Atelectasis is a condition where part or all of a lung collapses, leading to reduced lung volume and impaired gas exchange. This means the alveoli, which are tiny air sacs responsible for oxygenating the blood, cannot properly inflate. This condition is commonly associated with airway blockages, reduced airflow, or external pressure on the lungs. Conditions like cystic fibrosis, lung infections, tumors, or chest injuries can cause it. However, it most frequently occurs after surgery due to the effects of anesthesia, which can reduce lung expansion. Inhaled foreign objects can also obstruct airways, leading to atelectasis.1Carlsen, K. H., Crowley, S., & Smevik, B. (2019). Atelectasis. In Kendig’s Disorders of the Respiratory Tract in Children (pp. 1027-1033). Elsevier.
What is Atelectasis?
Atelectasis (a-teh-lek-tuh-sis) is a lung disease that occurs when one or more parts of the lungs collapse. It especially affects the tiny air sacs called alveoli.
When you inhale, air fills the alveoli, allowing oxygen to move into the bloodstream while carbon dioxide is expelled. In atelectasis, the alveoli fail to fully inflate due to insufficient airflow or external compression. This condition can affect a small portion of the lung (segmental atelectasis) or an entire lobe or lung. If enough lung tissue is involved, it can result in hypoxemia (low blood oxygen levels) and compromise overall respiratory function.2Carlsen, K. H., Crowley, S., & Smevik, B. (2019). Atelectasis. In Kendig’s Disorders of the Respiratory Tract in Children (pp. 1027-1033). Elsevier.
It can sometimes be misdiagnosed as pneumonia, particularly when pulmonary opacification (cloudiness on imaging) is minimal or absent. This overlap in radiographic appearance can lead to diagnostic challenges. Treatment is generally straightforward but depends on the underlying cause and the timing of intervention. Management strategies may include physiotherapy, bronchoscopy, or addressing the underlying obstruction to re-expand the collapsed lung tissue.3Hedenstierna, G., & Rothen, H. U. (2000). Atelectasis formation during anesthesia: causes and measures to prevent it. Journal of Clinical Monitoring and Computing, 16(5-6), 329–335. https://doi.org/10.1023/a:1011491231934
Symptoms of Atelectasis
This condition often does not cause noticeable symptoms, especially when only a small portion of the lung is affected. However, when larger areas are involved, it can lead to symptoms due to reduced oxygen levels in the blood (hypoxemia).4Woodring, J. H., & Reed, J. C. (1996). Types and mechanisms of pulmonary atelectasis. Journal of Thoracic Imaging, 11(2), 92-108.
- Face trouble while breathing/shortness of breath (Dyspnea)
- Tachypnea (rapid breathing)
- Coughing
- Chest pain
- High heart rate
- Bluish skin or lips (Cyanosis)
- Wheezing5Woodring, J. H., & Reed, J. C. (1996). Types and mechanisms of pulmonary atelectasis. Journal of Thoracic Imaging, 11(2), 92-108.
Patients with underlying conditions like COPD are more prone to these symptoms due to impaired lung function.
Cause of Atelectasis
This condition can occur due to blocked airways (obstructive atelectasis) or external pressure on the lung (non-obstructive atelectasis). Obstructive atelectasis results from airway obstructions like mucus plugs, tumors, or inhaled foreign objects, leading to the collapse of alveoli as air is absorbed but not replaced. Patients with chronic obstructive pulmonary disease (COPD) are at higher risk due to impaired lung function. Non-obstructive atelectasis includes compression from pleural effusions, pneumothorax, or abdominal distension. Surfactant-related issues, scarring from infections like tuberculosis, and postoperative factors like anesthesia also contribute to atelectasis.6Hedenstierna, G., & Rothen, H. U. (2000). Atelectasis formation during anesthesia: causes and measures to prevent it. Journal of Clinical Monitoring and Computing, 16(5-6), 329–335. https://doi.org/10.1023/a:1011491231934
Special Cases of Atelectasis
-
Rounded Atelectasis:
Typically associated with exposure to asbestos, this form involves localized lung collapse accompanied by fibrosis.
