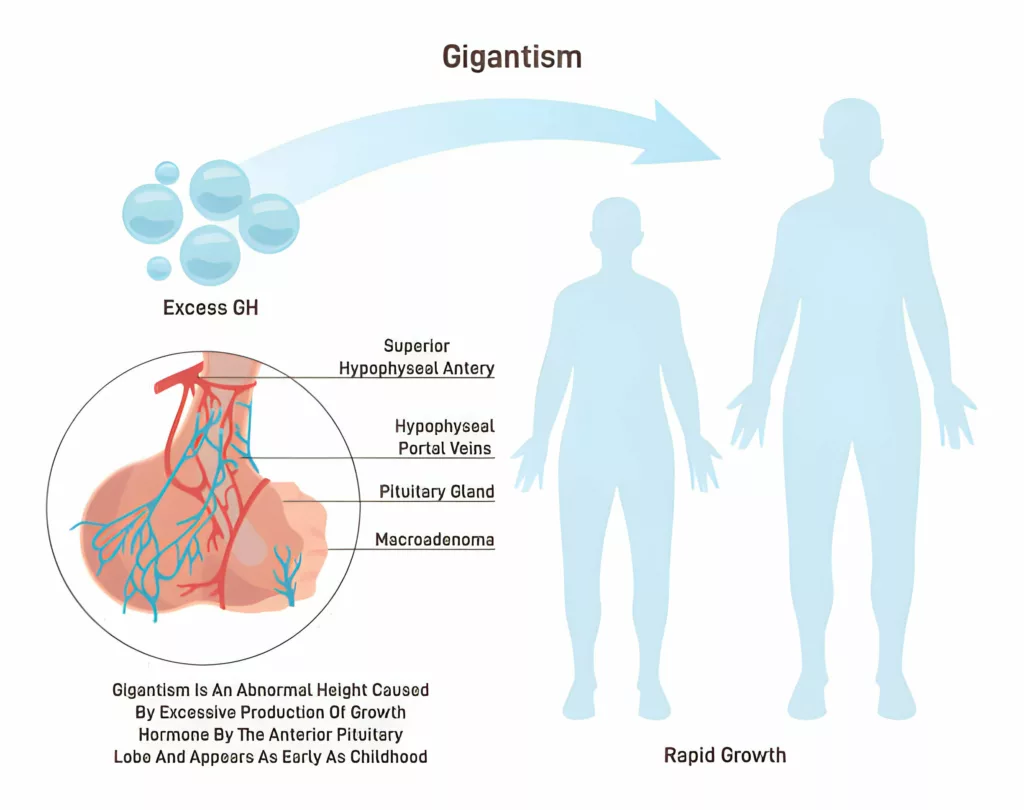
Gigantism, also known as pediatric acromegaly and pituitary gigantism, is an extremely rare disorder in which a kid or adolescent has elevated quantities of growth hormone (GH) in their body, causing them to grow extraordinarily tall. This usually happens because of a tumor in the brain’s pituitary gland.
What is Gigantism?
Gigantism is a pediatric disorder that makes the kids grow really tall. Usually, our bones grow under the influence of a “growth hormone” made inside the body.
Growth hormone, also known as human growth hormone (hGH) and somatotropin, is a natural hormone that promotes growth in children by acting on a variety of physiological systems. When your bones’ growth plates (epiphyses) merge, GH no longer increases height. Instead, it promotes proper bone, cartilage, and organ structure and metabolism. GH is closely related to insulin-like growth factor 1 (IGF1), which your liver produces. These hormones act together to regulate development and metabolism.
In gigantism, an overabundance of growth hormone (GH) causes muscle, bone, and connective tissue to expand faster. This results in an excessively tall height as well as various soft tissue abnormalities. If untreated, some people with gigantism have grown over 8 feet tall.
Gigantism specifically happens before the growth plates in the long bones, like the femur or humerus, have closed.1Bello MO, Garla VV. Gigantism and Acromegaly. [Updated 2023 Mar 20]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK538261/ When this condition occurs in adults, it’s known as acromegaly.
What Causes Gigantism?
Gigantism occurs due to the disturbance in the normal regulation mechanisms of growth hormones in the body. Here are some common causes that can lead to gigantism in kids:
Pituitary Tumor
The most common cause of gigantism is a tumor in the pituitary gland, which is like a control center for hormones in the body.2Rhee, N., Jeong, K., Yang, E. M., & Kim, C. J. (2014). Gigantism caused by growth hormone secreting pituitary adenoma. Annals of pediatric endocrinology & metabolism, 19(2), 96–99. https://doi.org/10.6065/apem.2014.19.2.96 Such a tumor called a pituitary adenoma can grow in the pituitary gland, causing it to produce too much growth hormone.
