Steatorrhea, commonly referred to as fatty stool, is a symptom of fat malabsorption characterized by greasy, bulky, foul-smelling stools that are challenging to flush. It’s not a disease itself, but it indicates something is seriously wrong with the intestines, the pancreas, or the liver, in the background. Untreated steatorrhea leads to severe malnutrition and similar outcomes, making it a serious health concern. Therefore, we need to diagnose it early and treat it timely, to prevent the complications, and also catch deadlier underlying issues such as pancreatic cancer on time.
How does Steatorrhea occur?
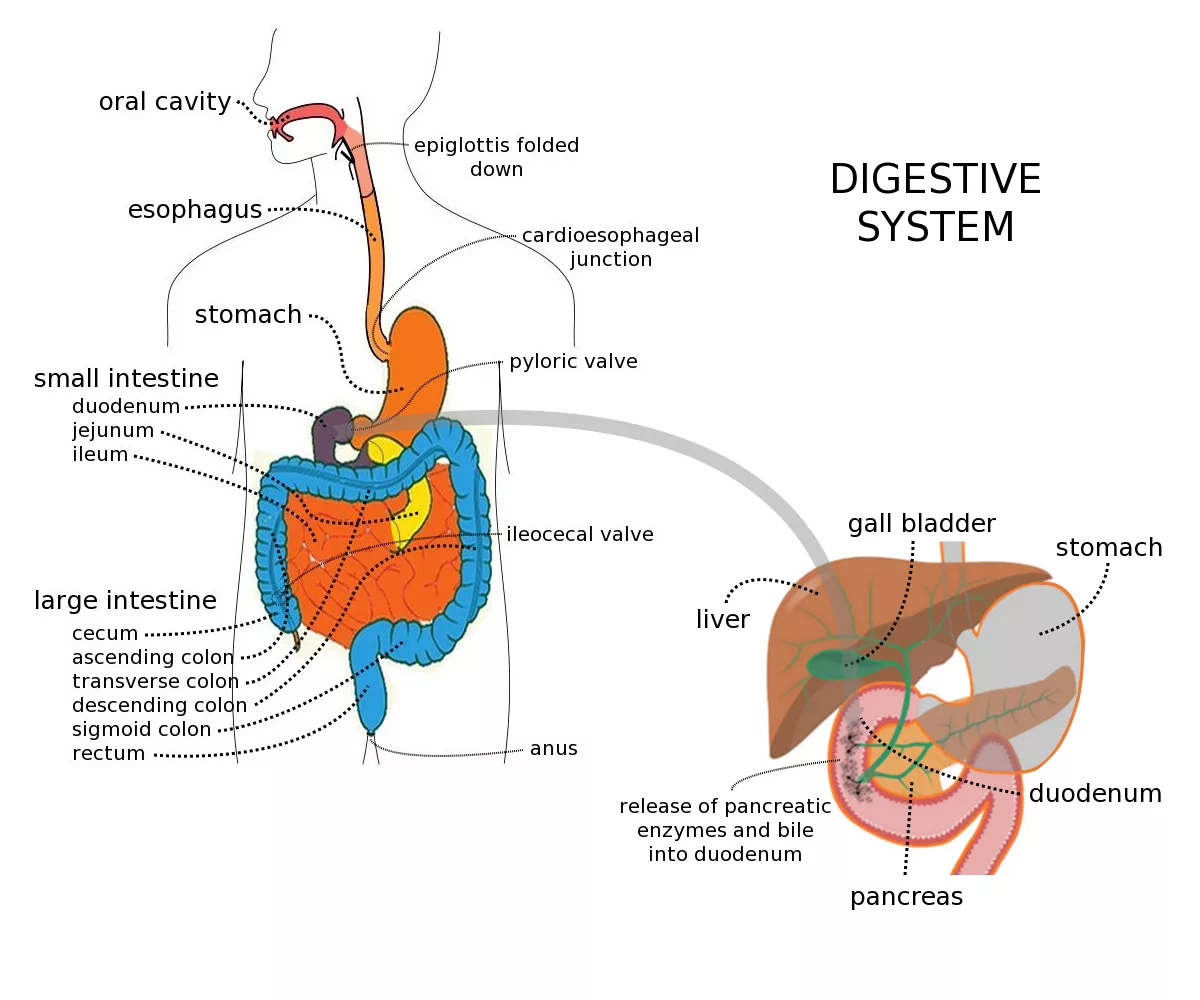
Any defect in the digestion of fat or its absorption through the villi of the small intestine gives rise to steatorrhea. In a healthy body, coordination between the liver, intestines, and the pancreas is responsible for digesting a fatty diet. When the fat we eat enters the duodenum, our liver and the pancreas secrete their juices into the small intestine to come in contact with the meal. Liver juice or the bile emulsifies larger fat globules into smaller ones, whereas pancreatic juice, through its lipid-digesting enzymes, further breaks it down into even smaller molecules called fatty acids and triglycerides. These smaller molecules can now be easily absorbed through tiny projections called villi, in our small intestine. But if there is a defect in any step of this process, it makes more fat pass into the stool, causing steatorrhea.
