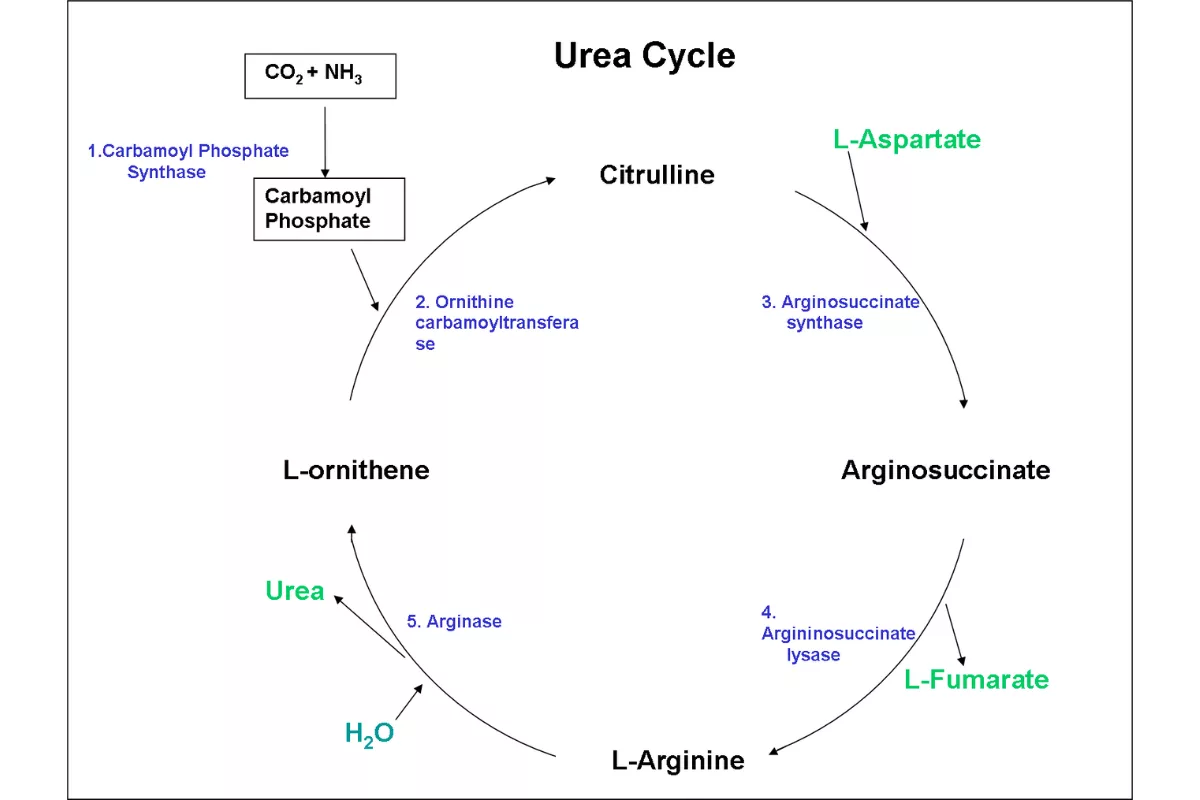
Hyperammonemia is a serious metabolic condition that occurs when ammonia accumulates abnormally in your blood due to impaired elimination or excessive production. Ammonia is produced in the body during the breakdown of protein and amino acids and is normally detoxified by the urea cycle in the liver.
But when your liver can’t do its job, or when too much ammonia is made, the levels rise above the normal limit (<50 µmol/L in adults), and that’s when things turn dangerous. You may risk confusion, cerebral edema, coma, and death. Early recognition of its types, causes, and symptoms is essential for immediate diagnosis and treatment.
Pathophysiology of Hyperammonemia
Ammonia (NH₃) is a toxic waste product produced during protein breakdown. Although the liver removes most ammonia, about 90%, through the urea cycle, the remaining ammonia is cleared by other tissues, particularly the brain and skeletal muscles. These tissues convert ammonia into glutamine via the enzyme glutamine synthetase.1Leger, R. F., Silverman, M. S., Hauck, E. S., & Guvakova, K. D. (2020). Hyperammonemia Post Lung Transplantation: A Review. Clinical Medicine Insights: Circulatory, Respiratory and Pulmonary Medicine. https://doi.org/10.1177/1179548420966234
However, liver failure or deficiencies of enzymes that work in the urea cycle cause ammonia to rise in the blood to a toxic level. This elevated ammonia crosses the blood-brain barrier (BBB), a protective layer that normally protects the brain from harmful substances.
- Once ammonia crosses the blood-brain barrier, it starts to accumulate in the astrocytes, the specialized brain cells. Astrocytes convert the ammonia to glutamine, a comparatively less toxic form of nitrogen. But this leads to another problem.
