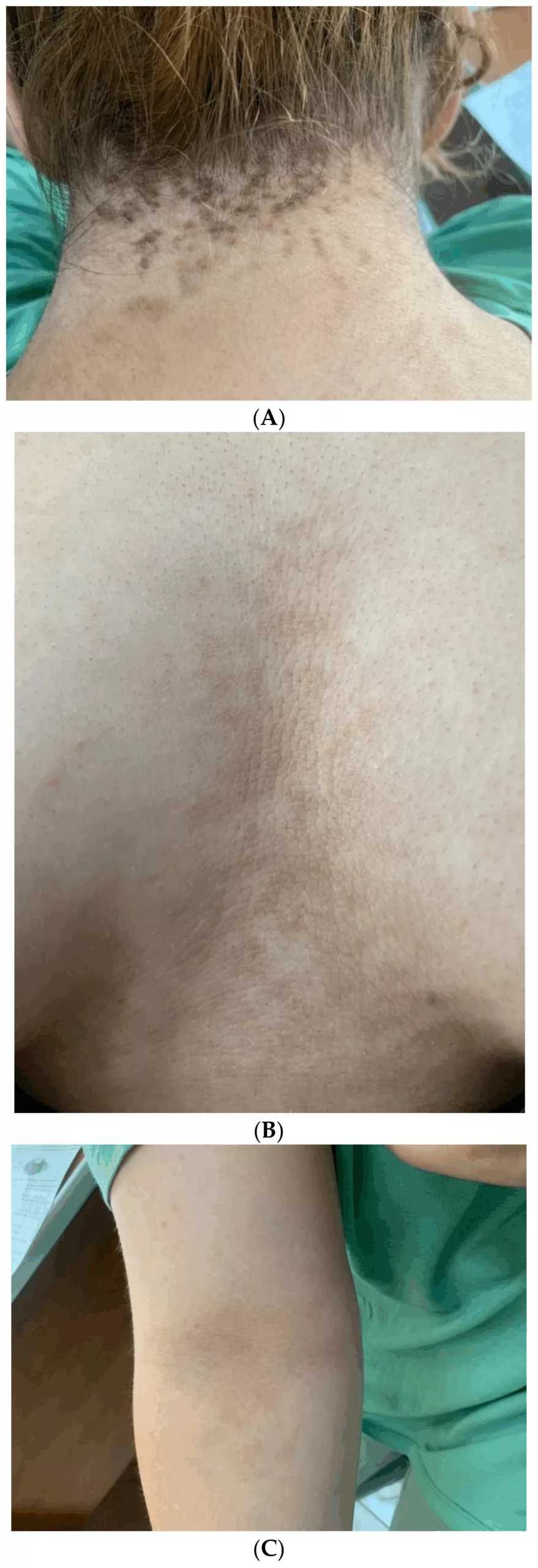
Acanthosis Nigricans (AN) is a skin condition characterized by dark, velvety, thickened patches or plaques, typically appearing in body folds and creases. Common sites include the axillae (armpits), posterior and lateral neck folds, antecubital fossae (inner elbows), popliteal fossae (behind the knees), inframammary areas, and the groin. These skin changes usually develop gradually and may be accompanied by a roughened or papillomatous texture, occasional odor, or the formation of skin tags (acrochordons).1Das, A., et al., Acanthosis nigricans: a review. Journal of Cosmetic Dermatology, 2020. 19(8): p. 1857-1865. Dr. Paul Gerson Unna introduced the term AN, and the first case report was published by Dr. Sigmund Pollitzer.2Pollitzer, S., Acanthosis nigricans: a symptom of a disorder of the abdominal sympathetic. Journal of the American Medical Association, 1909. 53(17): p. 1369-1373.