-
Middle Lobe Syndrome:
Chronic atelectasis of the right middle lobe is often caused by external compression or inflammation. It is more common in individuals with underlying lung diseases.
Additional Contributing Factors
Certain conditions and events can further increase the risk of atelectasis:
- Cancerous tumors in your airway
- Lung scarring
- Non-cancerous (benign) growths
- Injury (Chest trauma)
- Underlying diseases: This lung condition can be brought on by illnesses such as pneumonia, COVID-19, acute respiratory distress syndrome (ARDS), and chronic obstructive pulmonary disease (COPD).7Hedenstierna, G., & Rothen, H. U. (2000). Atelectasis formation during anesthesia: causes and measures to prevent it. Journal of Clinical Monitoring and Computing, 16(5-6), 329–335. https://doi.org/10.1023/a:1011491231934
Risk Factors for Atelectasis
Certain individuals are at a higher risk of developing atelectasis due to specific conditions, behaviors, or medical interventions. The following factors can increase susceptibility:
Respiratory and Lung Conditions
- Chronic Respiratory Diseases: Conditions like chronic obstructive pulmonary disease (COPD), asthma, cystic fibrosis, or bronchiectasis can impair lung function and increase mucus buildup, leading to airway blockages.
- Prolonged Oxygen Use: High-flow oxygen therapy can sometimes lead to alveolar collapse.
- Smoking: Smoking damages the lungs and reduces their ability to clear mucus effectively.
Neuromuscular and Systemic Conditions
- Neuromuscular Disorders: Diseases that weaken muscles and nerves, such as muscular dystrophy or spinal cord injuries, can impair the ability to breathe deeply or cough effectively.
- Swallowing Impairments: Conditions or injuries that impair swallowing can increase the risk of aspiration, potentially blocking airways.
Medical Interventions and Procedures
- Surgery on the Chest or Abdomen: Procedures requiring general anesthesia, especially for abdominal or thoracic surgeries, can reduce lung expansion and increase mucus retention.
- General Anesthesia: Recent use of anesthesia affects the ability to take deep breaths, increasing the risk of postoperative atelectasis.
- Mechanical Ventilation: Extended mechanical ventilation can contribute to alveolar collapse, particularly in trauma or ICU settings.
Physical and Lifestyle Factors
- Older Age: Age-related changes in lung elasticity and immune response make older adults more susceptible.
- Prolonged Bed Rest: Immobility reduces lung expansion and increases mucus accumulation.
- Obesity: Excess weight can restrict diaphragm movement, reducing lung expansion.
- Rib Fractures or Chest Injuries: Severe pain from chest injuries can inhibit deep breathing, leading to partial lung collapse.
- Smoke Exposure: Environmental or occupational exposure to smoke can irritate the lungs and contribute to atelectasis development.8Hongrattana, G., Reungjui, P., Tumsatan, P., & Ubolsakka-Jones, C. (2019). Incidence and risk factors of pulmonary atelectasis in mechanically ventilated trauma patients in ICU: a prospective study. JBI Evidence Implementation, 17(1), 44-52.