The glutamine then starts to build up inside astrocytes, creating a pulling effect that draws water into the cells. This results in the swelling of the brain cells, called cytotoxic cerebral edema, a major contributor to increased pressure in the brain.2Sepehrinezhad, A., Zarifkar, A., Namvar, G., Shahbazi, A., & Williams, R. (2020). Astrocyte swelling in hepatic encephalopathy: molecular perspective of cytotoxic edema. Metabolic brain disease, 35(4), 559–578. https://doi.org/10.1007/s11011-020-00549-8 - Furthermore, when excess glutamine enters the mitochondria of astrocytes, it is broken down, forming ammonia again. This ammonia inside the mitochondria disrupts their normal functioning.
- Ammonia also interferes with the brain’s energy supply by blocking important steps in how cells make energy. This leads to less energy (ATP) production, which harms brain cells.
Types & Causes of Hyperammonemia
Hyperammonemia can result from either a primary or secondary cause.3Ali R, Nagalli S. Hyperammonemia. [Updated 2023 Apr 7]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK557504/
Primary Hyperammonemia:
Genetic or inborn errors in the metabolism of urea lead to primary hyperammonemia. These inherited disorders are generally present in newborns and impair the liver’s ability to convert ammonia into urea.
- Urea Cycle Disorders (UCDs): These are one of the most common causes of primary hyperammonemia. They occur when any enzyme in the urea cycle is missing or not working properly. One well-known example is ornithine transcarbamylase (OTC) enzyme deficiency.
- Other Inherited Metabolic Disorders: Conditions such as organic acidemias (including propionic acidemia and methylmalonic acidemia) and fatty acid oxidation defects disrupt the way your body breaks down fats and proteins for energy. This also causes ammonia to build up in the body.4Häberle, J., Chakrapani, A., Mew, N. A., & Longo, N. (2018). Hyperammonaemia in classic organic acidaemias: A review of the literature and two case histories. Orphanet Journal of Rare Diseases, 13, 219. https://doi.org/10.1186/s13023-018-0963-7
- Transient Hyperammonemia of the Newborn (THAN): THAN is a temporary rise in blood ammonia levels seen in some premature babies, usually in the first few days after birth. It is considered tricky to diagnose because you can only diagnose it after ruling out all known genetic and acquired causes of hyperammonemia.
Secondary Hyperammonemia:
Secondary hyperammonemia occurs when non‑genetic factors either increase ammonia production or impair its clearance. Unlike primary hyperammonemia, it occurs at any age, often due to liver disease or drug toxicity.
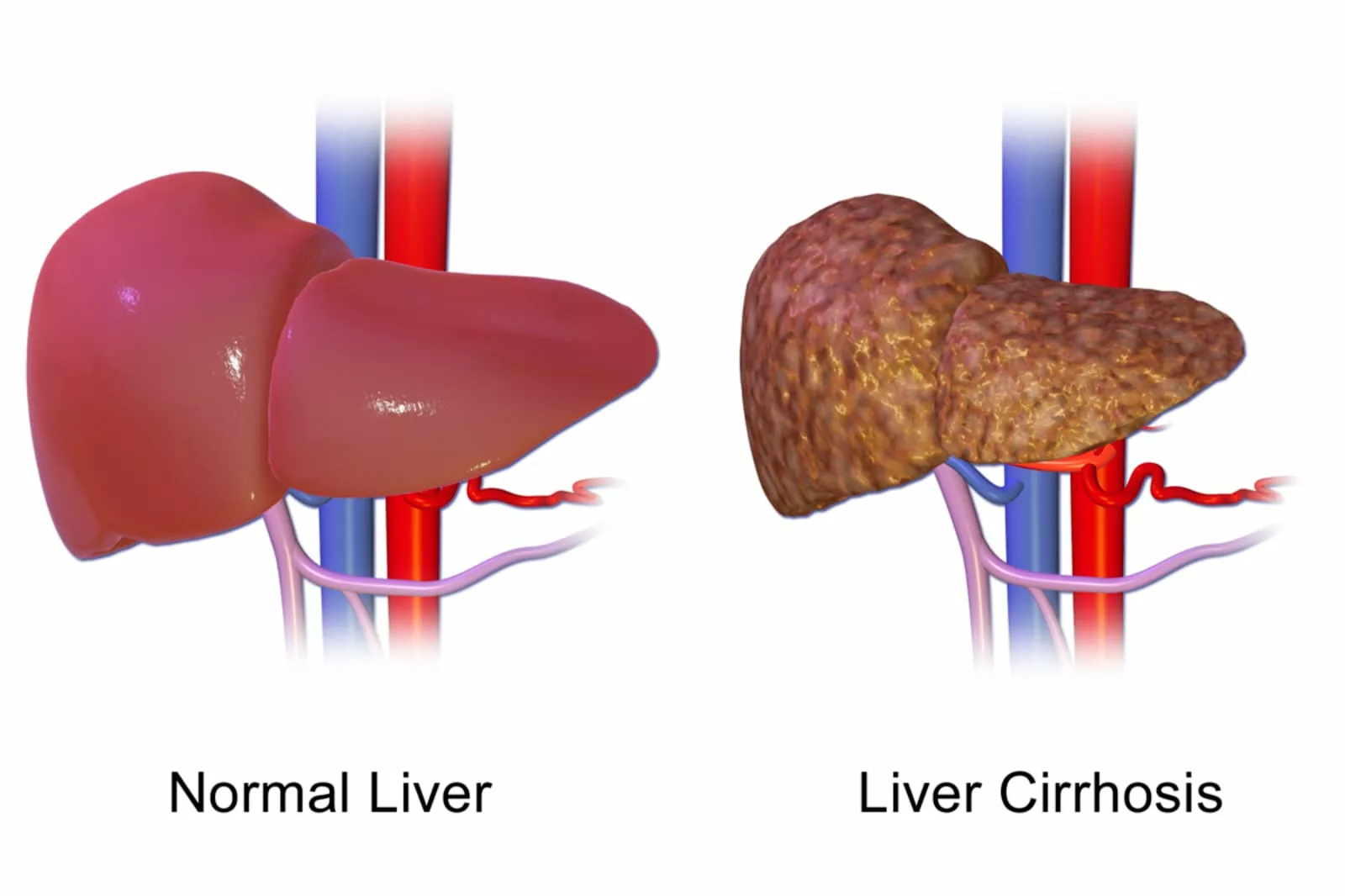
- Advanced Liver Disease: It is the most common cause of secondary hyperammonemia. When the liver is severely damaged, like in cirrhosis and acute liver failure, the liver can’t clear the ammonia properly from the body. As a result, ammonia starts to build up in your blood, leading to hyperammonemia.
- Medications: Drugs like valproic acid interfere with the urea cycle and cause hyperammonemia even in the absence of liver disease.