It is not harmful itself, but it is frequently associated with underlying health issues, particularly insulin resistance and obesity. It can serve as an essential marker for conditions like type 2 diabetes and metabolic syndrome. In rare cases, malignant acanthosis nigricans may occur and is most often associated with intra-abdominal malignancies, particularly gastric adenocarcinoma. Certain medications (e.g., nicotinic acid, corticosteroids, oral contraceptives) and endocrine disorders (e.g., polycystic ovary syndrome, Cushing’s disease, hypothyroidism) may also trigger AN.3Shiana, et al., A Comprehensive Review of Acanthosis Nigricans: Pathogenesis, Clinical Manifestation and Management. Recent Advances in Inflammation & Allergy Drug Discovery, 2024.
Causes of Acanthosis Nigricans
Acanthosis nigricans (AN) arises from a variety of underlying causes, and its pathogenesis typically involves stimulation of epidermal keratinocytes and dermal fibroblast proliferation. The most common etiologies include:
- Hereditary Variants: They may be associated with fibroblast growth factor defects.
- Insulin Resistance (Most Common Cause):
Elevated circulating insulin levels, as seen in obesity, type 2 diabetes, and polycystic ovary syndrome, stimulate keratinocyte proliferation. This occurs when excess insulin binds to insulin-like growth factor-1 (IGF-1) receptors on keratinocytes. At high concentrations, insulin can displace IGF-1 from its binding proteins, increasing free IGF-1 levels, which promotes epidermal and dermal proliferation. - Malignancy-Associated AN (Paraneoplastic):
This rare but important variant is most commonly linked to gastric adenocarcinoma and other intra-abdominal malignancies. The proposed mechanism involves tumor-secreted growth factors such as transforming growth factor-alpha (TGF-α), which activate epidermal growth factor receptors (EGFRs) in the skin, causing rapid and extensive skin changes.
Types of Acanthosis Nigricans
The types of AN were based on their underlying etiology. Types of AN include:
Obesity-Associated Acanthosis Nigricans:
This is one of the most common forms of AN and was historically referred to as “pseudoacanthosis nigricans.” Obesity, which is frequently linked with insulin resistance, plays a central role in its development. Management primarily involves lifestyle changes, dietary interventions, medications, and weight reduction strategies.4Ng, H.Y., Acanthosis nigricans in obese adolescents: prevalence, impact, and management challenges. Adolescent health, medicine and therapeutics, 2016: p. 1-10.
Familial Acanthosis Nigricans:
This rare form appears in childhood or at birth and follows an autosomal dominant inheritance pattern. Mutations in the fibroblast growth factor receptor 3 (FGFR3) gene are usually responsible.5Fukuchi, K., et al., Familial acanthosis nigricans with p. K650T FGFR 3 mutation. The Journal of Dermatology, 2018. 45(2): p. 207-210.
Medication-Associated Acanthosis Nigricans:
The medications linked with AN include:
- Systemic glucocorticoids
- Nicotinic acid
- Diethylstilbestrol
- Growth hormone therapy
- Combined oral contraceptive pill
- Estrogen
- Injected insulin
- Niacin
- Protease inhibitors
AN usually resolves when you stop using the offending medications.
Endocrine Dysfunction Associated with AN:
This form is associated with underlying endocrine disorders, such as insulin resistance, polycystic ovary syndrome (PCOS), diabetes mellitus, and hypoandrogenism. It tends to have a slower onset and milder skin involvement, often in obese individuals.
Unilateral Acanthosis Nigricans:
The other name for unilateral AN is nevoid AN. This rare variant is inherited in an autosomal dominant pattern and typically affects only one side of the body. It can manifest at any age.
Autoimmune Acanthosis Nigricans:
This type is linked with autoimmune disorders, including systemic lupus erythematosus (SLE), scleroderma, Hashimoto’s thyroiditis, and Sjögren’s syndrome.6Kondo, Y., et al., A case of generalized acanthosis nigricans with positive lupus erythematosus-related autoantibodies and antimicrosomal antibody: autoimmune acanthosis nigricans. Case Reports in Dermatology, 2012. 4(1): p. 85-91.
Malignant AN Syndrome:
This aggressive form of AN is often associated with internal malignancies, particularly gastrointestinal adenocarcinomas and genitourinary cancers. It presents with a sudden onset and may be accompanied by additional features such as skin tags, “tripe palms,” and multiple seborrheic keratoses.
