What is Peroneal Tendonitis?
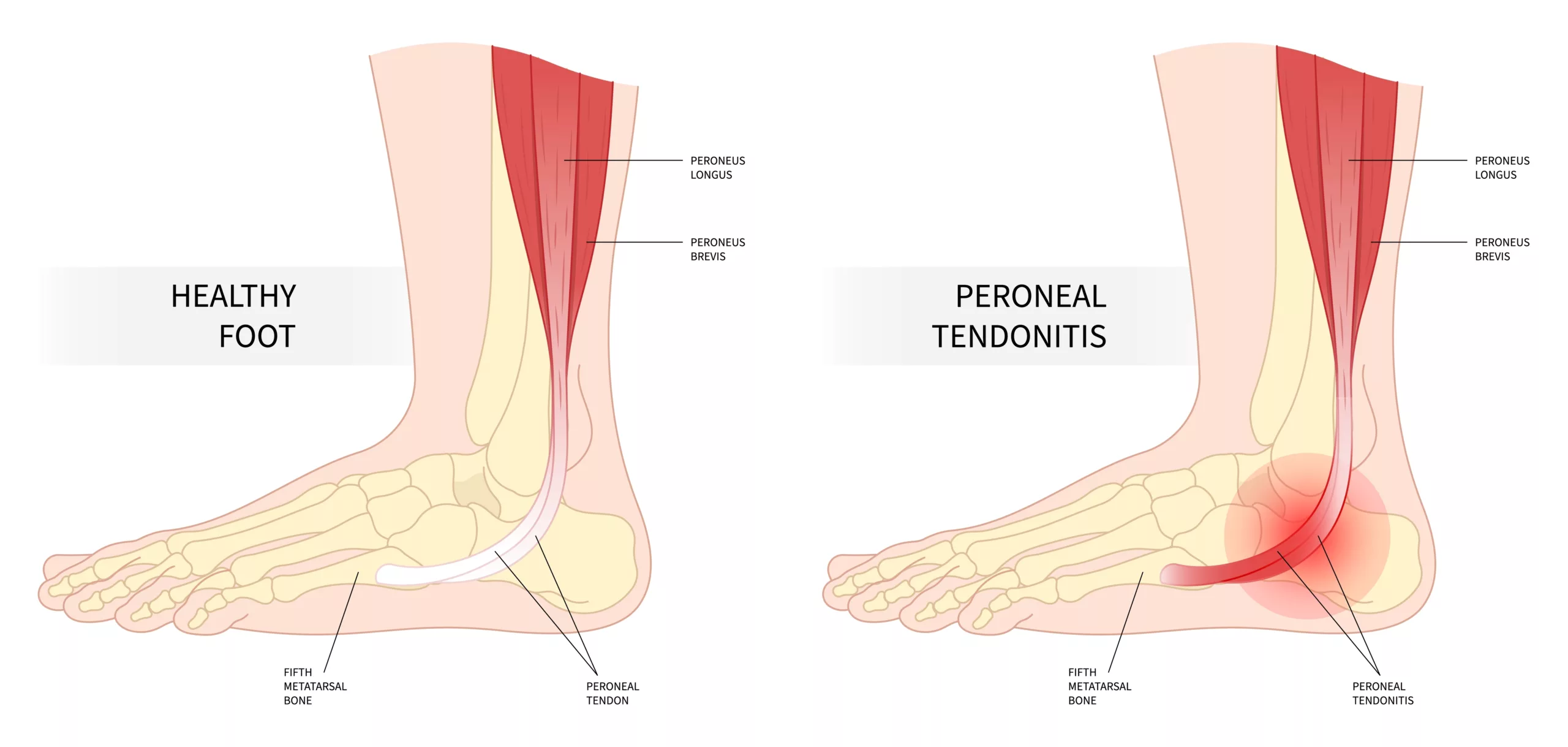
Peroneal tendonitis is an inflammatory condition affecting the peroneal tendons located on the outer side of the ankle. These tendons connect the peroneal muscles in the lower leg to the bones in the foot. They are responsible for stabilizing the ankle and enabling foot movement, particularly when walking or running. Inflammation of one or both peroneal tendons is called peroneal tendonitis. It results from trauma or overworking of the tendons, which causes pain and swelling in the ankle region. Peroneal tendonitis, also called peroneal tendinopathy, causes pain at the lateral side of the foot, i.e., the outer side of the ankle. Overburdened tendons rub against the bone, which creates friction, leading to inflammation of the peroneal tendons.
