Silicosis is a fibrotic lung disease caused by the inhalation of fine crystalline silica (silicon dioxide) particles. It primarily develops after significant occupational exposure to respirable crystalline silica (RCS), commonly found in certain industries such as mining, construction, and sandblasting. Silicosis has a long latency period. It clinically presents as an acute, accelerated, and sometimes chronic disease.1Finder, P.M., Michael I. Greenberg, MD, MPH, Javier Waksman, MD, and John Curtis, MD. Impairment of lung function increases with the progression of the disease. Some other conditions associated with silica dust exposure are lung cancer, airway obstruction, and mycobacterial diseases. Yet, there is no proper curative treatment. Comprehensive management strategies can help in improving the life expectancy of the patients. Silicosis is a potentially fatal and irreversible disease.2Leung, C.C., I.T.S. Yu, and W. Chen, Silicosis. The Lancet, 2012. 379(9830): p. 2008-2018.
Causes of Silicosis
Silica is a naturally occurring mineral. It is usually present in sand, soil, and rocks. When these substances are ground, cut, and drilled, tiny particles of silica get released into the surrounding air. Inhalation of these particles causes damage to lung tissue over time, resulting in fibrosis. Silica is also used in the manufacturing of glass, ceramics, cosmetics, processed foods, and agricultural products.
Silicosis is not infectious and cannot be spread from person to person. It most commonly affects individuals exposed to silica dust in occupational settings. Jobs with a high risk of silica exposure include:
- Construction
- Mining
- Glass manufacturing
- Sandblasting
- Farming
- Roofing
- Road repair
- Steel industry
- Masonry
Silicosis is a prominent international health issue. Silicosis occurs everywhere. It is especially prevalent in low and middle-income countries where the disease burden is often under-reported due to poor surveillance.

Types of Silicosis
The three types of silicosis are:
Acute Silicosis:
Acute silicosis is also known as silicoproteinosis. It is a rare condition. Patients with high-intensity respirable crystalline silica (RCS) exposure usually get this condition. It presents within a few weeks to less than five years after the exposure of RCS. It is more commonly seen in occupations like sandblasting and tunneling. The hallmark pathology of acute silicosis is alveolar proteinosis, in which the alveoli fill with proteinaceous material, severely impairing gas exchange.3Hoy, R.F. and D.C. Chambers, Silica‐related diseases in the modern world. Allergy, 2020. 75(11): p. 2805-2817.
Accelerated Silicosis:
Accelerated silicosis develops within 5 to 10 years of RCS exposure. Its disease progression is more rapid than the chronic form of silicosis. The features of this type overlap with both chronic and acute types. There is evidence of silicotic nodules in patients with accelerated silicosis. However, pulmonary nodules in this condition intensify more quickly.4Adamcakova, J. and D. Mokra, New insights into pathomechanisms and treatment possibilities for lung silicosis. International journal of molecular sciences, 2021. 22(8): p. 4162.
Chronic Silicosis:
This is the most common form, usually developing after 10 to 30 years of prolonged exposure to lower concentrations of RCS. It progresses slowly and is further subdivided into two types based on radiographic features:
Simple Chronic Silicosis
This type of silicosis is also known as nodular silicosis. It is characterized by multiple small (<10 mm) nodules, primarily in the upper lung zones. Although it may remain stable for years, it can progress to a more severe form.
Complicated Chronic silicosis
It is also known as pulmonary massive fibrosis (PMF). The pulmonary nodules expand and fuse to form conglomerate masses. The diameter of these masses is greater than 10mm. The lung tissue undergoes extensive damage, resulting in severe respiratory impairment, reduced diffusion capacity, pulmonary hypertension, and cor pulmonale (a condition where the right side of the heart fails due to high pressure in the lung arteries, often caused by chronic lung diseases like silicosis).5Champlin, J., R. Edwards, and S. Pipavath, Imaging of occupational lung disease. Radiologic Clinics, 2016. 54(6): p. 1077-1096.