Genetic Factors
In some cases, gigantism can be passed down from parents who have genetic mutations affecting growth hormone production or regulation. A study with 208 participants found that about 46% of gigantism cases are inherited.3Rostomyan, L., Daly, A. F., Petrossians, P., Nachev, E., Lila, A. R., Lecoq, A. L., Lecumberri, B., Trivellin, G., Salvatori, R., Moraitis, A. G., Holdaway, I., Kranenburg-van Klaveren, D. J., Chiara Zatelli, M., Palacios, N., Nozieres, C., Zacharin, M., Ebeling, T., Ojaniemi, M., Rozhinskaya, L., Verrua, E., … Beckers, A. (2015). Clinical and genetic characterization of pituitary gigantism: an international collaborative study in 208 patients. Endocrine-related cancer, 22(5), 745–757. https://doi.org/10.1530/ERC-15-0320
Rare Conditions
Certain uncommon conditions like McCune-Albright syndrome or Carney complex can also cause gigantism by disrupting hormone secretion or signaling pathways.4Hannah-Shmouni, F., Trivellin, G., & Stratakis, C. A. (2016). Genetics of gigantism and acromegaly. Growth hormone & IGF research: official journal of the Growth Hormone Research Society and the International IGF Research Society, 30-31, 37–41. https://doi.org/10.1016/j.ghir.2016.08.002. Some of the conditions include:
Multiple Endocrine Neoplasia Type 1
MEN1 is a hereditary disorder characterized by tumors in various endocrine glands, including the pituitary gland. These tumors can result in the overproduction of growth hormone (GH).
McCune-Albright Syndrome
MAS is a hereditary disease affecting bones, skin, and internal organs. It manifests in several abnormalities, such as enlarged bones, brownish skin patches (cafe au-lait spots), and high growth hormone levels.
Neurofibromatosis Type 1
NF1 is a genetic illness characterized by the growth of tumors on the nerves in various parts of the body. It is also known as neurofibromatosis 1. Some kids can get cafe-au-lait spots, and they might be more prone to pituitary tumors.
Carney Complex
Carney Complex has been recognized as a rare genetic disease unique in the development of multiple tumors on the skin accompanied by pigmentation irregularities. It can involve pituitary gland tumors, which result in an enlarged pituitary gland size and the excess secretion of GH, leading to the condition of gigantism.
Familial Isolated Pituitary Adenomas
This is an inheritable condition, resulting in the growth of pituitary tumors in several members of the family. Some of these kinds of adenomas may overproduce the GH and HGH receptors, leading to gigantism.
Hypothalamic Disorders
The hypothalamus, a part of the brain, controls hormone production. Disorders in this area can upset the hormone balance related to growth, possibly leading to gigantism.
Other Tumors
Although pituitary tumors are the main cause, tumors in other body parts like the pancreas or lungs can sometimes release hormones that trigger growth, leading to gigantism.
Gigantism Signs & Symptoms
Gigantism symptoms are not just limited to abnormal height; they involve other organs as well:
- An unusually tall stature
- Disproportionately large hands and feet compared to the rest of their body
- Changes in facial features, such as a prominent jaw, enlarged nose, and thickened lips
- Joint pain and stiffness, especially in the knees and hips, due to the rapid growth and strain on the joints
- Excessive sweating, particularly at night
- Pressure from the pituitary tumor or changes in hormone levels can lead to headaches, especially in the frontal or temporal regions of the head.
- The pituitary tumor associated with gigantism can compress nearby structures, including the optic nerves, leading to vision changes or even loss of peripheral vision in severe cases.
- Internal organs may also enlarge, leading to abdominal discomfort or other symptoms.
Diagnosis of Gigantism

Since every child has a different growth rate, it can be tricky to diagnose gigantism. Gigantism should be suspected if the child’s height is 2 or 3 standard deviations above the mean height. Doctors compare the child’s height to what’s normal for their age and gender or to what’s typical for their parents’ heights.
To check for gigantism, doctors might use these tests:
- Blood Tests: These assess the hormone levels in the blood by taking a small sample from a vein. High levels of insulin-like growth factor-1 (IGF-1) might indicate gigantism
- Glucose Tolerance Test: This assesses how the body responds to sugar. It involves taking blood samples at different times after sugary drinks to see if growth hormone levels change as expected.
