe Cardiovascular Disease: Splenectomy is not recommended for patients with advanced heart conditions, because of higher risks and potential difficulties in the operation.
- Uncontrolled Infection: Surgery might not be performed when the infection is active and extensive, for a splenectomy may serve to spread pathogens systemically.
- Immunodeficiency Disorders: When people have immunodeficiency disorders, spleen removal can further impair the immune system.
- Portal Hypertension: While not always a strict contraindication, it significantly increases the risk of intraoperative bleeding and postoperative complications.
- Autoimmune Lymphoproliferative Syndrome (ALPS): In these patients, splenectomy can lead to life-threatening infections, making it a generally contraindicated procedure.
- Gaucher Disease: Removing the spleen in these cases may worsen disease progression by promoting Gaucher cell accumulation in other organs.
- Hereditary Stomatocytosis and Xerocytosis: These rare red cell membrane disorders have a higher risk of thromboembolic events after splenectomy, outweighing any potential benefits.
Splenectomy Techniques
There are two main surgical approaches used for splenectomy:
Open splenectomy:
This traditional method involves making a large incision in the abdomen. It’s often reserved for emergencies, very large spleens, or situations involving significant bleeding. While it allows for better access and control, the recovery is generally slower compared to laparoscopic techniques.
Laparoscopic Splenectomy:
Laparoscopic splenectomy5Javed, I., Malik, A. A., Khan, A., Allahnawaz, Shamim, R., & Ayyaz, M. (2014). Laparoscopic splenectomy. Journal of the College of Physicians and Surgeons–Pakistan: JCPSP, 24(5), 361–364. is a minimally invasive surgery in which the spleen is taken out through small incisions with specially designed instruments called laparoscopes. In comparison to open splenectomy, this procedure has several advantages. Generally, three or four tiny cuts are made instead of one large cut in the abdomen.
This results in:
- Less pain
- Shorter hospital stays
- Fast recovery time
- Reduced risk of infection
However, not all patients are suitable candidates for this method, especially those with very large spleens, extensive adhesions, or active bleeding.
How to Prepare for Splenectomy?
One of the most important steps before a planned splenectomy is vaccination. Because the spleen plays a crucial role in fighting certain bacteria—especially encapsulated organisms—patients without a spleen are at increased risk of severe infections. Vaccinations should ideally be given at least two weeks before surgery in elective cases, or as soon as the patient is stable postoperatively in emergency splenectomies.
The key recommended vaccines include:
- Pneumococcal conjugate vaccine (PCV13)
- Pneumococcal polysaccharide vaccine (PPSV23)
- Haemophilus influenzae type b (Hib) vaccine
- Meningococcal Vaccines (both MenACWY and MenB)
- Annual flu shot and staying up to date on routine vaccines like Tdap and COVID-19
Patients should also practice good hygiene, wash hands frequently, and avoid close contact with sick individuals. Moreover, any signs of infection—such as fever, chills, shortness of breath, or stiff neck—after surgery should be promptly evaluated.
Steps of Splenectomy
The specific procedures performed during a splenectomy will vary depending on the surgeon’s selected surgical approach. Nonetheless, general procedures for an open splenectomy include:
General Anesthesia Administration:
As with any major surgery, ensuring the patient’s comfort and safety is the top priority. During an open splenectomy, the anesthesiologist administers general anesthesia to keep the patient fully asleep and pain-free throughout the procedure.
Making an Incision in the Abdomen:
The surgeon makes a large incision on the left side of the abdomen, usually just below the rib cage, extending toward the center. This provides clear access to the spleen and surrounding structures.
Mobilizing the spleen by dividing its attachments:
The spleen is held in place by ligaments and surrounding blood vessels. The surgeon carefully cuts these attachments using surgical tools or energy devices, which allows the spleen to be mobilized and safely handled.
Clamping & Dividing the splenic artery and vein:
To control bleeding, it is critical to identify, divide and clamp the splenic artery. This step helps to avoid excessive blood loss and ensure a safe removal.
Removing the spleen:
A surgeon can take out the spleen safely after they make sure the splenic artery and vein are safely handled. They usually use specific instruments to carefully move the spleen for this.
Bleeding Control:
The surgical team must ensure that all bleeding is stopped following spleen removal. This involves closing any open blood vessels using stitches, heat, or different techniques.
Closing the incision:
Finally, the surgeon closed the incision using sutures or surgical staples. This helps protect the internal organs and supports proper wound healing.
Splenectomy Recovery
After splenectomy, patients are required to remain in the hospital for a couple of days to check for any complications. Recovery periods may depend on the surgical technique and the individual’s condition. Nonetheless, the following general advice is suggested:
- Rest from strenuous activities for several weeks
- Hygiene maintenance
- Proper medication
- Follow-up appointments
Splenectomy Complications
Having your spleen removed can be beneficial. However, it’s not without potential pitfalls and unwanted reactions. Common issues that might arise encompass:
Bleeding:
This is the most common complication that can arise during or post-surgery. You might get dizzy, have a faster heartbeat, or notice swelling and redness near the cut. Treatments can range from simply applying pressure, to possibly needing a blood transfusion, or even additional surgery.