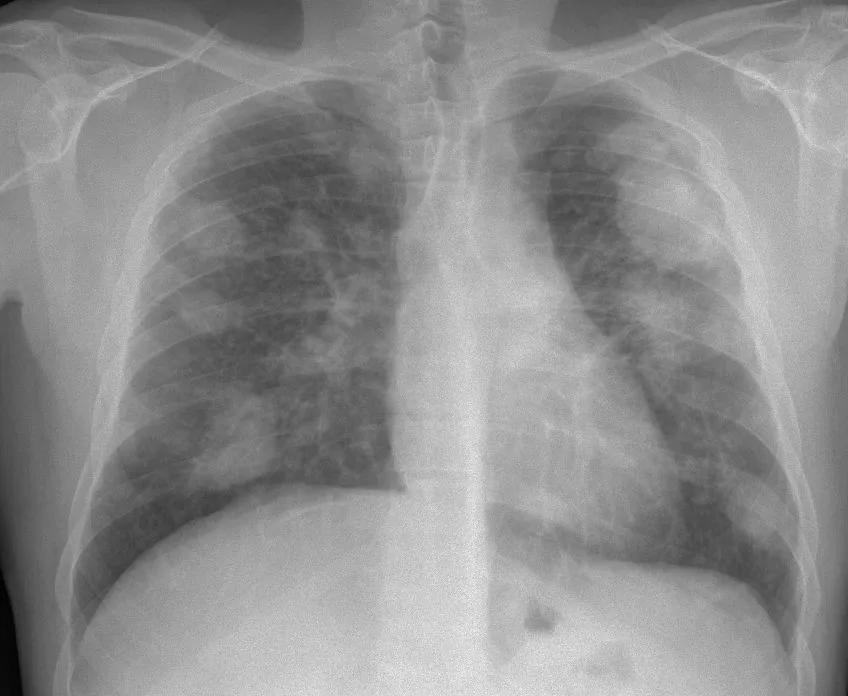
Image Courtesy: Wikimedia Commons by Gumersindorego, licensed under CC BY-SA 3.0. No changes were made to the original image.
Symptoms of Silicosis
Silicosis presents several symptoms. The most common symptoms include;
- Shortness of breath (Dyspnea)
- Weakness
- Fatigue
- Weight loss
- Chest pain
- Swollen legs (Peripheral Edema)
- Sudden fever
- Cyanosis
- Persistent coughing
- Inflammation
- Cough with sputum
- Pulmonary Fibrosis
- Scarring of Lung Tissue
The pulmonary and systemic symptoms that are specific to acute silicosis are:
- Coughs
- Weight loss
- Fever
- Pleurisy
- Fatigue
- Dyspnea
- Hypoxia6Krefft, S., J. Wolff, and C. Rose, Silicosis: an update and guide for clinicians. Clinics in Chest Medicine, 2020. 41(4): p. 709-722.
Patients with chronic or accelerated silicosis reveal lymphadenopathy. Patients suffering from simple chronic silicosis are generally asymptomatic. They can present a dry cough and dyspnea on exertion.7Krefft, S., J. Wolff, and C. Rose, Silicosis: an update and guide for clinicians. Clinics in Chest Medicine, 2020. 41(4): p. 709-722.
Diagnosis of Silicosis
The diagnosis of silicosis relies on a history of exposure to silica dust and compatible radiological features.8Hamilton Jr, R.F., S.A. Thakur, and A. Holian, Silica binding and toxicity in alveolar macrophages. Free Radical Biology and Medicine, 2008. 44(7): p. 1246-1258.
Physical Examination & History:
A thorough occupational history is crucial, focusing on prolonged or repeated exposure to silica dust. A physical exam may reveal abnormal lung sounds (crackles) and signs of chronic respiratory insufficiency.
Imaging Tests:
Chest radiography may show small, rounded nodules predominantly in the upper lung zones. Hilar and mediastinal lymph node enlargement can also be seen.9Tan, S. and S. Chen, The mechanism and effect of autophagy, apoptosis, and pyroptosis on the progression of silicosis. International journal of molecular sciences, 2021. 22(15): p. 8110. High-resolution computerized tomography (HRCT) can help diagnose the early stages of scoliosis. It is more sensitive and offers diagnostic confidence by providing detailed images of the lungs. The radiographic features that HRCT reveals in scoliosis are:
- Numerous bilateral centrilobular nodular and ground glass opacities.
- The images show a “crazy-paving” pattern due to septal thickening and alveolar filling.10Champlin, J., R. Edwards, and S. Pipavath, Imaging of occupational lung disease. Radiologic Clinics, 2016. 54(6): p. 1077-1096.
Lung Function Tests:
The pulmonary function in silicosis patients varies depending on the stage of the disease. Usually, the lung function remains unaffected during the early stages of the disease.11Adamcakova, J. and D. Mokra, New insights into pathomechanisms and treatment possibilities for lung silicosis. International journal of molecular sciences, 2021. 22(8): p. 4162.
The common lung function tests for assessing the condition are:
Spirometry
It measures the amount of air you can breathe in and out. It is normal in the early stages of silicosis. Both obstructive and destructive patterns are observed in simple silicosis. However, obstruction patterns are more common.12Leung, C.C., I.T.S. Yu, and W. Chen, Silicosis. The Lancet, 2012. 379(9830): p. 2008-2018.