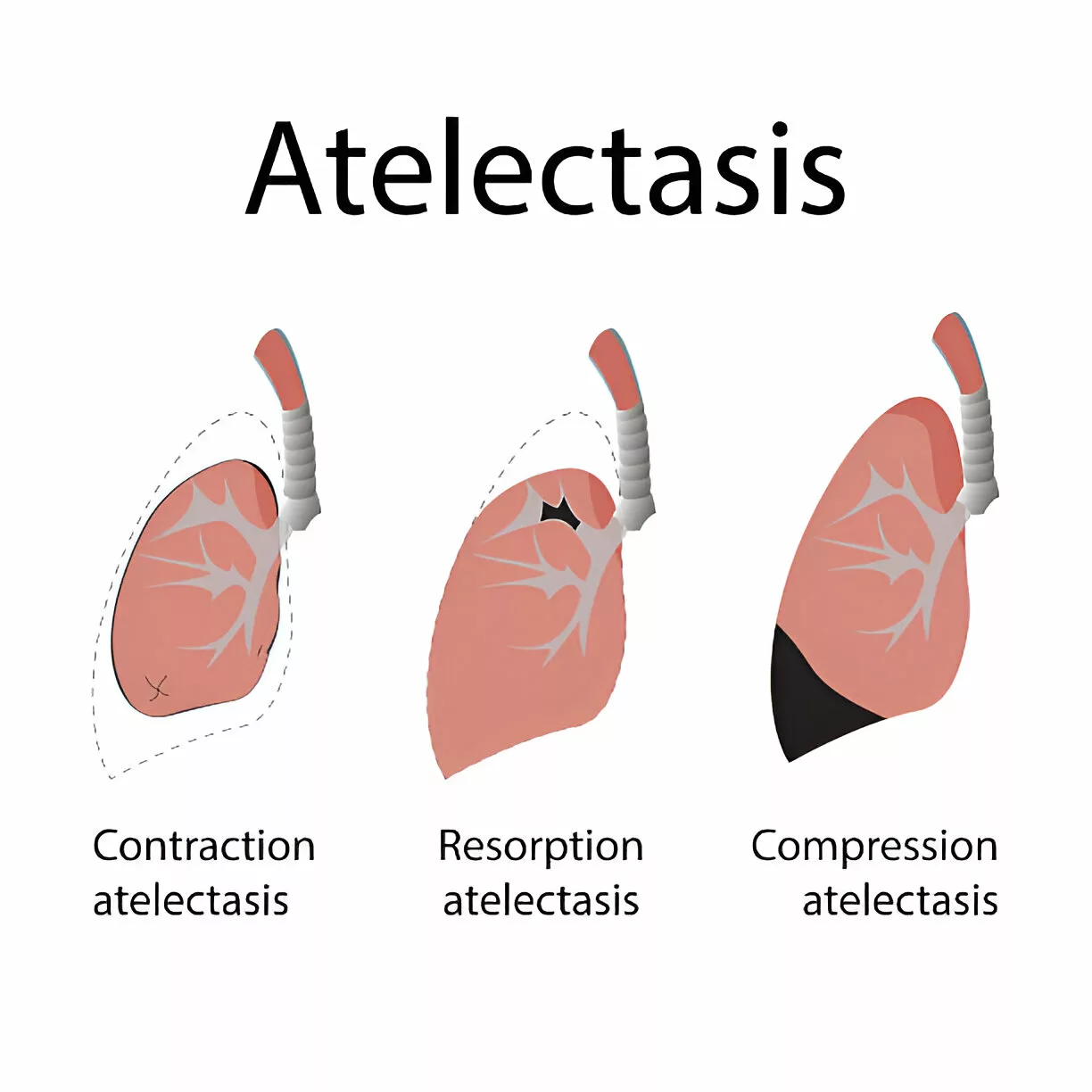
Types of Atelectasis
Three significant types are contraction, compressive, and resorptive (obstructive).
Compressive Atelectasis:
When your lung collapses due to external forces such as fluid, air, blood, or a tumor pressing against it, you have compressive atelectasis.9Hedenstierna, G., & Edmark, L. (2010). Mechanisms of atelectasis in the perioperative period. Best Practice & Research Clinical Anaesthesiology, 24(2), 157-169.
Obstructive/Resorptive Atherosclerosis:
This type occurs when air cannot enter the alveoli due to an obstruction like a tumor, mucus plug, or an inhaled foreign object. Surgery, especially under anesthesia, also contributes to this condition by causing shallow breathing, reducing lung expansion, and allowing mucus buildup, leading to alveolar collapse.10Woodring, J. H., & Reed, J. C. (1996). Types and mechanisms of pulmonary atelectasis. Journal of Thoracic Imaging, 11(2), 92-108.
Contraction Atelectasis:
This type results from lung scarring or fibrosis. Alveolar damage prevents the alveoli from expanding fully.
Other forms of Atelectasis:
Patchy Atelectasis
Acute respiratory distress syndrome (ARDS) patients and babies, especially those born prematurely, may have patchy atelectasis, a rare form of atelectasis. Insufficient levels of surfactant, a protein in the lungs that prevents them from collapsing, result in patchy atelectasis.11Stark, P., Muller, N. L., & Finlay, G. (2020). Atelectasis: Types and pathogenesis in adults. U: UpToDate, Muller NL ed. UpToDate [Internet]. Waltham, MA: UpToDate.