What are Peroneal Tendons?
Tendons are a type of connective tissue that connects muscles to bones. In the human body, two muscles join the lower fibula: the peroneus longus and the peroneus brevis. These muscles become tendons at the hind foot, with the peroneus brevis attached to the small toe. The peroneus longus continues under the foot and joins the arch on the opposite side. Both tendons play a role in stabilizing the foot and preventing strains.
What Causes Peroneal Tendonitis?
Peroneal tendonitis is common in athletes and long-distance runners due to repetitive ankle motion. Inflammation of the peroneal tendon may result from an acute injury, such as a sprain, or it may develop over some time (chronic injury). Another reason is the tightening of calf muscles due to repeated stress during exercise. Tight calf muscles stress peroneal tendons and overburden them. People who repetitively get ankle sprains have a higher chance of getting peroneal tendonitis.
Peroneal Tendonitis Symptoms
The symptoms of peroneal tendonitis can vary in severity but often include:
- Pain across the length of the tendon
- Swelling, warmth, and redness around the ankle1 Morrison, W. (ed.) (2017) Peroneal tendonitis: Causes, treatment, and recovery, Medical News Today. Retrieved 22 August 2023 from https://www.medicalnewstoday.com/articles/318349#Symptoms
- Thick tendons with a nodule-like mass that moves along the tendon
- Pain aggravates with physical activity.
- Some individuals may experience stiffness in the ankle, making it difficult to move the foot comfortably.
- Individuals may notice unusual sounds or sensations like clicking or snapping when moving the ankle.

Peroneal Tendonitis Diagnosis
The symptoms of peroneal tendonitis are like those of other foot problems that may be misdiagnosed.2Davda K, Malhotra K, O’Donnell P, Singh D, Cullen N. Peroneal tendon disorders. EFORT Open Rev. 2017 Jun 22;2(6):281-292. Doi: 10.1302/2058-5241.2.160047. PMID: 28736620; PMCID: PMC5508858. Your healthcare provider initially asks for your medical history to evaluate the use of the ankle and the nature of the injury. They might go for a physical examination and some imaging tests to further help with the diagnosis.
Physical Examination
Your physician may examine your foot for tenderness and swelling. They check the extent of movement by asking you to move your foot and applying pressure on different positions. It is important to confirm that the peroneal tendon and not the fibula are affected.
Imaging Tests
Various imaging tests are necessary to rule out fractures, cartilage damage, or osteoarthritis.
- X-ray imaging3 Mulcahy, J.A. (2019) GUIDE: Physical therapy guide to peroneal tendinopathy, Choose PT. Retrieved 22 August 2023 https://www.choosept.com/guide/physical-therapy-guide-peroneal-tendinopathy#:~:text=Your%20physical%20therapist%20may%20use,Range%2Dof%2Dmotion%20exercises is the primary technique to detect peroneal abnormalities.
- Ultrasound is another highly sensitive procedure that confirms any tears and evaluates the tendon’s movement.
- MRI provides a high-quality image of any tear in the peroneus brevis tendon characterized by bone edema, deformity, and discontinuity.
- CT Scan provides more fine details of bones and detects potential tendon dysfunction and bone deformity.
Peroneal Tendonitis Treatment
The primary treatment module is the non-surgical treatment. Peroneal tendinopathy usually improves with conservative treatment involving certain medications, stretches, compression, and ice. However, in some cases, surgery is preferred when the injury gets worse and the tendon ruptures.