- Catabolic States: In critical illness, our body breaks down more protein, which pushes up ammonia levels. 5Zhao, L., Walline, J. H., Gao, Y., Lu, X., Yu, S., Ge, Z., Zhu, H., & Li, Y. (2020). Prognostic Role of Ammonia in Critical Care Patients Without Known Hepatic Disease. Frontiers in medicine, 7, 589825. https://doi.org/10.3389/fmed.2020.589825
- Infections: Some bacteria, such as Klebsiella and Proteus, and fungi like Cryptococcus neoformans produce an enzyme called urease. This enzyme breaks down urea into ammonia, leading to increased ammonia levels.
- Iatrogen Causes: Certain treatments like total parenteral nutrition (TPN), organ transplants, and chemotherapy can also cause hyperammonemia by increasing nitrogen load or affecting liver function.
How common is Hyperammonemia?
While hyperammonemia is uncommon in healthy individuals, it frequently occurs in newborns with metabolic disorders, adults with liver disease, critically ill ICU patients, and users of drugs such as valproic acid.
- A study found that urea cycle disorders affect about 1 out of every 35,000 babies born in the United States.6Summar, M. L., Koelker, S., Freedenberg, D., Le Mons, C., Haberle, J., Lee, H. S., Kirmse, B., European Registry and Network for Intoxication Type Metabolic Diseases (E-IMD). Electronic address: http://www.e-imd.org/en/index.phtml, & Members of the Urea Cycle Disorders Consortium (UCDC). Electronic address: http://rarediseasesnetwork.epi.usf.edu/ucdc/ (2013). The incidence of urea cycle disorders. Molecular genetics and metabolism, 110(1-2), 179–180. https://doi.org/10.1016/j.ymgme.2013.07.008
- THAN is surprisingly common, affecting over half of premature babies in their first two months of life. 7Ni, B., Qin, M., Zhao, J., & Guo, Q. (2022). A glance at transient hyperammonemia of the newborn: Pathophysiology, diagnosis, and treatment: A review. Medicine, 101(48), e31796. https://doi.org/10.1097/MD.0000000000031796
- A study claimed that about 90% of the hyperammonemia cases in adults are related to liver diseases.8Ali R, Nagalli S. Hyperammonemia. [Updated 2023 Apr 7]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK557504/
- It is observed that about half of the ICU patients without diagnosed liver disease had elevated plasma ammonia levels. Persistent hyperammonemia is also one of the main causes of death in the ICU.9Zhao, L., Walline, J. H., Gao, Y., Lu, X., Yu, S., Ge, Z., Zhu, H., & Li, Y. (2020). Prognostic Role of Ammonia in Critical Care Patients Without Known Hepatic Disease. Frontiers in Medicine, 7, 589825. https://doi.org/10.3389/fmed.2020.589825
- Half of the patients taking valproic acid face the problem of hyperammonemia.10Raru, Y., & Zeid, F. (2017). Hypoxic respiratory failure due to hyperammonemia encephalopathy induced by concurrent use of valproic acid and topiramate, a case report and review of the literature. Respiratory Medicine Case Reports, 25, 1-3. https://doi.org/10.1016/j.rmcr.2018.05.026
Symptoms of Hyperammonemia
Symptoms of hyperammonemia can vary from mild behavioral changes to severe, life-threatening neurological problems. The severity of symptoms depends on the level of ammonia in the blood and the underlying cause.