Subphrenic Abscess:
A subphrenic abscess is a postoperative complication of splenectomy involving an infection in the space under the diaphragm. Early identification and intervention can prevent related risks and complications.
Infection:
Wound infections are common and can spread. Being overweight, using tobacco, and having diabetes can raise your risk. Symptoms include fever, localized redness, swelling, or pus discharge. Treatment ranges from antibiotics to surgical drainage, depending on severity.
Wound healing problems:
Delayed healing, incisional hernias, or wound dehiscence may occur. Redness, pain, or gaping wounds require prompt wound care, antibiotics, and possibly revision surgery.
Pancreatitis:
The pancreas may become inflamed due to harm from the operation or its own enzymes leaking. Fever, throwing up, feeling sick, and pain in the upper belly are some of the common signs. If it’s really bad, one might need IV fluids, medicine for the pain, and sometimes an operation.
Thrombosis:
A blood clot in a vein can be serious if it travels to the lungs or brain. Things like getting older, smoking, and being overweight may put you at risk. Symptoms vary by location but may include pain, redness, swelling, or shortness of breath. Anticoagulant therapy is often required.
Pneumonia:
Having your spleen removed can weaken your immune system. This makes lung infections more common. Look out for chest pain, fever, breathing problems, and coughing. If you get sick, you might need antibiotics or oxygen upon the prescription of the doctor. The doctors might even recommend a stay in the hospital depending upon your condition.
Long-term complications:
Long-term complications of splenectomy include:
Increased Risk of Infections After Splenectomy
Splenectomized patients suffer immunologically impoverished states rendering them susceptible to infections generally and encapsulated bacterial infections particularly. Patients become more susceptible to infections, especially from encapsulated bacteria such as Streptococcus pneumoniae, Haemophilus influenzae, and Neisseria meningitidis. These bacteria are coated with a polysaccharide capsule, acting as a shield against the immune system. The spleen plays a crucial role in purging these germs from the bloodstream, making its absence leave individuals more susceptible.
Following splenectomy, the following infections are the most typical types:
- Pneumococcal pneumonia: This is streptococcus pneumonia, a serious and sometimes fatal bacterial infection of the lungs.
- Meningitis: Meningitis, a bacterial or viral infection of the meninges mainly caused by Neisseria meningitis, Streptococcus pneumoniae, and Haemophilus influenzae.
- Sepsis: An overreaction of the body to an infection that can be very dangerous and even lethal.
Overwhelming Post-Splenectomy Infection (OPSI)
OPSI6Morgan, T. L., & Tomich, E. B. (2012). Overwhelming post-splenectomy infection (OPSI): a case report and review of the literature. The Journal of Emergency Medicine, 43(4), 758–763. https://doi.org/10.1016/j.jemermed.2011.10.029 is an infrequent but potentially lethal complication of splenectomy that predominantly afflicts children and adolescents. A highly contagious illness with the potential to be lethal. Bacteria responsible for OPSI include Neisseria meningitidis, Haemophilus influenzae, and Streptococcus pneumoniae.
OPSI typically develops in the initial years following splenectomy and can cause symptoms such as:
- High fever
- Chills
- Severe pain
- Rapid breathing
- Confusion
- Seizures
Early diagnosis and intensive treatment may work for OPSI. The treatment mostly involves hospitalization, administration of intravenous antibiotics, and other supportive care measures.
To prevent OPSI, one must undergo:
- Immunization against bacteria that are encapsulated.
- Instruction in this regard to the patient and relatives on increased infection risk.
- Always seek immediate medical attention when there are signs of an infection.
- Some of the at-risk people may have access to prophylactic antibiotics with a recommendation from the doctor.
Leucocytosis Post-Splenectomy
One of the side effects includes a temporary increase in the amount of leucocytes particularly neutrophils referred to as leucocytosis.This response is very frequent when the spleen is absent and most often it disappears within several weeks.This is so because after splenectomy, the remaining immune system parts take over the spleen’s functions which results in a temporary need for an increase in white blood cells that fight infections.
Increased Risk of Cardiovascular Disease
Research has demonstrated a connection between splenectomy and a higher risk of cardiovascular disease, which includes:
- Atherosclerosis: Plaque accumulation that causes artery hardening and narrowing.
- Hypertension: High blood pressure is known as hypertension.
- Coronary artery disease: The narrowing of the arteries supplying blood to the heart is known as coronary artery disease.
Bone Marrow Changes
In certain cases, some patients may undergo changes of the bone marrow.These modifications may show up as:
- Myeloid hyperplasia: which leads to an increased number of immature white blood cells, is usually harmless.
- Reduced red blood cell production: Anemia may result from this.
- Reduced platelet production: This could also be a cause of bleeding.