Non-Surgical Treatment
It is important to rest well until the pain lessens and the tendon heals completely. Ice and a compression bandage are other good options for reducing ankle swelling. Continue non-surgical therapy for four to six weeks, but switch to surgery if your foot does not heal. Some common non-surgical therapy options are:
Immobilization:
Your physician might suggest a cast or a controlled ankle motion boot that allows limited ankle and foot movement. Immobilizing the injured foot assists in healing the injury.4 Walt, J. and Massey, P. (2023) Peroneal tendon syndromes – statpearls – NCBI bookshelf, Stat Pearls [Internet]. Retrieved 22 August 2023 https://www.ncbi.nlm.nih.gov/books/NBK544354/
Medications:
Oral and intravenous non-steroidal anti-inflammatory medications help relieve swelling and pain. If it does not work, an injection of cortisone5 Morrison, W. (ed.) (2018) Peroneal tendonitis: Causes, treatment, and recovery, Medical News Today. Retrieved 23 August 2023 from https://www.medicalnewstoday.com/articles/318349 into the tendon sheath is effective, but there is a risk of tendon rupture. Another advanced dosage form is the Platelet-rich plasma (PRP) injection6Dallaudière B; Pesquer L; Meyer P; Silvestre A; Perozziello A; Peuchant A; Durieux MH; Loriaut P; Hummel V; Boyer P; Schouman-Claeys E; Serfaty JM; B. (2014) intratendinous injection of platelet-rich plasma under US guidance to treat tendinopathy: A long-term pilot study, Journal of vascular and interventional radiology : JVIR. Retrieved 23 August 2023 from https://pubmed.ncbi.nlm.nih.gov/24656590/ that is administered into the peroneal tendon. This injection stimulates the migration of new cells and helps in the healing process.
Physical therapy:
A physiotherapist might suggest exercises and stretches to help strengthen the peroneal tendon. Physical therapy may include deep tissue friction massage, biomechanical ankle platform (BAPS), or ultrasound electric stimulation.
Bracing:
Wearing a brace is a good option for activities that involve constant ankle motion. It immobilizes the ankle and removes stress from the peroneal tendon.
KT Tape:
A KT tape improves blood circulation, supports the ankle, and relieves the pain associated with tendonitis. Wrap the tape all over your foot, from the heels upward to the outer side of your foot. Keep your foot at a 90-degree angle.
Surgical Treatment
When conservative treatments fail to relieve peroneal tendonitis, surgical intervention7Grimsrud, C. (n.d.). Peroneal Tendonitis. CU Orthopedics – Foot & Ankle. https://medschool.cuanschutz.edu/docs/librariesprovider65/courtney-grimsrud/patient-handouts/peroneal-tendonitis.pdf?sfvrsn=388192ba_2 may become necessary. The following options can be considered:
Synovectomy:
The surgical procedure, known as a synovectomy, involves removing damaged outer tissue layers surrounding the peroneal tendons. This procedure aims to alleviate persistent symptoms, promote healing, and improve the overall condition of the peroneal tendons. In case of a ruptured tendon, the foot and ankle surgeon might perform a tendon repair surgery.
Ankle arthroscopy:
Patients with peroneal tendonitis may also have problems within the ankle joint itself. In this situation, an ankle arthroscopy may be indicated.’Ankle arthroscopy is a minimally invasive surgical technique involving a tiny camera and specialized instruments to diagnose and treat various conditions affecting the ankle joint. During the procedure, the surgeon can directly visualize the joint’s internal structures, including the cartilage, ligaments, and synovium, to assess any abnormalities, such as loose fragments or damaged tissues.
Ankle Ligament Stabilization:
Many patients with significant peroneal tendonitis requiring surgery may also have ankle instability. They may require a lateral ankle ligament stabilization, such as a Brostrum procedure, in addition to the procedures on the peroneal tendons. The Brostrum procedure is a surgical technique employed to address lateral ankle instability by repairing or reconstructing the damaged ligaments that support the outer aspect of the ankle. When patients present with both peroneal tendonitis and ankle instability, healthcare providers may recommend a combined approach.
Peroneal Tendonitis Exercises
To treat peroneal tendonitis, you can do some simple exercises. Start slow and gradually increase the hardness of the exercise. However, stop if you have pain or other symptoms.
Towel Stretch
- Take a towel, sit on the ground, and extend your feet outwards
- Wrap the towel around the toes and pull it backward
- The foot and the lower leg become stretched
- Resume the stretch for 30-60 seconds
- Repeat the stretch for the second leg
- Do this exercise 2-3 times a day
Standing Calf Stretch
- Stand against a rigid wall and place your palms on it at a level slightly above your shoulders.
- Assume a split position with feet pointing towards the wall, and keep the back leg straight.
- Slightly bend and move the front leg so that the lower part of the back leg stretches.
- Continue this position for almost 30 seconds.
- If you do not feel the stretch in the back leg, bend it slightly and repeat the same exercise.
- Repeat the exercise 2-3 times a day
Heel Raises
- Stand at the back of a table or a chair.
- Hold it and rise on your toes
- Assume this position for 5-10 seconds
- Leave the support and lower your heels. Nevertheless, you can hold the support while lowering the heels.