Neurological Symptoms:
Hyperammonemia is mainly toxic to our brains. In the brain, increased ammonia levels cause swelling, disrupt brain signals, and build up pressure inside the head.
Neonates & Infants
In newborns, symptoms typically appear within a few days of birth. Parents may notice:
- Poor feeding
- Vomiting
- Lethargy
- Hypotonia (floppy baby)
- Irritability
- Seizures
- Breathing difficulty
- Coma (in severe cases)
Older Children & Adults
Secondary hyperammonemia usually causes mental and behavioral symptoms. The early symptoms include:
- Irritability
- Confusion
- Headache
- Nausea and Vomiting
- Drowsiness and personality change
As the ammonia levels keep rising, it results in more severe toxicity, causing:
- Marked confusion
- Agitation
- Reduced consciousness
- Disorientation
- Slurred speech
- Seizures
- Coma
Asterixis (flapping hand tremor) is a classic physical sign of hepatic encephalopathy. It’s often linked to liver or metabolic brain problems, and also to certain medicines like valproate or carbamazepine.11Rissardo, J. P., Muhammad, S., Yatakarla, V., Vora, N. M., Paras, P., & Caprara, A. L. (2024). Flapping Tremor: Unraveling Asterixis—A Narrative Review. Medicina, 60(3), 362. https://doi.org/10.3390/medicina60030362
Complications of Hyperammonemia
These are the emergency conditions that require immediate attention.
- Increased intracranial pressure (ICP): Cerebral edema, which is the brain swelling, can press on the brain so hard that it becomes life-threatening. The continuous increase in pressure inside the brain may result in pushing out parts of the brain through openings in the skull.
- Hepatic Encephalopathy: In liver diseases, the increased ammonia reaches the brain and causes confusion, disorientation, and even coma.
- Other complications: Infections, kidney dysfunction, and low blood pH (acidosis) are also linked to hyperammonemia.
Other Systemic Signs:
These signs are usually secondary but can give important diagnostic clues:
- Low body temperature (especially in neonates)
- Respiratory alkalosis (due to rapid breathing)
- Vomiting and dehydration
- Enlarged liver (if associated with liver disease)
- Skin rash or unusual body odor (in some inborn errors of metabolism)
How is Hyperammonemia diagnosed?
Diagnosis of hyperammonemia requires high suspicion, especially in patients with unexplained neurological symptoms, liver disease, changed mental status, or metabolic crisis.
Plasma Ammonia Level:
The primary test for the diagnosis of hyperammonemia is the measurement of plasma ammonia levels. Its value varies with age. Normal values are < 50 µmol/L in adults and < 80 µmol/L in children. Levels of 80–150 µmol/L indicate moderate risk, while > 200 µmol/L is severe.
However, ammonia testing is highly sensitive and prone to false results if not handled properly. To ensure accuracy, blood should be drawn from a free-flowing vein with minimal or no tourniquet application.
The sample must be transported on ice and processed within 30 minutes to prevent artificial elevation of ammonia levels.
Other Laboratory Tests:
After confirming the elevation of ammonia levels in the body, further laboratory tests help determine the underlying cause. These are:
Liver Function Tests (LFTs)
Elevated values of the following chemicals in the plasma are common in cirrhosis, acute liver failure, or drug-induced liver injury.
- Aspartate aminotransferase (AST)
- Alanine aminotransferase (ALT)
- Bilirubin
A prolonged International Normalized Ratio (INR) also suggests a hepatic origin.
Arterial Blood Gases (ABG)
This test measures oxygen and acid levels in the blood.
- May show respiratory alkalosis, especially in the early stages. This happens when rapid breathing lowers carbon dioxide levels in the blood.
- Metabolic acidosis is seen in organic acidemias due to excess acid in the body.
Serum Electrolytes & Glucose
- Decreased blood glucose level, elevated lactate, or anion gap acidosis point toward inborn errors of metabolism
Plasma Amino Acids & Urinary Organic Acids
- Used for diagnosing urea cycle disorders and organic acidemias
- High levels of glutamine and alanine suggest that the body is overwhelmed trying to detoxify excess ammonia. Glutamine and alanine are the amino acids, the building blocks of protein.
Plasma Carnitine & Acylcarnitine Profile
- Indicates fatty acid oxidation defects or valproate toxicity
Serum Urea and Creatinine
- Helps distinguish liver vs kidney cause
Genetic & Metabolic Testing:
Genetic testing is essential in neonates and older children, where your doctor suspects primary hyperammonemia. These genetic tests include sequencing of urea cycle genes such as:
- OTC (Ornithine Transcarbamylase)
- CPS1 (Carbamoyl Phosphate Synthetase I)
- ASS1 (Argininosuccinate Synthetase 1)
- ASL (Argininosuccinate Lyase)
All of which encode enzymes that help detoxify ammonia by converting it into urea.