What causes Steatorrhea?
Steatorrhea can arise secondary to a number of problems with our pancreas, liver, or intestines:
Disorders of the Pancreas:
These mainly include the conditions that result in Exocrine Pancreas Insufficiency (EPI), i.e, insufficient production of digestive enzymes, such as:
- Chronic Pancreatitis: It’s a long-standing inflammation of the pancreas. By damaging the cells responsible for digestive enzymes, it can cause steatorrhea.
- Cystic Fibrosis: It’s a genetic condition characterized by abnormal production and accumulation of mucus in your body, causing breathing and digestive problems. 85% of patients with this condition also have a defect with their exocrine portion of the pancreas.1Paranjape, S. M., & Mogayzel, P. J., Jr (2014). Cystic fibrosis. Pediatrics in review, 35(5), 194–205. https://doi.org/10.1542/pir.35-5-194
- Pancreatic tumors, surgeries, and other conditions that might obstruct the pancreatic ducts or lead to resection of a portion of the pancreas, also produce fat malabsorption and hence, steatorrhea.
Disorders of the Liver & Bile Ducts:
These include conditions that either interfere with the production of bile or its secretion through the bile ducts into the duodenum.
- Primary Biliary Cholangitis (PBC): It’s a chronic autoimmune disease that causes inflammation and destruction of the bile ducts within the liver.
- Primary Sclerosing Cholangitis (PSC): It’s a chronic inflammatory disease that affects both the intrahepatic and extrahepatic bile ducts.
- Cholestasis: It’s a condition in which bile flow from the liver to the duodenum is impaired due to either mechanical or metabolic hindrance.
- Liver Cirrhosis
- Liver Failure
Disorders of the Intestine:
These include conditions that cause either maldigestion or poor absorption of fats.
- Celiac disease: It’s an autoimmune disease in which gluten intake triggers reactions that damage the small intestine.
- Crohn’s disease: It’s a chronic inflammation of our gastrointestinal tract that affects nutrient absorption.
- Tropical Sprue: It’s a common condition in the tropics. It causes steatorrhea through damaging the intestinal cells, secondary to long-standing inflammation or infection.
- Short Bowel Syndrome: This condition arises after the surgical removal of the small bowel. In this, our body fails to absorb a sufficient amount of fat, as the surface area for absorption is reduced.
Infectious Causes of Steatorrhea:
- Whipple’s disease: This chronic bacterial infection of the small intestine damages our villi, leading to malabsorption.
- Small Intestinal Bacterial Overgrowth or SIBO: It’s a condition with excessive bacteria in the small intestine, which interferes with normal digestion.
- Giardiasis: It’s a parasitic infection from contaminated food or water, leading to malabsorption.
- HIV Enteropathy: In patients with HIV, the virus penetrates and destroys the cells of the small intestine, hampering fat absorption, causing greasy stools.
Drug-induced Causes:
Certain medications can affect how our bodies digest or absorb fat. These include:
- Orlistat: It’s a weight loss medication that acts by blocking the fat-digesting pancreatic enzymes.
- Cholestyramine: Doctors prescribe it when you have high cholesterol in your blood. It traps the bile salts, making them unavailable for fat digestion.