Post-Op Experience
After a splenectomy, patients may experience some side effects, including:
- Fatigue
- Pain
- Difficulty sleeping
- Appetite changes
- Increased susceptibility to infections
How to Minimize Complications After Splenectomy?
Preventing complications after splenectomy involves a comprehensive approach both before and after surgery. Patients are encouraged to maintain a healthy lifestyle, eat a balanced diet, engage in regular physical activity, and manage body weight. Blood pressure and cholesterol should be well controlled, and individuals are strongly advised to quit smoking. Proper management of chronic conditions like diabetes is also essential. Routine medical follow-ups enable ongoing monitoring, personalized interventions, and timely adjustments in care plans—creating a robust framework to reduce long-term cardiovascular risks.
Partial Splenectomy
Partial splenectomy is a procedure where part of the spleen remains intact. This approach is considered when the underlying medical condition allows for the removal of only the affected or damaged part of the spleen while retaining its essential functions. The decision for a partial splenectomy is often influenced by factors such as the specific pathology, the extent of spleen involvement, and the overall health of the individual.7Uranues, S., Grossman, D., Ludwig, L., & Bergamaschi, R. (2007). Laparoscopic partial splenectomy. Surgical endoscopy, 21(1), 57–60. https://doi.org/10.1007/s00464-006-0124-2
Distal Pancreatectomy & Splenectomy – A Combined Procedure
Distal pancreatectomy with splenectomy, also known as the whole spleen and the tail and body of the pancreas, is also a surgical procedure.8Labib, J. Y., Lovasik, B. P., Lad, N., Saltalamacchia, J., Maithel, S. K., Sarmiento, J. M., Staley, C. A., Sweeney, J. F., & Kooby, D. A. (2022). Implications of leukocytosis following distal pancreatectomy splenectomy (DPS) and association with postoperative complications. Journal of Surgical Oncology, 126(6), 1012–1020. https://doi.org/10.1002/jso.26988 It is used to treat a range of illnesses, such as:
- Localized in the distal pancreas, pancreatic cancer
- Body and tail affected by chronic pancreatitis
- Pseudocysts in the pancreas
- Splenic and pancreatic trauma
Laparoscopic procedures are performed through a small incision and therefore make use of minimally invasive techniques. It has several benefits compared to open surgery, among them being shorter recovery periods, less pain, and fewer complications.
The surgeon meticulously separates the spleen from the distal part of the pancreas that is removed. Finally, the rest of the pancreas tissue is then joined to the small intestines to make sure that they are properly digested.
Wrap Up
In essence, a splenectomy is a significant operation with risks and benefits.Therefore, patients and their relatives should know that they need qualified post-treatment care, and possible side effects and consequences._Furthermore, it would be the duty of the concerned doctor to discuss the specifications of the undertaking.Patients should be cautious and careful since precaution is better than cure.
Refrences
- 1Katz SC, Pachter HL. Indications for splenectomy. Am Surg. 2006 Jul;72(7):565-80. PMID: 16875077.
- 2Mebius, R. E., & Kraal, G. (2005). Structure and function of the spleen. Nature reviews. Immunology, 5(8), 606–616. https://doi.org/10.1038/nri1669
- 3Bonnet, S., Guédon, A., Ribeil, J. A., Suarez, F., Tamburini, J., & Gaujoux, S. (2017). Indications and outcome of splenectomy in hematologic disease. Journal of visceral surgery, 154(6), 421–429. https://doi.org/10.1016/j.jviscsurg.2017.06.011
- 4Schrier, S. L., & Grace, R. F. (2024). Elective, diagnostic, or therapeutic splenectomy. UpToDate. Retrieved April 13, 2025, from https://www.uptodate.com/contents/elective-diagnostic-or-therapeutic-splenectomy?search=splenectomy&source=search_result&selectedTitle=2~150&usage_type=default&display_rank=2#H579413995
- 5Javed, I., Malik, A. A., Khan, A., Allahnawaz, Shamim, R., & Ayyaz, M. (2014). Laparoscopic splenectomy. Journal of the College of Physicians and Surgeons–Pakistan: JCPSP, 24(5), 361–364.
- 6Morgan, T. L., & Tomich, E. B. (2012). Overwhelming post-splenectomy infection (OPSI): a case report and review of the literature. The Journal of Emergency Medicine, 43(4), 758–763. https://doi.org/10.1016/j.jemermed.2011.10.029
- 7Uranues, S., Grossman, D., Ludwig, L., & Bergamaschi, R. (2007). Laparoscopic partial splenectomy. Surgical endoscopy, 21(1), 57–60. https://doi.org/10.1007/s00464-006-0124-2
- 8Labib, J. Y., Lovasik, B. P., Lad, N., Saltalamacchia, J., Maithel, S. K., Sarmiento, J. M., Staley, C. A., Sweeney, J. F., & Kooby, D. A. (2022). Implications of leukocytosis following distal pancreatectomy splenectomy (DPS) and association with postoperative complications. Journal of Surgical Oncology, 126(6), 1012–1020. https://doi.org/10.1002/jso.26988