Rapid genetic testing is now easily available and helps start enzyme-specific treatments quickly. Doctors recommend doing genetic tests right away in any newborn with unexplained hyperammonemia above 150 µmol/L, especially if there’s no clear liver-related cause.
Neuroimaging:
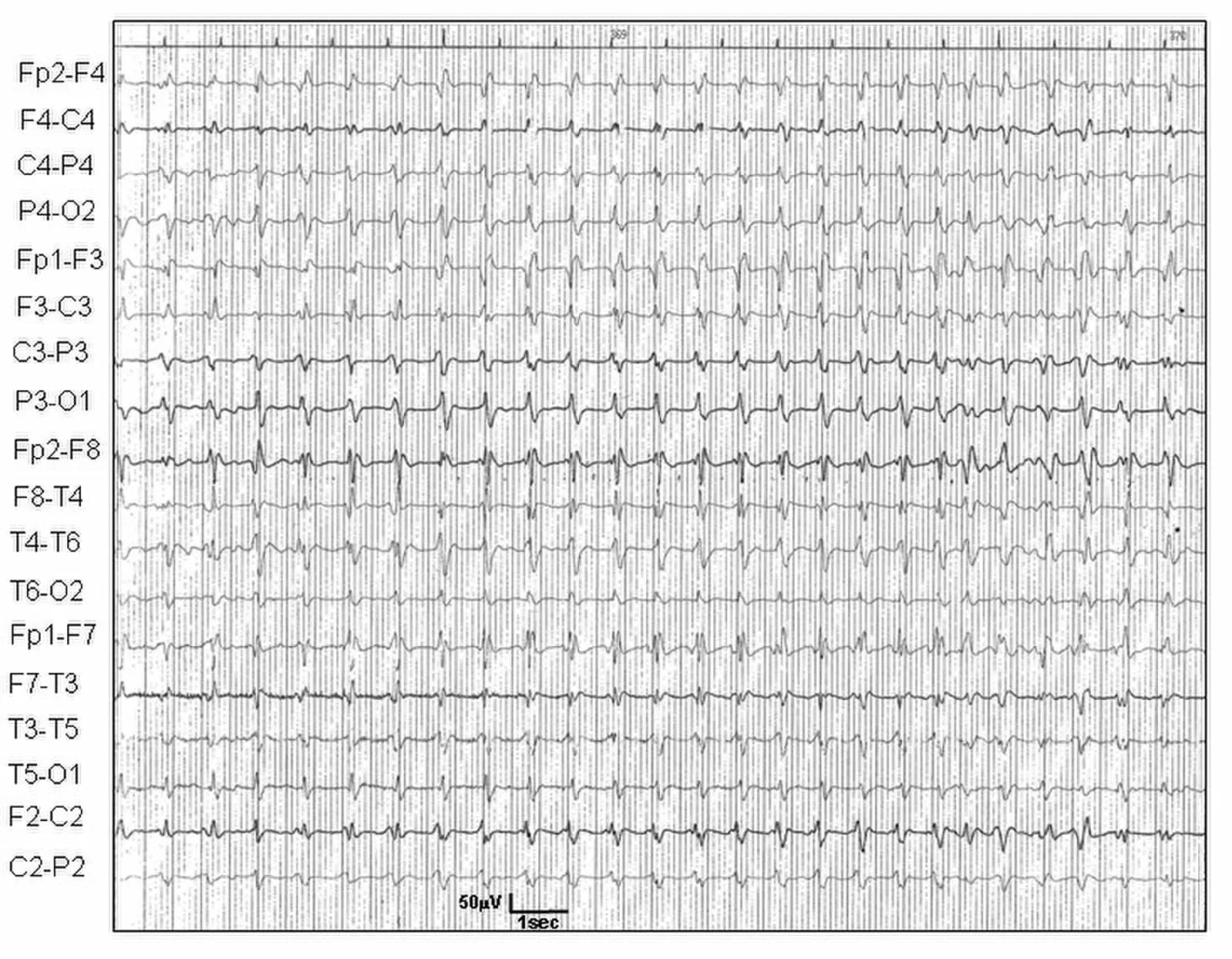
Neuroimaging and EEG are required if the symptoms are severe.
- Brain CT scans and MRIs reveal diffuse cerebral edema, particularly if the ammonia levels rise above 200-300 µmol/L.
- Electroencephalogram (EEG) is also helpful in identifying subclinical seizures that happen without obvious physical symptoms and encephalopathy patterns.