- Antibiotics such as Neomycin: These drugs indirectly cause malabsorption of fat through several mechanisms, such as disturbing gut flora, damaging intestinal cells, or promoting abnormal bacterial growth.
- Chronic laxative use: By speeding up the normal gut motility, these medications give fat less time to absorb, and can even destroy the intestinal cells.
How common is Steatorrhea?
Steatorrhea is a common symptom, but people often don’t report it out of shame, or it goes unnoticed due to the initial asymptomatic phase. Therefore, its exact prevalence is difficult to determine. However, scientists have somehow given an estimate from the prevalence of underlying causes.
For example, chronic pancreatitis is a frequent cause, with a prevalence of 42 per 100,000 cases every year in the US.2Yadav, D., Timmons, L., Benson, J. T., Dierkhising, R. A., & Chari, S. T. (2011). Incidence, prevalence, and survival of chronic pancreatitis: a population-based study. The American journal of gastroenterology, 106(12), 2192–2199. https://doi.org/10.1038/ajg.2011.328 Similarly, 1 in every 3000 births suffers from cystic fibrosis, and 85% of cystic fibrosis patients (mainly children) also develop Exocrine Pancreatic Insufficiency, hence steatorrhea.3Paranjape, S. M., & Mogayzel, P. J., Jr (2014). Cystic fibrosis. Pediatrics in review, 35(5), 194–205. https://doi.org/10.1542/pir.35-5-194 Another study indicates that around 78% of liver disease patients have fatty stools.4Williams, C. N., & Sidorov, J. J. (1971). Steatorrhea in patients with liver disease. Canadian Medical Association journal, 105(11), 1143–1154.
Also, steatorrhea is more common in developing countries due to a higher incidence of giardiasis and malnutrition-related conditions.
Symptoms of Steatorrhea
The symptoms of steatorrhea involve certain stool characteristics accompanied by symptoms of malabsorption or maldigestion, indicating corresponding underlying pathologies:
Stool Characteristics:
It is possible that initially, you might not have any symptoms at all. Later, your stool may exhibit the following characteristics:
- Bulky, greasy, and loose
- Clay-colored or pale
- Foul-swelling
- May float
- It may be hard to flush
- Presence of foam or oil droplets in the toilet bowl
Associated Symptoms:
These are often non-specific and include:
- Pain Abdomen
- Bloating
- Loose stools
- Weight loss
- Fatigue
Manifestations of the Underlying Cause:
You might exhibit some case-specific symptoms depending on the cause of your steatorrhea, such as:
- Jaundice and pruritis in the case of Primary Biliary cirrhosis or Primary Sclerosing Cholangitis
- Oral ulcers, dermatitis herpetiformis, and anemia if celiac disease is the underlying cause
- Frequent lung and sinus infections in patients with cystic fibrosis
Signs of fat-soluble vitamins Deficiency:
Since the digestion and/or absorption of fats is compromised in these patients, they often present with a deficiency of fat-soluble vitamins:
- Vitamin A deficiency: Dry eyes (Xerophthalmia), night blindness, skin problems
- Vitamin D deficiency: Bony pains, weakness, low mood
- Vitamin E deficiency: Peripheral neuropathy, brittleness of skin or nails
- Vitamin K deficiency: Abnormalities with clotting
Symptoms in Children:
Children often present with other manifestations such as:
- Growth retardation
- Delayed puberty
How do doctors diagnose Steatorrhea?
Doctors diagnose steatorrhea through a combination of clinical evaluation, lab tests, and imaging studies. The focus is on confirming the presence of fatty stools and then identifying the underlying cause.
Clinical Evaluation:
It starts with a thorough history, in which the doctor explores the characteristics of your poop, their duration, any accompanied symptoms and presence or absence of nutrient deficiency signs. He may also inquire about the medications you might be taking to rule out drug-induced causes of steatorrhea.
Then the doctor proceeds to an in-depth general physical examination, as well as an abdominal examination.
Lab Investigations:
These include qualitative and quantitative tests to confirm the presence of fat in stools.