Other forms of atelectasis that specify the location, appearance, or severity of the collapse include:
- Subsegmental
- Rounded (also called folded lung)
- Gravity-dependent atelectasis
- Adhesive atelectasis
- Linear atelectasis
- Basilar atelectasis
- Dependent atelectasis
- Acceleration atelectasis12Woodring, J. H., & Reed, J. C. (1996). Types and mechanisms of pulmonary atelectasis. Journal of Thoracic Imaging, 11(2), 92-108.
How is Atelectasis Diagnosed?
This is diagnosed through a combination of physical exams, imaging tests, and clinical history.
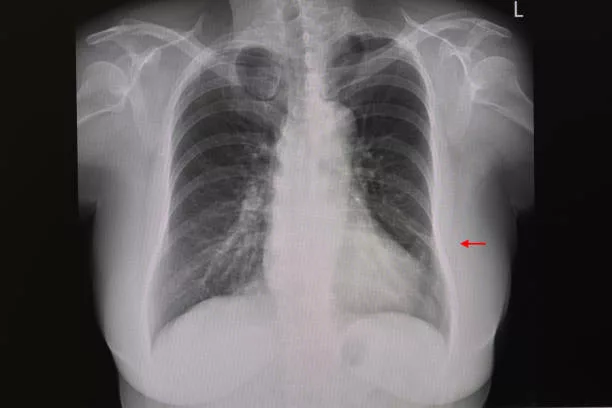
X-ray
The first test to diagnose this condition is an X-ray of the chest (a picture of your lungs). If more detailed images are needed, your healthcare professional may utilize a computed tomography (CT) scan.
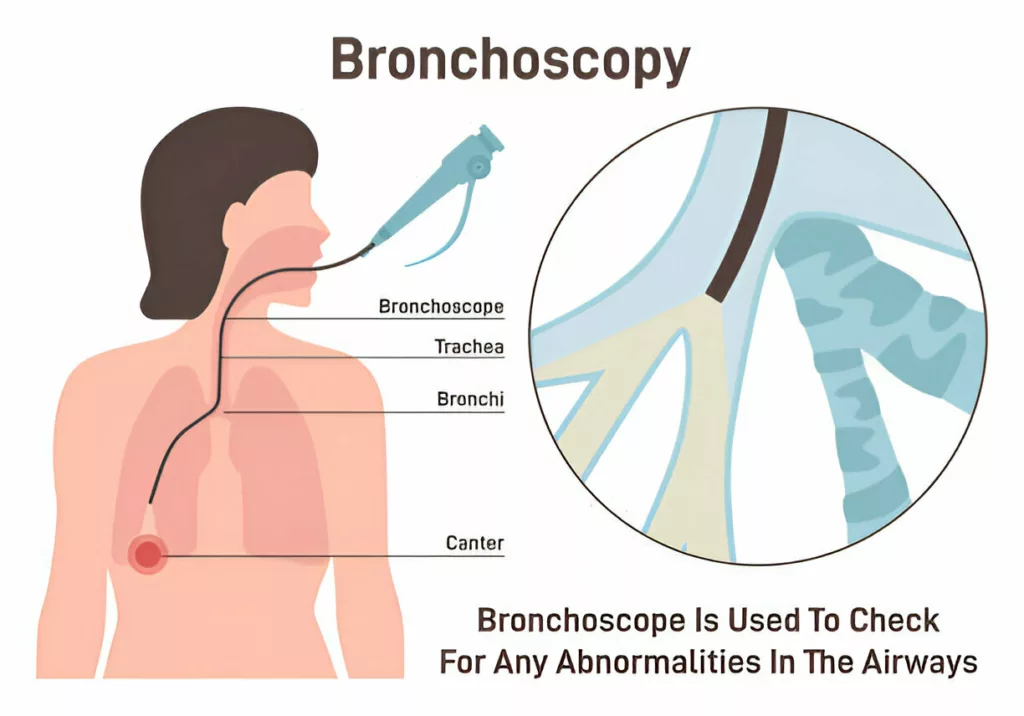
Bronchoscopy
In certain situations, your doctor may perform a bronchoscopy, a procedure in which a tiny camera attached to a tube down your throat looks inside your lungs. During the procedure, blockages may be removed.