In hepatic encephalopathy, EEG often shows a typical pattern called triphasic waves, a specific pattern in which each wave has three distinct phases: a sharp upstroke, a quick dip, and another upward slope. 12Emmady PD, Murr NI. EEG Triphasic Waves. [Updated 2023 Feb 1]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK557679/
When to Suspect Hyperammonemia:
| Scenario | Consider Ammonia Testing If… |
| Neonate with vomiting, lethargy | Within the first 3–5 days of life, a metabolic disorder is suspected |
| Adults with liver disease | Confusion, drowsiness, or asterixis |
| ICU patient without liver disease | Sudden confusion, failure to wean from the ventilator |
| Post-valproate or chemotherapy patient | Drowsiness, ataxia, or altered mental status |
| Post-transplant patient | Rapid neurological deterioration |
Management & Treatment Options for Hyperammonemia
Management of hyperammonemia aims to rapidly reduce the ammonia level, treat the underlying cause, prevent further ammonia accumulation, and protect the brain from damage.
Initial Emergency Measures:
Hyperammonemia is a life-threatening emergency that requires rapid and targeted interventions.
- Withholding Protein: The first step in the hyperammonemia crisis is to stop protein intake immediately to prevent more ammonia from building up.
- High‑dose IV Dextrose: The administration of 10-15% intravenous dextrose with insulin can provide calories and shift the protein catabolism (breakdown) to anabolism to reduce ammonia production.
- Supportive Intensive Care: If the hyperammonia in the patient exceeds the level of 200 µmol/L, or the patient shows signs of encephalopathy or cerebral edema, intensive care becomes essential. Transfer the patient to the ICU for dose monitoring, seizure control, and respiratory support if needed.
Hemodialysis & Kidney Replacement Therapy (KRT):
When the ammonia exceeds 500 µmol/L, or the patient is in a coma, or unresponsive to medical therapy, kidney replacement therapies (KRTs) are the fastest and most effective way to clear ammonia from the bloodstream.
- Intermittent Hemodialysis (iHD): It is the most effective method, which works by removing ammonia directly from the blood.
- Continuous Kidney Replacement Therapy (CKRT): This special type of dialysis, which works slowly and continuously over 24 hours, is preferred in neonates and critically unstable patients. This gentle approach helps prevent sudden drops in blood pressure, making it safer for critically ill patients.
A clinical study found that the duration of coma before starting dialysis was the strongest predictor of outcome. Infants who began dialysis earlier had significantly better neurological recovery.13Picca, S., Dionisi-Vici, C., Abeni, D., Pastore, A., Rizzo, C., Orzalesi, M., Sabetta, G., Rizzoni, G., & Bartuli, A. (2001). Extracorporeal dialysis in neonatal hyperammonemia: modalities and prognostic indicators. Pediatric nephrology (Berlin, Germany), 16(11), 862–867. https://doi.org/10.1007/s004670100702
Specific Treatment Options Based on Underlying Cases:
Urea Cycle Disorders
In patients with urea cycle disorders or unknown causes, doctors use ammonia scavengers to provide an alternate route to eliminate nitrogen.
- Nitrogen Scavenger Medications: These medications are sodium benzoate, sodium phenylacetate, and sodium phenylbutyrate. These medications bind nitrogen and help excrete it safely through urine.
- Arginine Supplementations: In many urea cycle defects, except arginase enzyme deficiency, intravenous arginine supports the residual cycle activity and nitrogen clearance.
Valproate-Induced Hyperammonemia
Valproic acid inhibits the Carbamoyl Phosphate Synthetase 1 (CPS1), the first enzyme of the urea cycle. Treatment of valproate-induced hyperammonemia involves:
- Immediate discontinuation of valproic acid
- Administration of L-carnitine, which helps reverse the CPS1 blockage.
- Supportive care and monitoring for liver injury
Liver Failure-Related Hyperammonemia
- Use lactulose, a non-absorbable sugar, that traps the ammonia by converting it into ammonium.
- Take rifaximin, an antibiotic, which kills the ammonia-producing bacteria in the gut.
- Manage intracranial hypertension if present.
A liver transplant is considered the only curative option for irreversible liver failure.
Prognosis & Life Expectancy of Hyperammonemia
The prognosis of hyperammonemia depends on how quickly it is diagnosed and treated, the severity of ammonia elevation, the underlying cause, and the patient’s age.
Prognosis in Neonates & Children:
Sadly, newborns with severe hyperammonemia often face lifelong challenges. But if caught early, some go on to live full lives.
- A study of newborns with early-onset UCD found that 7 out of 10 babies survived the newborn stage. However, among the survivors, about one-third had some form of intellectual or developmental disability. 14Pontoizeau, C., Roda, C., Arnoux, J. B., Vignolo-Diard, P., Brassier, A., Habarou, F., Barbier, V., Grisel, C., Abi-Warde, M. T., Boddaert, N., Kuster, A., Servais, A., Kaminska, A., Hennequin, C., Dupic, L., Lesage, F., Touati, G., Valayannopoulos, V., Chadefaux-Vekemans, B., Oualha, M., … de Lonlay, P. (2020). Neonatal factors related to survival and intellectual and developmental outcomes of patients with early-onset urea cycle disorders. Molecular genetics and metabolism, 130(2), 110–117. https://doi.org/10.1016/j.ymgme.2020.03.003
Those who present early and receive hemodialysis within 8 hours, along with scavenger therapy and dietary control, have a better chance of survival and cognitive development.