Qualitative Fecal Fat Test
For this test, you give a stool sample, and the microbiologist examines it under the microscope using Sudan III staining to detect fat globules. A presence of more than 50 neutral fat globules and more than 100 fatty acid globules confirms steatorrhea
Quantitative Fecal Fat Test
This test measures the excretion of fat over 72 hours. Your healthcare provider will advise you to go on a high-fat diet for a given number of days. In the last three days, you will need to collect your stool samples. The lab technologists then examine these stool samples to calculate the Coefficient of Fat Absorption (CFA), i.e, how much amount of ingested fat is absorbed through the small intestine. A value above 92% indicates normal stool characteristics.5Lindkvist, B., Phillips, M. E., & Domínguez-Muñoz, J. E. (2015). Clinical, anthropometric, and laboratory nutritional markers of pancreatic exocrine insufficiency: Prevalence and diagnostic use. Pancreatology: official journal of the International Association of Pancreatology (IAP) … [et al.], 15(6), 589–597.https://doi.org/10.1016/j.pan.2015.07.001
Apart from this, your doctor may ask you to undergo these labs:
- D-xylose Test: Doctors ask you to drink a sugary solution, called D-xylose. Then they ask for a urine sample and evaluate it for the presence of D-xylose. If positive, the test indicates that pathology lies within the liver or pancreas, as D-xylose was perfectly absorbed from the small intestine and was excreted in urine. If negative, it means there is a problem with the small intestine.
- Fecal Elastase test: Doctors prescribe this test to rule out chronic pancreatitis. If fecal elastase in your stool sample is below the required threshold, it means you have exocrine pancreatic insufficiency (EPI).
Imaging & Endoscopy:
Your healthcare provider would ask you to get these done to find out which underlying disorder is causing steatorrhea.
- Plain X-ray Abdomen: To detect calcifications in case of chronic pancreatitis.
- CT/MRI Abdomen: To get a more detailed view of the pancreas, or look for ductal damage.
- Magnetic Resonance Cholangiopancreatography (MRCP): It’s a specialized form of MRI to assess the bile ducts and pancreatic ducts. It may reveal a beaded appearance in the case of Primary Sclerosing Cholangitis (PSC).6Fricker, Z. P., & Lichtenstein, D. R. (2019). Primary Sclerosing Cholangitis: A Concise Review of Diagnosis and Management. Digestive diseases and sciences, 64(3), 632–642. https://doi.org/10.1007/s10620-019-05484-y
- Endoscopic Retrograde Cholangiopancreatography (ERCP): It’s an invasive test that combines endoscopy and imaging to assess the pancreatic/biliary ducts. It is helpful in PSC and chronic pancreatitis.
- Duodenal Biopsy: Doctors use it to confirm celiac disease when blood tests come positive
- Colonoscopy / Workup for Inflammatory Bowel Disease (IBD): Doctors recommend it when PSC is diagnosed, as more than 80% of PSC patients also have IBD.
Other Investigations:
These may include lab tests to diagnose other conditions, such as:
- Tissue Transglutaminase IgA and Endomysial Antibodies for Celiac Disease.7Lebwohl, B., Sanders, D. S., & Green, P. H. R. (2018). Coeliac disease. Lancet (London, England), 391(10115), 70–81. https://doi.org/10.1016/S0140-6736(17)31796-8
- Liver Function Test, such as AST, ALT, GGT, to look for the presence and progression of underlying liver pathology.
- Anti-Mitochondrial Antibodies (AMA) for Primary Biliary Cirrhosis (PBC).8Bader, T. R., Beavers, K. L., & Semelka, R. C. (2003). MR imaging features of primary sclerosing cholangitis: patterns of cirrhosis in relationship to clinical severity of disease. Radiology, 226(3), 675–685. https://doi.org/10.1148/radiol.2263011623
- Glucose or Lactulose Breath Test: It’s a non-invasive screening test for SIBO.
- Stool PCR or antigen testing for Giardia.
- Small bowel biopsy for Whipple’s or tropical sprue.
- HIV testing, if clinically indicated.