Oximetry or Blood Gas Test:
These help to measure how much oxygen is getting into the blood.13Peroni, D. G., & Boner, A. L. (2000). Atelectasis: mechanisms, diagnosis and management. Pediatric respiratory reviews, 1(3), 274-278.
Treatment of Atelectasis
The treatment plan depends on the underlying cause, severity, and patient’s overall condition. While many cases can be resolved on their own with careful monitoring, specific interventions may be necessary to promote lung re-expansion and clear obstructions.14Peroni, D. G., & Boner, A. L. (2000). Atelectasis: mechanisms, diagnosis and management. Pediatric respiratory reviews, 1(3), 274-278. Possible therapies include:
Monitoring & Assessment:
In many cases, especially when this condition is mild or occurs postoperatively, careful monitoring may be sufficient. Healthcare professionals will assess the patient’s respiratory status and may recommend interventions based on clinical findings.
Airway Clearance Techniques:
-
Chest Physiotherapy:
Techniques like deep-breathing exercises, postural drainage, and chest percussion help re-expand collapsed lung areas and clear mucus.
-
Deep-Breathing Exercises:
Using an incentive spirometer can improve lung function and promote alveolar expansion.
-
Body Positioning:
Postural drainage techniques position the body to encourage mucus drainage.
-
Chest Tap
Percussion involves tapping the chest over collapsed areas to dislodge mucus. Devices like handheld instruments or vibrating vests may enhance this process.
Breathing Treatment:
A continuous positive airway pressure (CPAP) machine or breathing tube. It may help people who have low oxygen levels (also called hypoxemia) or are too weak to cough after surgery.15Carlsen, K. H., Crowley, S., & Smevik, B. (2019). Atelectasis. In Kendig’s Disorders of the Respiratory Tract in Children (pp. 1027-1033). Elsevier.16Zhao, Y., Zheng, R., Xiang, W., Ning, D., & Li, Z. (2021). Systematic review and meta-analysis on perioperative intervention to prevent postoperative atelectasis complications after thoracic surgery. Annals of Palliative Medicine, 10(10), 107260734-107210734.
Many studies have shown numerous techniques like PEEP (positive end-expiratory pressure) and arterial oxygenation, but they have not greatly improved atelectasis. The lungs rapidly reopened when the PEEP methodology was applied, which works on an airway pressure of 40 cm2 (H2O) and holds it for 7-8 seconds to help reopen the lungs.17Zhao, Y., Zheng, R., Xiang, W., Ning, D., & Li, Z. (2021). Systematic review and meta-analysis on perioperative intervention to prevent postoperative atelectasis complications after thoracic surgery. Annals of Palliative Medicine, 10(10), 107260734-107210734.
Bronchoscopy
A flexible tube is inserted into the airway to remove blockages like mucus plugs or foreign objects. It’s also used to obtain samples if a tumor is suspected.
Suctioning
Mucus suctioning is helpful in cases where patients cannot clear their airways on their own due to weakness or anesthesia effects.
Surgical Management:
In some rare cases, you may require surgery to remove the blockage and repair the structural issues of the lungs. If atelectasis is caused by a tumor, treatment may include reducing or removing the tumor during a bronchoscopy, which may need surgery. Other cancer therapies, such radiation or chemotherapy may or may not be necessary.
Prevention
Some strategies to lower the chance include:
- Perform regular deep-breathing exercises to maintain proper lung function.
- Stop smoking to improve lung health, enhance the respiratory tract’s efficiency, and reduce mucus buildup.
- Get vaccinated against respiratory infections, such as pneumonia and influenza, to protect lung function.
- Follow your doctor’s post-surgery instructions, including getting up and moving around, practicing breathing techniques, and using an incentive spirometer.
- Address any underlying conditions contributing to atelectasis as directed by your healthcare provider.
- Keep small objects out of toddlers’ reach to prevent accidental inhalation.18Rothen, H. U., Sporre, B., Engberg, G., Wegenius, G., Reber, A., & Hedenstierna, G. (1995). Prevention of atelectasis during general anesthesia. The Lancet, 345(8962), 1387-1391.