Prognosis in Adults:
In adults, the prognosis of hyperammonemia is closely linked with the underlying cause rather than the ammonia level alone.
- In patients with acute liver failure, persistent hyperammonemia (≥122 μmol/L for 3 days) is linked to poor outcomes. Unfortunately, only about 1 in 4 patients survived.15Kumar, R., Shalimar, Sharma, H., Prakash, S., Panda, S. K., Khanal, S., & Acharya, S. K. (2012). Persistent hyperammonemia is associated with complications and poor outcomes in patients with acute liver failure. Clinical gastroenterology and hepatology: the official clinical practice journal of the American Gastroenterological Association, 10(8), 925–931. https://doi.org/10.1016/j.cgh.2012.04.011
- In patients with cirrhosis or severe liver damage, those whose ammonia levels do not come to a normal level by day 5 had a high risk of death; sadly, about 7 out of 10 don’t survive.16Shalimar, Sheikh, M. F., Mookerjee, R. P., Agarwal, B., Acharya, S. K., & Jalan, R. (2019). Prognostic Role of Ammonia in Patients With Cirrhosis. Hepatology (Baltimore, Md.), 70(3), 982–994. https://doi.org/10.1002/hep.30534
However, if hyperammonemia in adults is treated early, especially in cases with valproate-induced hyperammonemia, patients often recover fully with discontinuation of the drug and L-carnitine therapy.
Life Expectancy in Hyperammonemia:
There is no single figure for the life expectancy in hyperammonemia because it varies widely depending on the cause and severity.
- In primary hyperammonemia, only about 1 in 3 children survive beyond 11 years.
- In secondary hyperammonemia, long-term survival is much higher, with nearly 9 out of 10 living past 11 years. The chances of survival often depend on how high the ammonia levels get and how long the person remains in a coma.17Ali R, Nagalli S. Hyperammonemia. [Updated 2023 Apr 7]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK557504
How to prevent Hyperammonemia?
Since hyperammonemia can progress to cerebral edema, coma, and death, its prevention is not just an ideal; it is lifesaving.
Prevention in Patients With Liver Disease:
Individuals with cirrhotic or chronic hepatitis require consistent control of ammonia-producing factors:
- Correct electrolyte imbalance: Especially hypokalemia (decreased potassium levels in the body) and metabolic acidosis, which can increase ammonia reabsorption.
- Avoid Gut Bleeding: Bleeding in the gut causes protein breakdown and ammonia production.
- Prevent Infections & Dehydration: These can precipitate hepatic encephalopathy.
Prevention of Inborn Errors Of Metabolism:
Preventive measures for the inborn errors of metabolism, especially UCDs, involve:
- Lifelong Protein Restrictions: Take low-protein diets to reduce the nitrogen load while ensuring the essential amino acids.
- Nitrogen Scavengers: Regular use of nitrogen scavengers helps prevent ammonia buildup.
- Supplements: Oral citrulline and arginine supplements support the urea cycle function.
- Sick day management protocol: During infections, fasting, or stress, patients require extra calories through glucose and temporary protein withdrawal.
- Emergency Plans for Families: Ready-to-use instructions, emergency contact numbers, and a “go-bag” for hospital visits to cope with any emergency.
Genetic Counseling & Screening:
For families with a known history of UCDs or other metabolic conditions:
- Prenatal testing and carrier screening can guide future family planning
- Newborn screening allows early detection before symptoms arise
- Early intervention in asymptomatic siblings can prevent first crises altogether
Conclusion
Hyperammonemia is a serious medical condition where excess ammonia builds up in the blood, often due to liver disease, genetic enzyme defects, or certain medications. Recognizing the early signs, such as vomiting, poor feeding, lethargy in newborns, or confusion and drowsiness in older children and adults, can help start early treatment. With timely diagnosis, ammonia-lowering treatments, and supportive care, many patients recover fully. Stay alert, understand the risks, and consult a doctor right away if symptoms suggest hyperammonemia.