Steatorrhea vs. Diarrhea
Steatorrhea and diarrhea are distinct gastrointestinal symptoms, but they are often confused due to overlapping features. Here’s how they differ:
| Feature | Steatorrhea | Diarrhea |
| Definition | Passage of fatty, greasy stools due to fat malabsorption | Increased frequency and liquidity of stools |
| Stool Appearance | Pale, bulky, foul-smelling, oily; may float and stick to the toilet bowl | Watery or loose; usually doesn’t contain fat |
| Cause | Fat malabsorption (e.g., pancreatic insufficiency, celiac disease) | Infection, IBS, IBD, medications, food intolerance |
| Fat Content | High fat content in stool | Normal or low fat content |
| Associated Symptoms | Weight loss, vitamin deficiencies, bloating | Cramping, urgency, dehydration |
| Stool Frequency | May or may not be increased | Usually increased |
| Diagnosis | Stool fat test, imaging, serology, endoscopy | Stool cultures, electrolyte panel, colonoscopy (if chronic) |
| Treatment Focus | Address fat malabsorption and its cause, dietary support | Rehydration, antidiarrheals, and treat the underlying cause |
How do doctors treat Steatorrhea?
Doctors focus on treating the underlying pathology, managing the symptoms, and offering nutritional support.
Addressing the underlying cause:
- Pancreatic Enzyme Replacement Therapy (PERT).9Clark, R., & Johnson, R. (2018). Malabsorption Syndromes. The Nursing clinics of North America, 53(3), 361–374. https://doi.org/10.1016/j.cnur.2018.05.001 and dietary recommendations for patients with EPI.
- Ursodeoxycholic acid in the case of PBC.10Santiago, P., Scheinberg, A. R., & Levy, C. (2018). Cholestatic liver diseases: new targets, new therapies. Therapeutic advances in gastroenterology, 11, 1756284818787400. https://doi.org/10.1177/1756284818787400
- Antibiotics like Rifaxamine for SIBO patients, Ceftriaxone for Whipple’s disease, anti-parasitic agents like Metronidazole for Giardiasis, and Anti-retroviral therapy (ART) in case of HIV Enteropathy.
- For drug-induced causes, doctors advise discontinuing the culprit drug and replacing it with one that doesn’t interfere with fat digestion.
- ERCP with stent dilation for those with PSC.
- Strictly gluten-free diet and counselling for celiac disease.
Symptomatic Management:
Your doctor may prescribe:
- Antidiarrheals such as loperamide to aid with loose stools.
- Probiotics to support gut flora, especially in SIBO patients, after an antibiotic treatment.
Nutritional Support:
- In steatorrhea, our bodies have a hard time absorbing fat-soluble vitamins like Vit A, D, E, and K. Therefore, you would need supplementation with these vitamins.
- Your nutritionist will advise you to consume medium-chain triglycerides (MCTs), which are absorbed easily and don’t require bile salts.
- Apart from this, you might need a high-protein, nutrient-rich diet to combat malnutrition
Dietary Recommendations for Steatorrhea
Dietary modifications depend on the underlying cause. If your steatorrhea is due to excessive consumption of fat, your diet should be devoid of the following fat-rich foods:
- Butter
- Coffee creamers
- Red meat
- Whole nuts
- Alchohol
- Coconut & palm oils
On the contrary, if the cause of your steatorrhea is a malabsorption of fats, then you need to consume a high-fat diet, with the replacement of pancreatic enzymes as required. In this case, make sure your diet consists of unsaturated fats, especially:
- Fish oil
- Nut butter
- Olive oil
- Avocados
Also, you can add sources of fat-soluble vitamins to your diet while continuing their oral supplementation. Some good dietary sources of these vitamins are:
- Carrots, butter, and fish oil for vitamin A
- Oily fish, egg yolks, and liver for vitamin D
- Almonds, peanuts, and sunflower oil for vitamin E
- Leafy green vegetables such as spinach and kale for vitamin K
Complications of Steatorrhea
If left untreated, steatorrhea can cause the following complications:
Malnutrition:
A long-standing loss of nutrients and fat can produce anemia, vitamin deficiencies, and cachexia. This is particularly alarming in children as they can fall into a state of impaired growth and abnormal cognitive development.
Bone Health Issues:
If calcium and vitamin D aren’t being absorbed well, your bones won’t be left with much mineral content, resulting in conditions like osteoporosis or osteopenia.