Outlook / Prognosis
The prognosis for varies depending on the underlying cause. In most cases, the lungs reopen and function normally after treatment. However, in severe or prolonged cases, permanent lung damage may occur.19 Zhao, Y., Zheng, R., Xiang, W., Ning, D., & Li, Z. (2021). Systematic review and meta-analysis on perioperative intervention to prevent postoperative atelectasis complications after thoracic surgery. Annals of Palliative Medicine, 10(10), 107260734-107210734.
Complications of Atelectasis
If left untreated, it can result in serious complications, including:
- Fluid accumulation in the lungs.
- Pneumonia: due to prolonged lung collapse and mucus retention.
- Respiratory failure: from inadequate oxygen exchange.
- Hypoxemia or reduced oxygen levels in the blood.20Zhao, Y., Zheng, R., Xiang, W., Ning, D., & Li, Z. (2021). Systematic review and meta-analysis on perioperative intervention to prevent postoperative atelectasis complications after thoracic surgery. Annals of Palliative Medicine, 10(10), 107260734-107210734.
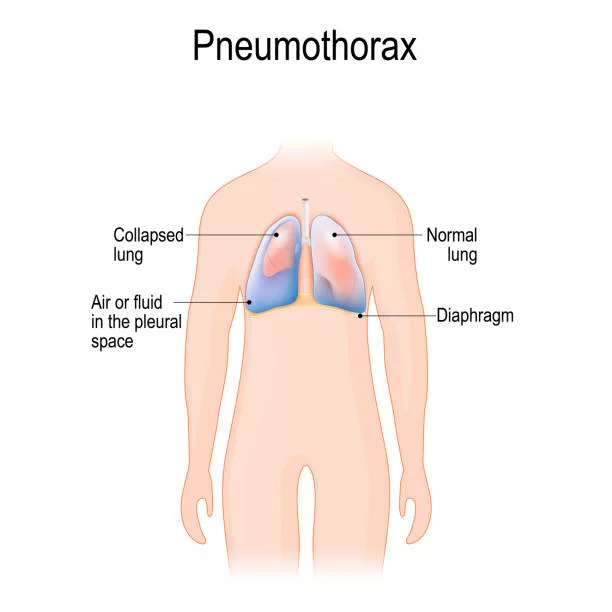
Atelectasis Vs. Pneumothorax
Pneumothorax and atelectasis are distinct lung conditions with opposite mechanisms. Atelectasis involves the partial or complete collapse of lung tissue due to obstruction or pressure, preventing proper air exchange in the affected area. In contrast, Pneumothorax occurs when air leaks into the pleural space (the area between the lung and chest wall), causing lung collapse due to increased pressure. Symptoms of pneumothorax may include sharp chest pain, shortness of breath, and rapid heart rate.21Boccatonda, A., Primomo, G., Cocco, G., D’Ardes, D., Marinari, S., Montanari, M., … & Schiavone, C. (2021). Not all abolished lung sliding are pneumothorax: the case of a particular lung atelectasis. Journal of Ultrasound, 24, 519-523.
Wrap up
This condition occurs when the alveoli (tiny sacs) in your lungs can’t inflate properly, causing either a partial or complete collapse of your lungs. It may cause symptoms including shortness of breath, chest pain, and rapid heart rate. Under the doctor’s supervision, it can be treated and may even be resolved by itself. However, not being treated can cause more health complications. Get medical assistance right away if you have any difficulty breathing, especially after the surgery.
Refrences
- 1Carlsen, K. H., Crowley, S., & Smevik, B. (2019). Atelectasis. In Kendig’s Disorders of the Respiratory Tract in Children (pp. 1027-1033). Elsevier.
- 2Carlsen, K. H., Crowley, S., & Smevik, B. (2019). Atelectasis. In Kendig’s Disorders of the Respiratory Tract in Children (pp. 1027-1033). Elsevier.
- 3Hedenstierna, G., & Rothen, H. U. (2000). Atelectasis formation during anesthesia: causes and measures to prevent it. Journal of Clinical Monitoring and Computing, 16(5-6), 329–335. https://doi.org/10.1023/a:1011491231934
- 4Woodring, J. H., & Reed, J. C. (1996). Types and mechanisms of pulmonary atelectasis. Journal of Thoracic Imaging, 11(2), 92-108.