- Imaging Tests: If blood tests suggest gigantism, the doctor might recommend an MRI or CT scan of the head. These tests can reveal if there’s a tumor in the pituitary gland, often the cause of gigantism.
If someone is diagnosed with gigantism, the doctor might conduct further tests to check if other parts of their body are affected. These tests could include:
- An echocardiogram to check the heart.
- X-rays or scans to assess bone health.
- Sleep tests to detect sleep problems like sleep apnea.
Treatment Options for Gigantism
The treatment options for gigantism are:
Surgery
Surgery is the primary treatment for gigantism, offering the best chance for a cure.
Surgeons use a method called transsphenoidal approach, entering through the sphenoid sinus behind the nose. This minimally invasive technique accesses the pituitary gland without external incisions or bruising.
The tumor is removed using precise instruments and high magnification, often aided by endoscopic pituitary surgery, which involves a tiny camera through the nostrils.
The goal is to remove the tumor while minimizing damage to surrounding tissues, promoting a swift recovery. Most patients can return home the day after surgery.
Pharmacological Treatment and Hormone Therapy
If surgery isn’t successful or recommended, medications may be prescribed.
- Synthetic forms of somatostatin, like octreotide or lanreotide, can effectively control gigantism by suppressing growth hormone release. However, these drugs require regular injections.
- Bromocriptine and cabergoline, dopamine agonists, can also lower growth hormone levels, albeit less effectively5Gonzaga, M. F. M., de Castro, L. F., Naves, L. A., Mendonça, J. L., Oton de Lima, B., Kessler, I., & Casulari, L. A. (2018). Prolactinomas Resistant to Treatment With Dopamine Agonists: Long-Term Follow-Up of Six Cases. Frontiers in endocrinology, 9, 625. https://doi.org/10.3389/fendo.2018.00625.
- Pegvisomant is a newer drug that blocks growth hormone action and is administered by daily injections under the skin.
Radiotherapy
There are two types of radiotherapy for gigantism.
Stereotactic Radiation Therapy
Stereotactic radiotherapy (SRT) stands for a type of radiation therapy that has great precision in sending a high dose of radiation to the tumor. At the same time, attention is given to the surrounding healthy tissues. Through advanced imaging technologies like MRI or CT scan, SRT guarantees accurate tumor localization in the three-dimensional space. The technique mostly involves a few high-dose fractions delivered over the shorter treatment period. It is an excellent choice for pituitary gigantism because its efficiency and safety profile reduce the risk of damaging nearby essential structures such as the optic nerve.
Conventional Radiation Therapy
On the other hand, Traditional or external beam radiation therapy (EBRT) is one where the radiant energy comes to the tumor from outside the body using the linear accelerator. It must be clarified that the radiation doses used in the EBRT differ significantly from the higher doses adopted in SRT. These doses are delivered in a shorter period than in the course of EBRT, which is longer. Although it has low precision compared to SRT, for larger tumors or those situated in less vital areas where precise targeting is not crucial, the EBRT still remains a preferred option. Both therapy methods refer to minimizing or regulating pituitary tumors, reducing excess secretion, and allowing the individual to undergo a normal health state.
Gamma Knife Radiosurgery
This advanced radiation treatment offers an alternative to traditional surgery.
It delivers precise radiation beams to the tumor, gradually reducing hormone levels over several years.
Gamma Knife is outpatient, noninvasive, and requires only brief sedation. However, due to the longer timeframe for hormone normalization, it’s typically considered a last resort.
Complications Related to Gigantism Treatment
After undergoing surgery or radiation therapy for gigantism, there are potential complications that patients may experience. These include:
Hypopituitarism:
Around 60% of people treated for gigantism develop hypopituitarism, a condition in which the pituitary gland doesn’t produce enough hormones6Kim S. Y. (2015). Diagnosis and Treatment of Hypopituitarism. Endocrinology and metabolism (Seoul, Korea), 30(4), 443–455. https://doi.org/10.3803/EnM.2015.30.4.443. Treatment involves taking medications to replace the missing hormones.