Acral Acanthotic Anomaly:
This variant presents with hyperpigmentation limited to areas like the knuckles, elbows, knees, and the dorsal surfaces of the feet. It is more common in individuals with darker skin tones.7Anand, V., et al., Acral acanthosis nigricans (acral acanthotic anomaly). Indian Dermatology Online Journal, 2014. 5(Suppl 2): p. S140-S141.
Symptoms of Acanthosis Nigricans
The clinical features of AN include:
Dark, Thickened & Velvety Skin:
The gradual development of dark, thickened, and velvety patches or plaques of the skin is the hallmark of AN.
Symmetrical Distribution:
These body changes are symmetric and commonly affect these areas:
- The neck (especially the nape and sides)
- Armpits
- Elbows
- Knees
- Knuckles
- Belly button
- Under the breast
- Groin
Other Possible Locations
In more severe or atypical cases, lesions can also affect the:
- Face, lips, and eyelids
- Palms and soles
- Mucosal surfaces (particularly in malignancy-associated AN)
- Areola and nipples in women
- Perineum and vulva
Associated Symptoms:
- Odor: Thickened plaques may emit an unpleasant smell due to moisture and bacterial colonization.
- Itching: More commonly seen in malignant cases.
- Maceration: Moisture buildup in body folds may lead to softening and increased susceptibility to secondary infections.
- Skin Tags: These benign outgrowths may appear near the affected regions.
- Rapid Onset: A sudden appearance, particularly in adults, can signal an underlying malignancy and requires urgent evaluation.
- Rare Associations: Nail changes and conjunctival involvement have occasionally been reported.8Rawla, E.K.H.M.F.B.P., Acanthosis Nigricans. 2025.
Diagnosis of Acanthosis Nigricans
Evaluation and diagnosis of this condition include:
Clinical Assessment
The diagnosis of Acanthosis Nigricans is primarily clinical. A dermatologist or healthcare provider typically identifies it based on the presence of hallmark features: dark, velvety, hyperkeratotic plaques commonly located in intertriginous areas. A detailed medical history and physical examination are essential to evaluate associated risk factors such as obesity, insulin resistance, endocrine disorders, and medication use.

Dermoscopy
Dermoscopy may support diagnosis by revealing characteristic patterns such as exaggerated skin markings and pigmentary network changes.
Skin Biopsy
A skin biopsy may be performed to confirm the diagnosis or rule out other skin conditions if the presentation is atypical.Histological findings typically include:
- Basal layer hyperpigmentation
- Hyperkeratosis
- Papillomatosis
- Mild acanthosis
Laboratory Investigations:
Lab tests are essential when AN appears abruptly, is extensive, or is seen in a non-obese individual:
- Fasting glucose and insulin levels: to assess insulin resistance or diabetes
- Hemoglobin A1c (if not already known)
- Thyroid function tests: if hypothyroidism is suspected
- Hormonal panel: including androgens in females with PCOS features like hirsutism
- Cancer screening (in older patients with sudden onset or extensive disease): e.g., abdominal imaging, endoscopy, or tumor markers based on clinical suspicion
Treatment & Management of Acanthosis Nigricans
AN is not treatable, but it can fade over time by treating the underlying cause.
Treating the Underlying Cause:
- Obesity is the most common cause of AN, so significant weight loss can lead to partial or complete resolution of skin changes.
- Nutritional counseling and a healthy, balanced diet are recommended.
- Improving blood sugar control through diet, exercise, and medications (e.g., metformin, rosiglitazone) can improve or resolve AN.
- If AN is linked to hormonal imbalances (e.g., PCOS), treating the underlying endocrine disorder may help.
- If due to medications (e.g., corticosteroids, nicotinic acid, estrogen), discontinuation or substitution may lead to regression.
- In rare cases of internal malignancies, surgical removal of the tumor or cancer treatment can resolve the skin lesions.