Diffusion Capacity
Diffusion capacity is the measurement of how well oxygen gets into your blood. Reduced diffusion capacity can indicate early fibrotic changes. Decreased total lung capacity and compliance may appear in advanced silicosis.13Leung, C.C., I.T.S. Yu, and W. Chen, Silicosis. The Lancet, 2012. 379(9830): p. 2008-2018.
Invasive Diagnostic Methods:
The invasive investigation technique for diagnosing silicosis is lung biopsy. Additionally, bronchoalveolar lavage and bronchoscopy can also be helpful. These tests are ordered rarely.
Management & Treatment
Currently, there is no effective treatment for silicosis, as most interventions are supportive. The supportive interventions include:
- Pulmonary rehabilitation
- Prompt treatment of infection
- Administration of recommended vaccinations (E.g. Influenza and Pneumococcal)
- Supplemental oxygen in case of hypoxia.14Hamilton Jr, R.F., S.A. Thakur, and A. Holian, Silica binding and toxicity in alveolar macrophages. Free Radical Biology and Medicine, 2008. 44(7): p. 1246-1258.
The treatment modality for end-stage silicosis is a lung transplant. However, a lung transplant is a very expensive treatment, and it carries a significant amount of risk. An advanced understanding of the pathophysiology of silicosis is opening doors toward the targeted treatment, such as anti-cytokine and anti-fibrotic therapy. However, no large randomized controlled trials have assessed the safety and efficacy of such drugs to hold the treatment option title for scoliosis.15Adamcakova, J. and D. Mokra, New insights into pathomechanisms and treatment possibilities for lung silicosis. International journal of molecular sciences, 2021. 22(8): p. 4162.
Prevention
Although silicosis is currently untreatable, it is preventable. Primary prevention via controlling the RCS exposure is critical in preventing silicosis.16Krefft, S., J. Wolff, and C. Rose, Silicosis: an update and guide for clinicians. Clinics in Chest Medicine, 2020. 41(4): p. 709-722. Prevention strategies include:
- Reducing or eliminating exposure to RCS through engineering controls (ventilation, wet methods).
- Use personal protective equipment if you work in risk occupational areas or change your job.
- Use supplemental oxygen while working in risky areas if required.
- Avoiding tobacco use to prevent compounding lung damage.
- If your work puts you at high risk of getting the disease, ensure regular screening.
- Early detection can help in preventing the severity of the disease.
- Counseling patients to avoid further exposure to silica can lower the chance of getting the severe form of the disease.
Some other methods of preventing silicosis at your workplace are:
- Wash your hands and face before eating at your workplace.
- Avoid drinking or eating near the silica dust areas.
- Use respirators to avoid inhaling silica at your workplace.
- Ensure proper ventilation and use blasting cabinets while working.
- Switch to wet methods for cutting, chipping, or grinding materials.
- Take a shower and change your clothes after work.
Differential Diagnosis
The radiographic opacities of patients with silicosis can resemble some other pulmonary diseases. These diseases include:
- Malignancy
- Tuberculosis
- Sarcoidosis17Champlin, J., R. Edwards, and S. Pipavath, Imaging of occupational lung disease. Radiologic Clinics, 2016. 54(6): p. 1077-1096.
Additionally, microscopic evaluation of the biopsied nodules from patients with silicosis can present acellular whorls of hyaline collagen.
Prognosis
The prognosis of the disease is poor. It leads to a gradual worsening decline in the pulmonary function of the patients. The disease can lead to the eventual development of respiratory failure. Infection with tubercular or non-tubercular Mycobacteria is common. Pumorny damage and pulmonary inflammation can progress even after the cessation of silica exposure.
Complications
Prolonged exposure to respirable crystalline silica (RCS) is associated with an increased risk of developing all histologic types of lung cancer. The progressive changes of silicosis can mimic or obscure early signs of malignancy, complicating early cancer detection. In animal models, silica-related inflammation appears to promote tumor growth.18Hoy, R.F. and D.C. Chambers, Silica‐related diseases in the modern world. Allergy, 2020. 75(11): p. 2805-2817. Tuberculosis is another important complication of the silicosis. Although the exact mechanism is not well understood, there is evidence that supports that silica exposure can be linked with the development of certain autoimmune disorders. These include:
- Rheumatoid arthritis
- Glomerulonephritis
- Scleroderma or systemic sclerosis
- Systemic lupus erythematosus19Hamilton Jr, R.F., S.A. Thakur, and A. Holian, Silica binding and toxicity in alveolar macrophages. Free Radical Biology and Medicine, 2008. 44(7): p. 1246-1258.