Surgical Complications:
Surgery to remove a pituitary tumor can sometimes lead to complications such as:
- Bleeding
- Leaks of cerebrospinal fluid (CSF)
- Meningitis (infection of the membranes surrounding the brain and spinal cord)
- Imbalances in sodium and water levels in the body
Side Effects of Radiation Therapy:
Radiation therapy, while effective, can have its own set of side effects, including:
- Impaired fertility
- Vision loss
- Brain injury
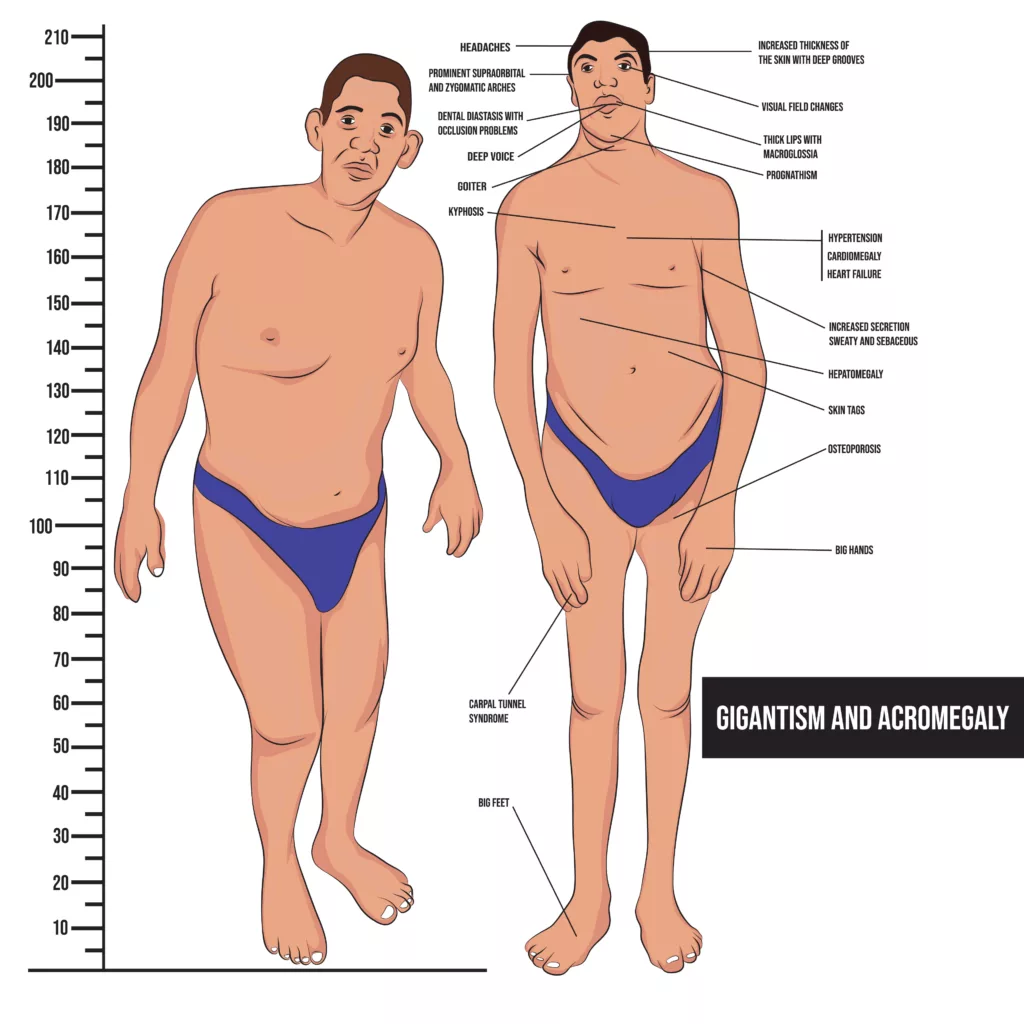
Gigantism Vs Acromegaly – What’s The Difference?
Gigantism and acromegaly are two different conditions but have the same cause: an abnormally increased growth hormone in the body. Both conditions have different times of onset and symptoms.
Doctors can find these conditions by checking the insulin-like growth factor-1 (IGF-1) hormone level. Surgery is often the first treatment, but it might not cure the problem. Sometimes, more treatment like medicine or radiation is needed.7Katznelson, L., Laws, E. R., Jr, Melmed, S., Molitch, M. E., Murad, M. H., Utz, A., Wass, J. A., & Endocrine Society (2014). Acromegaly: an endocrine society clinical practice guideline. The Journal of clinical endocrinology and metabolism, 99(11), 3933–3951. https://doi.org/10.1210/jc.2014-2700 Doctors and other healthcare workers work together to help people with these conditions improve.