- 5Woodring, J. H., & Reed, J. C. (1996). Types and mechanisms of pulmonary atelectasis. Journal of Thoracic Imaging, 11(2), 92-108.
- 6Hedenstierna, G., & Rothen, H. U. (2000). Atelectasis formation during anesthesia: causes and measures to prevent it. Journal of Clinical Monitoring and Computing, 16(5-6), 329–335. https://doi.org/10.1023/a:1011491231934
- 7Hedenstierna, G., & Rothen, H. U. (2000). Atelectasis formation during anesthesia: causes and measures to prevent it. Journal of Clinical Monitoring and Computing, 16(5-6), 329–335. https://doi.org/10.1023/a:1011491231934
- 8Hongrattana, G., Reungjui, P., Tumsatan, P., & Ubolsakka-Jones, C. (2019). Incidence and risk factors of pulmonary atelectasis in mechanically ventilated trauma patients in ICU: a prospective study. JBI Evidence Implementation, 17(1), 44-52.
- 9Hedenstierna, G., & Edmark, L. (2010). Mechanisms of atelectasis in the perioperative period. Best Practice & Research Clinical Anaesthesiology, 24(2), 157-169.
- 10Woodring, J. H., & Reed, J. C. (1996). Types and mechanisms of pulmonary atelectasis. Journal of Thoracic Imaging, 11(2), 92-108.
- 11Stark, P., Muller, N. L., & Finlay, G. (2020). Atelectasis: Types and pathogenesis in adults. U: UpToDate, Muller NL ed. UpToDate [Internet]. Waltham, MA: UpToDate.
- 12Woodring, J. H., & Reed, J. C. (1996). Types and mechanisms of pulmonary atelectasis. Journal of Thoracic Imaging, 11(2), 92-108.
- 13Peroni, D. G., & Boner, A. L. (2000). Atelectasis: mechanisms, diagnosis and management. Pediatric respiratory reviews, 1(3), 274-278.
- 14Peroni, D. G., & Boner, A. L. (2000). Atelectasis: mechanisms, diagnosis and management. Pediatric respiratory reviews, 1(3), 274-278.
- 15Carlsen, K. H., Crowley, S., & Smevik, B. (2019). Atelectasis. In Kendig’s Disorders of the Respiratory Tract in Children (pp. 1027-1033). Elsevier.
- 16Zhao, Y., Zheng, R., Xiang, W., Ning, D., & Li, Z. (2021). Systematic review and meta-analysis on perioperative intervention to prevent postoperative atelectasis complications after thoracic surgery. Annals of Palliative Medicine, 10(10), 107260734-107210734.
- 17Zhao, Y., Zheng, R., Xiang, W., Ning, D., & Li, Z. (2021). Systematic review and meta-analysis on perioperative intervention to prevent postoperative atelectasis complications after thoracic surgery. Annals of Palliative Medicine, 10(10), 107260734-107210734.
- 18Rothen, H. U., Sporre, B., Engberg, G., Wegenius, G., Reber, A., & Hedenstierna, G. (1995). Prevention of atelectasis during general anesthesia. The Lancet, 345(8962), 1387-1391.
- 19Zhao, Y., Zheng, R., Xiang, W., Ning, D., & Li, Z. (2021). Systematic review and meta-analysis on perioperative intervention to prevent postoperative atelectasis complications after thoracic surgery. Annals of Palliative Medicine, 10(10), 107260734-107210734.
- 20Zhao, Y., Zheng, R., Xiang, W., Ning, D., & Li, Z. (2021). Systematic review and meta-analysis on perioperative intervention to prevent postoperative atelectasis complications after thoracic surgery. Annals of Palliative Medicine, 10(10), 107260734-107210734.
- 21Boccatonda, A., Primomo, G., Cocco, G., D’Ardes, D., Marinari, S., Montanari, M., … & Schiavone, C. (2021). Not all abolished lung sliding are pneumothorax: the case of a particular lung atelectasis. Journal of Ultrasound, 24, 519-523.