- Repeat the exercise 5-20 times
Plantar Fascia Stretch
- Sit on a chair
- Roll a tennis ball backward and forward under your foot for one minute and repeat the process for the other foot.
- Now, cross your legs and pull the big toe of the crossed leg towards your body.
- Do this for 30-45 seconds and repeat the exercise by switching legs
- Do this exercise 2-3 times a day
Ankle Flexion
- Sit straight on the floor. Hold a resistance band around the ball of the foot bone and stretch your leg forward.
- Point the toes of the extended leg away from your body, and then slightly bend the ankle by drawing the toes towards the shin.
- Repeat this ten times, and then do the same stretch for the other leg.
Peroneal Tendonitis Prognosis
The symptoms of peroneal tendonitis go away after three months in most people if they follow the recommended therapy.8NHS Lanarkshire Peroneal tendinopathy, NHS choices. Retrieved 22 August 2023 from https://www.nhslanarkshire.scot.nhs.uk/services/physiotherapy-msk/peroneal-tendinopathy/ However, in some cases, it may take a year to alleviate the symptoms completely. Recovery from peroneal tendonitis following surgery can be longer. Proper physiotherapy after surgery speeds recovery and helps regain ankle stability.
How to Prevent Peroneal Tendonitis?
Take some simple measures to avoid an injury to the peroneal tendon:
- Stretch your peroneal, ankle, and calf muscles regularly
- Maintain an appropriate form and posture while doing exercises that involve ankle and peroneal muscles
- Gradually increase the strength of weight-bearing exercises
- Take appropriate rest in between exercises and running
Final Words
Peroneal tendonitis is the inflammation of peroneal tendons due to overworking of tendons. The condition may seem trivial, but if left untreated, it may worsen and lead to tendon rupture. Take conservative treatment for a few weeks after injury and undergo surgery if you don’t recover. Take appropriate precautionary measures to avoid tendinopathy.
Refrences
- 1Morrison, W. (ed.) (2017) Peroneal tendonitis: Causes, treatment, and recovery, Medical News Today. Retrieved 22 August 2023 from https://www.medicalnewstoday.com/articles/318349#Symptoms
- 2Davda K, Malhotra K, O’Donnell P, Singh D, Cullen N. Peroneal tendon disorders. EFORT Open Rev. 2017 Jun 22;2(6):281-292. Doi: 10.1302/2058-5241.2.160047. PMID: 28736620; PMCID: PMC5508858.
- 3Mulcahy, J.A. (2019) GUIDE: Physical therapy guide to peroneal tendinopathy, Choose PT. Retrieved 22 August 2023 https://www.choosept.com/guide/physical-therapy-guide-peroneal-tendinopathy#:~:text=Your%20physical%20therapist%20may%20use,Range%2Dof%2Dmotion%20exercises
- 4Walt, J. and Massey, P. (2023) Peroneal tendon syndromes – statpearls – NCBI bookshelf, Stat Pearls [Internet]. Retrieved 22 August 2023 https://www.ncbi.nlm.nih.gov/books/NBK544354/
- 5Morrison, W. (ed.) (2018) Peroneal tendonitis: Causes, treatment, and recovery, Medical News Today. Retrieved 23 August 2023 from https://www.medicalnewstoday.com/articles/318349
- 6Dallaudière B; Pesquer L; Meyer P; Silvestre A; Perozziello A; Peuchant A; Durieux MH; Loriaut P; Hummel V; Boyer P; Schouman-Claeys E; Serfaty JM; B. (2014) intratendinous injection of platelet-rich plasma under US guidance to treat tendinopathy: A long-term pilot study, Journal of vascular and interventional radiology : JVIR. Retrieved 23 August 2023 from https://pubmed.ncbi.nlm.nih.gov/24656590/
- 7Grimsrud, C. (n.d.). Peroneal Tendonitis. CU Orthopedics – Foot & Ankle. https://medschool.cuanschutz.edu/docs/librariesprovider65/courtney-grimsrud/patient-handouts/peroneal-tendonitis.pdf?sfvrsn=388192ba_2
- 8NHS Lanarkshire Peroneal tendinopathy, NHS choices. Retrieved 22 August 2023 from https://www.nhslanarkshire.scot.nhs.uk/services/physiotherapy-msk/peroneal-tendinopathy/