Neurological Symptoms:
These are common with a deficiency of vitamin E, vitamin B12(in case of ileal resection), and with Whipple’s disease. These include loss of sensation, muscle weakness, impaired balance and cognition, and vision problems.
What is the prognosis of Steatorrhea?
The prognosis of steatorrhea depends upon the underlying pathology.11Azer SA, Sankararaman S. Steatorrhea. [Updated 2023 May 16]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK541055/
- Patients with treatable diseases such as Giardiasis and Celiac disease have a good prognosis due to the reversible nature of these conditions.
- On the other hand, patients with cystic fibrosis, PBC, and PSC have a longer course and often a poor prognosis, due to the progressive nature of these etiologies.
- Positive prognostic indicators include compliance with dietary and medical therapy.
- On the contrary, persistent weight loss, severe malnutrition, or ongoing fat malabsorption may worsen outcomes.
Take-Home message
Steatorrhea is more than just fatty stools – it indicates serious underlying pathologies. Common causes are pancreatic insufficiency, liver conditions, celiac disease, and cystic fibrosis. Symptoms include greasy, bulky, hard-to-flush stools and associated symptoms according to the cause. Diagnosis involves a mix of clinical evaluation, stool fat tests, imaging, antibody testing, and sometimes endoscopy. Treatment is focused on addressing the underlying cause, advising dietary modifications, and managing other symptoms. Since it leads to malabsorption of essential nutrients, particularly fat-soluble vitamins (A, D, E, K), early recognition and intervention are crucial to prevent complications like malnutrition, bone disease, and immune dysfunction.
Refrences
- 1Paranjape, S. M., & Mogayzel, P. J., Jr (2014). Cystic fibrosis. Pediatrics in review, 35(5), 194–205. https://doi.org/10.1542/pir.35-5-194
- 2Yadav, D., Timmons, L., Benson, J. T., Dierkhising, R. A., & Chari, S. T. (2011). Incidence, prevalence, and survival of chronic pancreatitis: a population-based study. The American journal of gastroenterology, 106(12), 2192–2199. https://doi.org/10.1038/ajg.2011.328
- 3Paranjape, S. M., & Mogayzel, P. J., Jr (2014). Cystic fibrosis. Pediatrics in review, 35(5), 194–205. https://doi.org/10.1542/pir.35-5-194
- 4Williams, C. N., & Sidorov, J. J. (1971). Steatorrhea in patients with liver disease. Canadian Medical Association journal, 105(11), 1143–1154.
- 5Lindkvist, B., Phillips, M. E., & Domínguez-Muñoz, J. E. (2015). Clinical, anthropometric, and laboratory nutritional markers of pancreatic exocrine insufficiency: Prevalence and diagnostic use. Pancreatology: official journal of the International Association of Pancreatology (IAP) … [et al.], 15(6), 589–597.https://doi.org/10.1016/j.pan.2015.07.001
- 6Fricker, Z. P., & Lichtenstein, D. R. (2019). Primary Sclerosing Cholangitis: A Concise Review of Diagnosis and Management. Digestive diseases and sciences, 64(3), 632–642. https://doi.org/10.1007/s10620-019-05484-y
- 7Lebwohl, B., Sanders, D. S., & Green, P. H. R. (2018). Coeliac disease. Lancet (London, England), 391(10115), 70–81. https://doi.org/10.1016/S0140-6736(17)31796-8
- 8Bader, T. R., Beavers, K. L., & Semelka, R. C. (2003). MR imaging features of primary sclerosing cholangitis: patterns of cirrhosis in relationship to clinical severity of disease. Radiology, 226(3), 675–685. https://doi.org/10.1148/radiol.2263011623
- 9Clark, R., & Johnson, R. (2018). Malabsorption Syndromes. The Nursing clinics of North America, 53(3), 361–374. https://doi.org/10.1016/j.cnur.2018.05.001
- 10Santiago, P., Scheinberg, A. R., & Levy, C. (2018). Cholestatic liver diseases: new targets, new therapies. Therapeutic advances in gastroenterology, 11, 1756284818787400. https://doi.org/10.1177/1756284818787400
- 11Azer SA, Sankararaman S. Steatorrhea. [Updated 2023 May 16]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK541055/