| Gigantism | Acromegaly | |
| Onset | It occurs during childhood, before growth plates close | Develops in adulthood, after growth plates have closed |
| Symptoms | Excessive height, rapid growth, enlarged hands/feet/facial features | Enlarged hands/feet/facial features, thickened skin, joint pain, organ enlargement |
| Diagnosis | Based on height, growth rate, hormonal tests (elevated GH) | Physical examination, imaging studies (MRI), hormonal tests (GH, IGF-1) |
| Complications | Joint problems, vision problems, increased risk of heart disease | Cardiovascular disease, diabetes, arthritis, sleep apnea, increased cancer risk |
Soto’s Syndrome
Sotos syndrome is an uncommon hereditary condition in which children get taller than their agemates. Sotos syndrome symptoms include different physical characteristics, cognitive difficulties, and behavioral obstacles. Children with Sotos syndrome have an optimistic outlook and a typical lifetime.8Mathai, S. S., & Purkayastha, S. B., Retd (1996). CEREBRAL GIGANTISM (SOTOS’ SYNDROME): A Case Report. Medical journal, Armed Forces India, 52(3), 200–201. https://doi.org/10.1016/S0377-1237(17)30804-3
Can Gigantism Be Prevented?
Unfortunately, you can do little to prevent gigantism, but early detection is critical. Prompt treatment can help prevent or decrease the alterations that cause your child to become extremely tall.
Gigantism Life Expectancy – What is their Average lifespan?
People with gigantism typically have a shorter lifespan compared to the general population. Life expectancy for gigantism varies based on factors like treatment effectiveness and associated health issues. Early diagnosis and treatment can improve outcomes, but complications like cardiovascular problems may impact life expectancy. With proper management, many individuals lead fulfilling lives.
To sum it up, gigantism is a condition due to an increase in the growth hormone. It differs from acromegaly and has unique diagnosis and treatment options.
Refrences
- 1Bello MO, Garla VV. Gigantism and Acromegaly. [Updated 2023 Mar 20]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK538261/
- 2Rhee, N., Jeong, K., Yang, E. M., & Kim, C. J. (2014). Gigantism caused by growth hormone secreting pituitary adenoma. Annals of pediatric endocrinology & metabolism, 19(2), 96–99. https://doi.org/10.6065/apem.2014.19.2.96
- 3Rostomyan, L., Daly, A. F., Petrossians, P., Nachev, E., Lila, A. R., Lecoq, A. L., Lecumberri, B., Trivellin, G., Salvatori, R., Moraitis, A. G., Holdaway, I., Kranenburg-van Klaveren, D. J., Chiara Zatelli, M., Palacios, N., Nozieres, C., Zacharin, M., Ebeling, T., Ojaniemi, M., Rozhinskaya, L., Verrua, E., … Beckers, A. (2015). Clinical and genetic characterization of pituitary gigantism: an international collaborative study in 208 patients. Endocrine-related cancer, 22(5), 745–757. https://doi.org/10.1530/ERC-15-0320
- 4Hannah-Shmouni, F., Trivellin, G., & Stratakis, C. A. (2016). Genetics of gigantism and acromegaly. Growth hormone & IGF research: official journal of the Growth Hormone Research Society and the International IGF Research Society, 30-31, 37–41. https://doi.org/10.1016/j.ghir.2016.08.002
- 5Gonzaga, M. F. M., de Castro, L. F., Naves, L. A., Mendonça, J. L., Oton de Lima, B., Kessler, I., & Casulari, L. A. (2018). Prolactinomas Resistant to Treatment With Dopamine Agonists: Long-Term Follow-Up of Six Cases. Frontiers in endocrinology, 9, 625. https://doi.org/10.3389/fendo.2018.00625
- 6Kim S. Y. (2015). Diagnosis and Treatment of Hypopituitarism. Endocrinology and metabolism (Seoul, Korea), 30(4), 443–455. https://doi.org/10.3803/EnM.2015.30.4.443
- 7Katznelson, L., Laws, E. R., Jr, Melmed, S., Molitch, M. E., Murad, M. H., Utz, A., Wass, J. A., & Endocrine Society (2014). Acromegaly: an endocrine society clinical practice guideline. The Journal of clinical endocrinology and metabolism, 99(11), 3933–3951. https://doi.org/10.1210/jc.2014-2700
- 8Mathai, S. S., & Purkayastha, S. B., Retd (1996). CEREBRAL GIGANTISM (SOTOS’ SYNDROME): A Case Report. Medical journal, Armed Forces India, 52(3), 200–201. https://doi.org/10.1016/S0377-1237(17)30804-3