Refrences
- 1Leger, R. F., Silverman, M. S., Hauck, E. S., & Guvakova, K. D. (2020). Hyperammonemia Post Lung Transplantation: A Review. Clinical Medicine Insights: Circulatory, Respiratory and Pulmonary Medicine. https://doi.org/10.1177/1179548420966234
- 2Sepehrinezhad, A., Zarifkar, A., Namvar, G., Shahbazi, A., & Williams, R. (2020). Astrocyte swelling in hepatic encephalopathy: molecular perspective of cytotoxic edema. Metabolic brain disease, 35(4), 559–578. https://doi.org/10.1007/s11011-020-00549-8
- 3Ali R, Nagalli S. Hyperammonemia. [Updated 2023 Apr 7]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK557504/
- 4Häberle, J., Chakrapani, A., Mew, N. A., & Longo, N. (2018). Hyperammonaemia in classic organic acidaemias: A review of the literature and two case histories. Orphanet Journal of Rare Diseases, 13, 219. https://doi.org/10.1186/s13023-018-0963-7
- 5Zhao, L., Walline, J. H., Gao, Y., Lu, X., Yu, S., Ge, Z., Zhu, H., & Li, Y. (2020). Prognostic Role of Ammonia in Critical Care Patients Without Known Hepatic Disease. Frontiers in medicine, 7, 589825. https://doi.org/10.3389/fmed.2020.589825
- 6Summar, M. L., Koelker, S., Freedenberg, D., Le Mons, C., Haberle, J., Lee, H. S., Kirmse, B., European Registry and Network for Intoxication Type Metabolic Diseases (E-IMD). Electronic address: http://www.e-imd.org/en/index.phtml, & Members of the Urea Cycle Disorders Consortium (UCDC). Electronic address: http://rarediseasesnetwork.epi.usf.edu/ucdc/ (2013). The incidence of urea cycle disorders. Molecular genetics and metabolism, 110(1-2), 179–180. https://doi.org/10.1016/j.ymgme.2013.07.008
- 7Ni, B., Qin, M., Zhao, J., & Guo, Q. (2022). A glance at transient hyperammonemia of the newborn: Pathophysiology, diagnosis, and treatment: A review. Medicine, 101(48), e31796. https://doi.org/10.1097/MD.0000000000031796
- 8Ali R, Nagalli S. Hyperammonemia. [Updated 2023 Apr 7]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK557504/
- 9Zhao, L., Walline, J. H., Gao, Y., Lu, X., Yu, S., Ge, Z., Zhu, H., & Li, Y. (2020). Prognostic Role of Ammonia in Critical Care Patients Without Known Hepatic Disease. Frontiers in Medicine, 7, 589825. https://doi.org/10.3389/fmed.2020.589825
- 10Raru, Y., & Zeid, F. (2017). Hypoxic respiratory failure due to hyperammonemia encephalopathy induced by concurrent use of valproic acid and topiramate, a case report and review of the literature. Respiratory Medicine Case Reports, 25, 1-3. https://doi.org/10.1016/j.rmcr.2018.05.026
- 11Rissardo, J. P., Muhammad, S., Yatakarla, V., Vora, N. M., Paras, P., & Caprara, A. L. (2024). Flapping Tremor: Unraveling Asterixis—A Narrative Review. Medicina, 60(3), 362. https://doi.org/10.3390/medicina60030362
- 12Emmady PD, Murr NI. EEG Triphasic Waves. [Updated 2023 Feb 1]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK557679/
- 13Picca, S., Dionisi-Vici, C., Abeni, D., Pastore, A., Rizzo, C., Orzalesi, M., Sabetta, G., Rizzoni, G., & Bartuli, A. (2001). Extracorporeal dialysis in neonatal hyperammonemia: modalities and prognostic indicators. Pediatric nephrology (Berlin, Germany), 16(11), 862–867. https://doi.org/10.1007/s004670100702
- 14Pontoizeau, C., Roda, C., Arnoux, J. B., Vignolo-Diard, P., Brassier, A., Habarou, F., Barbier, V., Grisel, C., Abi-Warde, M. T., Boddaert, N., Kuster, A., Servais, A., Kaminska, A., Hennequin, C., Dupic, L., Lesage, F., Touati, G., Valayannopoulos, V., Chadefaux-Vekemans, B., Oualha, M., … de Lonlay, P. (2020). Neonatal factors related to survival and intellectual and developmental outcomes of patients with early-onset urea cycle disorders. Molecular genetics and metabolism, 130(2), 110–117. https://doi.org/10.1016/j.ymgme.2020.03.003
- 15Kumar, R., Shalimar, Sharma, H., Prakash, S., Panda, S. K., Khanal, S., & Acharya, S. K. (2012). Persistent hyperammonemia is associated with complications and poor outcomes in patients with acute liver failure. Clinical gastroenterology and hepatology: the official clinical practice journal of the American Gastroenterological Association, 10(8), 925–931. https://doi.org/10.1016/j.cgh.2012.04.011
- 16Shalimar, Sheikh, M. F., Mookerjee, R. P., Agarwal, B., Acharya, S. K., & Jalan, R. (2019). Prognostic Role of Ammonia in Patients With Cirrhosis. Hepatology (Baltimore, Md.), 70(3), 982–994. https://doi.org/10.1002/hep.30534
- 17Ali R, Nagalli S. Hyperammonemia. [Updated 2023 Apr 7]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK557504