Silicosis vs. Asbestosis
Both asbestosis and silicosis are the two common types of non-malignant lung diseases. They have the same pathogenesis and incurable nature. The main cause of both disorders is inhaling hazardous dust in various workplaces.20Mapa, M.S. and R.S.H. Koralege, Silicosis, and Asbestosis. Medical Geology: En route to One Health, 2023: p. 83-94.
The key differences between these two diseases are:
| Feature | Silicosis | Asbestosis |
|---|---|---|
| Causative Agent | Crystalline silica | Asbestos fibers |
| Affected Lung Area | Upper lobes with nodular pattern | Lower lobes with pleural involvement |
| Latency Period | Typically shorter | Usually longer |
| Radiological Markers | Nodules and progressive massive fibrosis (PMF) | Pleural plaques and lower lobe fibrosis |
A Quick Review
Scoliosis is a devastating and incurable disease. An irreversible lung scarring marks the condition. Fibrosis is a progressive disease and often leads to a fatal restrictive lung function. Now, there is plenty of knowledge on scoliosis and its causes and detrimental effects. But, millions of workers worldwide continue to endure exposure to the hazardous levels of RCS. Elimination of this preventable disease with the conjoined effort of industry employers, medical professionals, and the public health system.
Refrences
- 1Finder, P.M., Michael I. Greenberg, MD, MPH, Javier Waksman, MD, and John Curtis, MD.
- 2Leung, C.C., I.T.S. Yu, and W. Chen, Silicosis. The Lancet, 2012. 379(9830): p. 2008-2018.
- 3Hoy, R.F. and D.C. Chambers, Silica‐related diseases in the modern world. Allergy, 2020. 75(11): p. 2805-2817.
- 4Adamcakova, J. and D. Mokra, New insights into pathomechanisms and treatment possibilities for lung silicosis. International journal of molecular sciences, 2021. 22(8): p. 4162.
- 5Champlin, J., R. Edwards, and S. Pipavath, Imaging of occupational lung disease. Radiologic Clinics, 2016. 54(6): p. 1077-1096.
- 6Krefft, S., J. Wolff, and C. Rose, Silicosis: an update and guide for clinicians. Clinics in Chest Medicine, 2020. 41(4): p. 709-722.
- 7Krefft, S., J. Wolff, and C. Rose, Silicosis: an update and guide for clinicians. Clinics in Chest Medicine, 2020. 41(4): p. 709-722.
- 8Hamilton Jr, R.F., S.A. Thakur, and A. Holian, Silica binding and toxicity in alveolar macrophages. Free Radical Biology and Medicine, 2008. 44(7): p. 1246-1258.
- 9Tan, S. and S. Chen, The mechanism and effect of autophagy, apoptosis, and pyroptosis on the progression of silicosis. International journal of molecular sciences, 2021. 22(15): p. 8110.
- 10Champlin, J., R. Edwards, and S. Pipavath, Imaging of occupational lung disease. Radiologic Clinics, 2016. 54(6): p. 1077-1096.
- 11Adamcakova, J. and D. Mokra, New insights into pathomechanisms and treatment possibilities for lung silicosis. International journal of molecular sciences, 2021. 22(8): p. 4162.
- 12Leung, C.C., I.T.S. Yu, and W. Chen, Silicosis. The Lancet, 2012. 379(9830): p. 2008-2018.
- 13Leung, C.C., I.T.S. Yu, and W. Chen, Silicosis. The Lancet, 2012. 379(9830): p. 2008-2018.
- 14Hamilton Jr, R.F., S.A. Thakur, and A. Holian, Silica binding and toxicity in alveolar macrophages. Free Radical Biology and Medicine, 2008. 44(7): p. 1246-1258.
- 15Adamcakova, J. and D. Mokra, New insights into pathomechanisms and treatment possibilities for lung silicosis. International journal of molecular sciences, 2021. 22(8): p. 4162.
- 16Krefft, S., J. Wolff, and C. Rose, Silicosis: an update and guide for clinicians. Clinics in Chest Medicine, 2020. 41(4): p. 709-722.
- 17Champlin, J., R. Edwards, and S. Pipavath, Imaging of occupational lung disease. Radiologic Clinics, 2016. 54(6): p. 1077-1096.
- 18Hoy, R.F. and D.C. Chambers, Silica‐related diseases in the modern world. Allergy, 2020. 75(11): p. 2805-2817.
- 19Hamilton Jr, R.F., S.A. Thakur, and A. Holian, Silica binding and toxicity in alveolar macrophages. Free Radical Biology and Medicine, 2008. 44(7): p. 1246-1258.
- 20Mapa, M.S. and R.S.H. Koralege, Silicosis, and Asbestosis. Medical Geology: En route to One Health, 2023: p. 83-94.