Skin-Directed Treatments:
Some patients seek cosmetic improvement. The options include:
Topical Treatments
- Retinoids (tretinoin 0.1% gel)
- Vitamin D analogs (calcipotriol 0.005%)9Rawla, E.K.H.M.F.B.P., Acanthosis Nigricans. 2025.
- Ammonium lactate creams
- Alpha-hydroxy acids (e.g., lactic acid, glycolic acid)
- Keratolytics (salicylic acid)
- Topical metformin (investigational in some studies)
Systemic treatments (selective cases):
- Etretinate (oral retinoid; rarely used now due to side effects)
- Oral metformin, especially in insulin-resistant individuals
Procedural Treatments
Cosmetic treatments have been tried to include:
- Dermabrasion
- Laser therapy
- Chemical peels (e.g., trichloroacetic acid)
Cosmetic treatments can only improve the appearance of the condition, but can not cure the underlying causes.
Self-Care & Lifestyle Measures:
- lean the affected areas gently with mild soap
- Avoid harsh scrubbing or exfoliants
- Avoid bleaching creams
- Maintain a healthy diet
- Engage in regular physical activity
- Monitor for sudden or widespread changes in skin10Rawla, E.K.H.M.F.B.P., Acanthosis Nigricans. 2025.
Prognosis
Patients with the benign form of AN have no or only a few skin complications and a good prognosis. They have the potential for resolution with treatment. The prognosis in patients with the malignant form of AN is poor, as the malignancy is usually advanced at the time of diagnosis.
Acanthosis Nigricans vs. Hyperpigmentation
AN and hyperpigmentation both involve the darkening of the skin but differ significantly in their causes, appearance, and locations. The key differences are summarized in the table.
| Features | AN | Hyperpigmentation |
| Causes |
|
|
| Symptoms | Sun-exposed areas such as the face, hands, or anywhere on the skin | Dark patches without thickening |
| Locations | Generally, the body folds | Sun-exposed areas such as face, hands, or anywhere on the skin |
| Associated conditions |
|
|
| Treatment |
|
|
Conclusion
AN is a common skin disorder. Recognizing AN is clinically significant, as addressing the underlying cause can often lead to improvement of the skin changes and may help identify and manage serious systemic diseases. Any new, unexplained, or rapidly developing skin changes should prompt medical evaluation, especially if accompanied by other systemic symptoms or risk factors for diabetes or malignancy.
Refrences
- 1Das, A., et al., Acanthosis nigricans: a review. Journal of Cosmetic Dermatology, 2020. 19(8): p. 1857-1865.
- 2Pollitzer, S., Acanthosis nigricans: a symptom of a disorder of the abdominal sympathetic. Journal of the American Medical Association, 1909. 53(17): p. 1369-1373.
- 3Shiana, et al., A Comprehensive Review of Acanthosis Nigricans: Pathogenesis, Clinical Manifestation and Management. Recent Advances in Inflammation & Allergy Drug Discovery, 2024.
- 4Ng, H.Y., Acanthosis nigricans in obese adolescents: prevalence, impact, and management challenges. Adolescent health, medicine and therapeutics, 2016: p. 1-10.
- 5Fukuchi, K., et al., Familial acanthosis nigricans with p. K650T FGFR 3 mutation. The Journal of Dermatology, 2018. 45(2): p. 207-210.
- 6Kondo, Y., et al., A case of generalized acanthosis nigricans with positive lupus erythematosus-related autoantibodies and antimicrosomal antibody: autoimmune acanthosis nigricans. Case Reports in Dermatology, 2012. 4(1): p. 85-91.
- 7Anand, V., et al., Acral acanthosis nigricans (acral acanthotic anomaly). Indian Dermatology Online Journal, 2014. 5(Suppl 2): p. S140-S141.
- 8Rawla, E.K.H.M.F.B.P., Acanthosis Nigricans. 2025.
- 9Rawla, E.K.H.M.F.B.P., Acanthosis Nigricans. 2025.
- 10Rawla, E.K.H.M.F.B.P., Acanthosis Nigricans. 2025.

